Abstract
Purpose
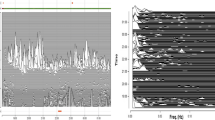
Despite the increasing number of research studies of cardiopulmonary coupling (CPC) analysis, an electrocardiogram-based technique, the use of CPC in underserved population remains underexplored. This study aimed to first evaluate the reliability of CPC analysis for the detection of obstructive sleep apnea (OSA) by comparing with polysomnography (PSG)-derived sleep outcomes.
Methods
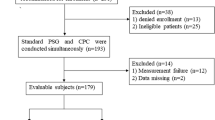
Two hundred five PSG data (149 males, age 46.8 ± 12.8 years) were used for the evaluation of CPC regarding the detection of OSA. Automated CPC analyses were based on ECG signals only. Respiratory event index (REI) derived from CPC and apnea–hypopnea index (AHI) derived from PSG were compared for agreement tests.
Results
CPC-REI positively correlated with PSG-AHI (r = 0.851, p < 0.001). After adjusting for age and gender, CPC-REI and PSG-AHI were still significantly correlated (r = 0.840, p < 0.001). The overall results of sensitivity and specificity of CPC-REI were good.
Conclusion
Compared with the gold standard PSG, CPC approach yielded acceptable results among OSA patients. ECG recording can be used for the screening or diagnosis of OSA in the general population.



Similar content being viewed by others
Abbreviations
- AASM:
-
American Academy of Sleep Medicine
- AHI:
-
apnea–hypopnea index
- AUC:
-
area under the curve
- CPC:
-
cardiopulmonary coupling
- e-LFC:
-
elevated low-frequency coupling
- ECG:
-
electrocardiogram
- EEG:
-
electroencephalography
- FDA:
-
Food and Drug Administration
- HFC:
-
high-frequency coupling
- HRV:
-
heart-rate variability
- IRB:
-
Institutional Review Board
- LFC:
-
low-frequency coupling
- LR:
-
likelihood ratio
- NPV:
-
negative predictive value
- OCST:
-
out of center sleep testing
- OSA:
-
obstructive sleep apnea
- PPV:
-
positive predictive value
- PSG:
-
polysomnography
- REI:
-
respiratory event index
- ROC:
-
receiver operating characteristic
- RPSGT:
-
registered polysomnographic technologists
- SD:
-
standard deviation
- SDB:
-
sleep-disordered breathing
- TIB:
-
time in bed
- TST:
-
total sleep time
- VLFC:
-
very-low-frequency coupling
References
Senaratna CV, Perret JL, Lodge CJ, Lowe AJ, Campbell BE, Matheson MC, Hamilton GS, Dharmage SC (2016) Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev 34:70–81. https://doi.org/10.1016/j.smrv.2016.07.002
Ma Y, Sun S, Peng CK, Fang Y, Thomas RJ (2017) Ambulatory blood pressure monitoring in Chinese patients with obstructive sleep apnea. J Clin Sleep Med 13(3):433–439. https://doi.org/10.5664/jcsm.6498
Collop NA, Anderson WM, Boehlecke B, Claman D, Goldberg R, Gottlieb DJ, Hudgel D, Sateia M, Schwab R (2007) Clinical guidelines for the use of unattended portable monitors in the diagnosis of obstructive sleep apnea in adult patients. Portable Monitoring Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med 3(7):737–747
Collop NA, Tracy SL, Kapur V, Mehra R, Kuhlmann D, Fleishman SA, Ojile JM (2011) Obstructive sleep apnea devices for out-of-center (OOC) testing: technology evaluation. J Clin Sleep Med 7(5):531–548. https://doi.org/10.5664/jcsm.1328
Yuceege M, Firat H, Demir A, Ardic S (2013) Reliability of the Watch-PAT 200 in detecting sleep apnea in highway bus drivers. J Clin Sleep Med 9(4):339–344. https://doi.org/10.5664/jcsm.2584
Korkuyu E, Duzlu M, Karamert R, Tutar H, Yilmaz M, Ciftci B, Guven SF (2015) The efficacy of Watch PAT in obstructive sleep apnea syndrome diagnosis. Eur Arch Otorhinolaryngol 272(1):111–116. https://doi.org/10.1007/s00405-014-3097-0
