Abstract
Purpose
One of the concerns regarding surgical treatment of the obstructive sleep apnea syndrome (OSAS) has been the possibility that these patients may experience a higher rate of perioperative complications, which could be aggravated by the upper airway edema caused by surgical trauma. The purpose of this study was to evaluate the immediate impact of pharyngeal surgery on the respiratory parameters of adult patients with OSAS.
Methods
Twenty-three adults with moderate to severe OSAS and indications for pharyngeal surgery (with or without nasal surgery) were consecutively selected. The subjects underwent surgical treatment and monitoring of sleep parameters preoperatively (by type I polysomnography, PSG) and in the immediate postoperative period (arterial tonometry).
Results
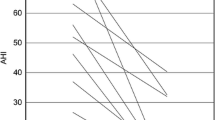
Twenty-two subjects, aged 20 to 59 years (mean ± SD, 38.0 ± 12.1 years), were included in the study. Nineteen (86.4%) were male. The mean apnea-hypopnea index (AHI) was 59.3 ± 26.0 events/h. Comparison between preoperative PSG and postoperative arterial tonometry revealed statistically significant reductions in AHI (p = 0.03), respiratory disturbance index (RDI) (p = 0.05), and oxygen desaturation index (p = 0.001), as well as increases in nadir oxyhemoglobin saturation (p = 0.003) and percentage of REM sleep (p = 0.01).
Conclusions
In this sample of patients with moderate and severe OSAS who underwent pharyngeal surgery, the vast majority of patients did not exhibit any deterioration of respiratory parameters in the immediate postoperative period. Conversely, there was a significant improvement in the parameters.




Similar content being viewed by others
References
Marin JM, Carrizo SJ, Vicente E, Agusti AGN (2005) Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 365(9464):1046–1053
Butt M, Dwivedi G, Khair O, Lip GYH (2010) Obstructive sleep apnea and cardiovascular disease. Int J Cardiol 139(1):7–16
George CF, Smiley A (1999) Sleep apnea & automobile crashes. Sleep 22(6):790–795
Lindberg EVA, Carter NED, Gislason T, Janson C (2001) Role of snoring and daytime sleepiness in occupational accidents. Am J Respir Crit Care Med 164(11):2031–2035
Kushida CA, Littner MR, Hirshkowitz M, Morgenthaler TI, Alessi CA, Bailey D, Boehlecke B, Brown TM, Coleman J Jr, Friedman L, Kapen S, Kapur VK, Kramer M, Lee-Chiong T, Owens J, Pancer JP, Swick TJ, Wise MS (2006) Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep 29(3):375–380
Vasu TS, Grewal R, Doghramji K (2012) Obstructive sleep apnea syndrome and perioperative complications: a systematic review of the literature. J Clin Sleep Med 8(2):199–207
Chung F, Memtsoudis SG, Ramachandran SK, Nagappa M, Opperer M, Cozowicz C, Patrawala S, Lam D, Kumar A, Joshi GP, Fleetham J, Ayas N, Collop N, Doufas AG, Eikermann M, Englesakis M, Gali B, Gay P, Hernandez AV, Kaw R, Kezirian EJ, Malhotra A, Mokhlesi B, Parthasarathy S, Stierer T, Wappler F, Hillman DR, Auckley D (2016) Society of Anesthesia and Sleep Medicine Guidelines on preoperative screening and assessment of adult patients with obstructive sleep apnea. Anesth Analg 123(2):452–473
American Academy of Sleep Medicine (2014) International classification of sleep disorders: diagnostic and coding manual. 3nd edition. Diagn Coding Manual 281:2313
Brodsky L (1989) Modern assessment of tonsils and adenoids. Pediatr Clin N Am 36(6):1551–1569
Ferber R, Millman R, Coppola M, Fleetham J, Murray CF, Iber C, McCall WV, Nino-Murcia G, Pressman M, Sanders M, Strohl K, Votteri B, Williams A (1994) Portable recording in the assessment of obstructive sleep apnea. {ASDA} standards of practice. Sleep 17(4):378–392
Pang KP, Gourin CG, Terris DJ (2007) A comparison of polysomnography and the WatchPAT in the diagnosis of obstructive sleep apnea. Otolaryngol - Head Neck Surg 137(4):665–668
Choi JH, Kim EJ, Kim YS, Choi J, Kim TH, Kwon SY, Lee HM, Lee SH, Shin C, Lee SH (2010) Validation study of portable device for the diagnosis of obstructive sleep apnea according to the new AASM scoring criteria: Watch-PAT 100. Acta Otolaryngol 130(7):838–843
Hedner J, White DP, Malhotra A, Herscovici S, Pittman SD, Zou D et al (2011) Sleep staging based on autonomic signals: a multi-center validation study. J Clin Sleep Med 7(3):301–306