Choi JH, Lee B, Lee JY, Kim HJ (2018) Validating the Watch-PAT for diagnosing obstructive sleep apnea in adolescents. J Clin Sleep Med 14(10):1741–1747. https://doi.org/10.5664/jcsm.7386
Gehring J, Gesche H, Drewniok G, Kuchler G, Patzak A (2018) Nocturnal blood pressure fluctuations measured by using pulse transit time in patients with severe obstructive sleep apnea syndrome. Sleep Breath 22(2):337–343. https://doi.org/10.1007/s11325-017-1555-9
Li Y, Gao H, Ma Y (2017) Evaluation of pulse oximeter derived photoplethysmographic signals for obstructive sleep apnea diagnosis. Medicine 96(18):e6755. https://doi.org/10.1097/md.0000000000006755
Morgenthaler T, Alessi C, Friedman L, Owens J, Kapur V, Boehlecke B, Brown T, Chesson A Jr, Coleman J, Lee-Chiong T, Pancer J, Swick TJ (2007) Practice parameters for the use of actigraphy in the assessment of sleep and sleep disorders: an update for 2007. Sleep 30(4):519–529
Dumont M, Jurysta F, Lanquart JP, Migeotte PF, van de Borne P, Linkowski P (2004) Interdependency between heart rate variability and sleep EEG: linear/non-linear? Clin Neurophysiol 115(9):2031–2040. https://doi.org/10.1016/j.clinph.2004.04.007
Penzel T, Kantelhardt JW, Bartsch RP, Riedl M, Kraemer JF, Wessel N, Garcia C, Glos M, Fietze I, Schöbel C (2016) Modulations of heart rate, ECG, and cardio-respiratory coupling observed in polysomnography. Front Physiol 7:460–460. https://doi.org/10.3389/fphys.2016.00460
Stein PK, Pu Y (2012) Heart rate variability, sleep and sleep disorders. Sleep Med Rev 16(1):47–66. https://doi.org/10.1016/j.smrv.2011.02.005
Hill LK, Siebenbrock A (2009) Are all measures created equal? Heart rate variability and respiration - biomed 2009. Biomed Sci Instrum 45:71–76
Billman GE (2011) Heart rate variability - a historical perspective. Front Physiol 2:86. https://doi.org/10.3389/fphys.2011.00086
Shaffer F, McCraty R, Zerr CL (2014) A healthy heart is not a metronome: an integrative review of the heart’s anatomy and heart rate variability. Front Psychol 5:1040. https://doi.org/10.3389/fpsyg.2014.01040
Ma Y, McCraty R (2016) Heart rate variability in mind-body interventions. Complement Ther Med 29:A1–A2. https://doi.org/10.1016/j.ctim.2016.05.003
Ma Y, Tseng PH, Ahn A, Wu MS, Ho YL, Chen MF, Peng CK (2017) Cardiac autonomic alteration and metabolic syndrome: an ambulatory ECG-based study in a general population. Sci Rep 7:44363. https://doi.org/10.1038/srep44363
Ma Y, Wu CW, Peng CK, Ahn A, Bertisch SM, Lipsitz LA, Yeh GY, Manor B, Novak V, Hausdorff JM, Gow B, Wayne PM (2019) Complexity-based measures of heart rate dynamics in older adults following long- and short-term tai chi training: cross-sectional and randomized trial studies. Sci Rep 9(1):7500. https://doi.org/10.1038/s41598-019-43602-y
Thomas RJ, Mietus JE, Peng CK, Goldberger AL (2005) An electrocardiogram-based technique to assess cardiopulmonary coupling during sleep. Sleep 28(9):1151–1161
Magnusdottir S, Hilmisson H (2018) Ambulatory screening tool for sleep apnea: analyzing a single-lead electrocardiogram signal (ECG). Sleep Breath 22(2):421–429. https://doi.org/10.1007/s11325-017-1566-6
Hayano J, Watanabe E, Saito Y, Sasaki F, Fujimoto K, Nomiyama T, Kawai K, Kodama I, Sakakibara H (2011) Screening for obstructive sleep apnea by cyclic variation of heart rate. Circ Arrhythm Electrophysiol 4(1):64–72. https://doi.org/10.1161/circep.110.958009