Vidigal TA, Haddad FL, Cabral RF, Oliveira MC, Cavalcante RR, Bittencourt LR et al (2014) New clinical staging for pharyngeal surgery in obstructive sleep apnea patients. Braz J Otorhinolaryngol 80(6):490–496
Friedman M, Tanyeri H, La Rosa M, Landsberg R, Vaidyanathan K, Pieri S et al (1999) Clinical predictors of obstructive sleep apnea. Laryngoscope 109:1–10
Friedman M, Ibrahim H, Bass L (2002) Clinical staging for sleep-disordered breathing. Otolaryngol Head Neck Surg 127:13–21
Fassbender P, Herbstreit F, Eikermann M, Teschler H, Peters J (2016) Obstructive sleep apnea-perioperative risk factor. Dtsch Arztebl Int 113(27–28):463–469
Maurer J, Juncker C, Dworschak M, Hormann K (1997) Paraoperative change of sleep-disordered breathing in healthy snorers and sleep apnea patients compared to preoperative values. Sleep Breath 2(2):50–55
Sanders MH, Costantino JP, Johnson JT (1990) Polysomnography early after uvulopalatopharyngoplasty as a predictor of late postoperative results. Chest 97(4):913–919
Mickelson SA, Hakim I (1998) Is postoperative intensive care monitoring necessary after uvulopalatopharyngoplasty? Otolaryngol - Head Neck Surg 119(4):352–356
Kim JA, Lee JJ, Jung HH (2005) Predictive factors of immediate postoperative complications after uvulopalatopharyngoplasty. Laryngoscope 115(10):1837–1840
Esclamado RM, Glenn MG, McCulloch TM, Cummings CW (1989) Perioperative complications and risk factors in the surgical treatment of obstructive sleep apnea syndrome. Laryngoscope 99(11):1125–1129
Haavisto L, Suonpaa J (1994) Complications of uvulopalatopharyngoplasty. Clin Otolaryngol Allied Sci 19(3):243–247
Terris DJ, Fincher EF, Hanasono MM, Fee WE, Adachi K (1998) Conservation of resources: indications for intensive care monitoring after upper airway surgery on patients with obstructive sleep apnea. Laryngoscope 108(6):784–788
Hathaway B, Johnson JT (2006) Safety of uvulopalatopharyngoplasty as outpatient surgery. Otolaryngol - Head Neck Surg 134(4):542–544
Kandasamy T, Wright ED, Fuller J, Rotenberg BW (2013) The incidence of early post-operative complications following uvulopalatopharyngoplasty: identification of predictive risk factors. J Otolaryngol - Head Neck Surg 42(1):15
Brenner MJ, Goldman JL (2014) Obstructive sleep apnea and surgery: quality improvement imperatives and opportunities. Curr Otorhinolaryngol Rep 2(1):20–29
Ayas NT, Pittman S, MacDonald M, White DP (2003) Assessment of a wrist-worn device in the detection of obstructive sleep apnea. Sleep Med 4(5):435–442
Bar A, Pillar G, Dvir I, Sheffy J, Schnall RP, Lavie P (2003) Evaluation of a portable device based on peripheral arterial tone for unattended home sleep studies. Chest 123(3):695–703
Körkuyu E, Düzlü M, Karamert R, Tutar H, Yılmaz M, Çiftçi B, Güven SF (2015) The efficacy of Watch PAT in obstructive sleep apnea syndrome diagnosis. Eur Arch Otorhinolaryngol 272(1):111–116
Souza FJFB, Genta PR, Souza Filho AJS, Wellman A, Lorenzi-Filho G (2017) The influence of head-of-bed elevation in patients with obstructive sleep apnea. Sleep Breath 21(4):815–820
Funding
This study was funded by CAPES–Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (grant number USD$26000.00). Lia Bittencourt and Sergio Tufik have received grants from CNPq - Conselho Nacional de Desenvolvimento Científico e Tecnológico. Material support was provided by Politec Saúde (Watch-PAT 200, Itamar Medical Ltd., Israel) and by AFIP–Associação Fundo de Incentivo à Pesquisa (Polysomnography exams).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study protocol was approved by the institutional Research Ethics Committee with opinion no. 192,034.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This study was performed at the Universidade Federal de São Paulo, Brazil.
Rights and permissions
About this article
Cite this article
Stefanini, R., Caparroz, F., Sguillar, D.A. et al. Immediate impact of pharyngeal surgery on respiratory parameters in adults with obstructive sleep apnea. Sleep Breath 24, 505–511 (2020). https://doi.org/10.1007/s11325-019-01888-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-019-01888-2