Berry RB, Brooks R, Gamaldo CE et al (2016) The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. American Academy of Sleep Medicine, Illinois Version 2.3. Darien
American Academy of Sleep Medicine (2014) International classification of sleep disorders, 3rd edn. American Academy of Sleep Medicine, Darien
Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force (1999). Sleep 22 (5):667–689
Gupta MA, Simpson FC (2015) Obstructive sleep apnea and psychiatric disorders: a systematic review. J Clin Sleep Med 11(2):165–175. https://doi.org/10.5664/jcsm.4466
Guilleminault C, Connolly S, Winkle R, Melvin K, Tilkian A (1984) Cyclical variation of the heart rate in sleep apnoea syndrome. Mechanisms, and usefulness of 24 h electrocardiography as a screening technique. Lancet (London, England) 1(8369):126–131
Hilmisson H, Lange N, Duntley SP (2018) Sleep apnea detection: accuracy of using automated ECG analysis compared to manually scored polysomnography (apnea hypopnea index). In: Sleep & breathing = Schlaf & Atmung, vol 23, pp 125–133. https://doi.org/10.1007/s11325-018-1672-0
Harrington J, Schramm PJ, Davies CR, Lee-Chiong TL Jr (2013) An electrocardiogram-based analysis evaluating sleep quality in patients with obstructive sleep apnea. Sleep Breath 17(3):1071–1078. https://doi.org/10.1007/s11325-013-0804-9
Thomas RJ, Wood C, Bianchi MT (2018) Cardiopulmonary coupling spectrogram as an ambulatory clinical biomarker of sleep stability and quality in health, sleep apnea, and insomnia. Sleep 41(2):1–11. https://doi.org/10.1093/sleep/zsx196
Hilmisson H, Sveinsdottir E, Lange N, Magnusdottir S (2019) Insomnia symptoms in primary care: a prospective study focusing on prevalence of undiagnosed co-morbid sleep disordered breathing. Eur J Intern Med 63:19–26. https://doi.org/10.1016/j.ejim.2019.01.011
Schramm PJ, Thomas R, Feige B, Spiegelhalder K, Riemann D (2013) Quantitative measurement of sleep quality using cardiopulmonary coupling analysis: a retrospective comparison of individuals with and without primary insomnia. Sleep Breath 17(2):713–721. https://doi.org/10.1007/s11325-012-0747-6
Yang AC, Yang CH, Hong CJ, Tsai SJ, Kuo CH, Peng CK, Mietus JE, Goldberger AL, Thomas RJ (2011) Sleep state instabilities in major depressive disorder: detection and quantification with electrocardiogram-based cardiopulmonary coupling analysis. Psychophysiology 48(2):285–291. https://doi.org/10.1111/j.1469-8986.2010.01060.x
Schramm PJ, Poland RE, Rao U (2014) Bupropion response on sleep quality in patients with depression: implications for increased cardiovascular disease risk. Eur Neuropsychopharmacol 24(2):207–214. https://doi.org/10.1016/j.euroneuro.2013.09.007
Ma Y, Yeung A, Yang AC, Peng CK, Clain A, Alpert J, Fava M, Yeung AS (2018) The effects of tai chi on sleep quality in Chinese American patients with major depressive disorder: a pilot study. Behav Sleep Med 16(4):398–411. https://doi.org/10.1080/15402002.2016.1228643
Schramm PJ, Zobel I, Monch K, Schramm E, Michalak J (2016) Sleep quality changes in chronically depressed patients treated with mindfulness-based cognitive therapy or the cognitive behavioral analysis system of psychotherapy: a pilot study. Sleep Med 17:57–63. https://doi.org/10.1016/j.sleep.2015.09.022
Thomas RJ, Mietus JE, Peng CK, Goldberger AL, Crofford LJ, Chervin RD (2010) Impaired sleep quality in fibromyalgia: detection and quantification with ECG-based cardiopulmonary coupling spectrograms. Sleep Med 11(5):497–498. https://doi.org/10.1016/j.sleep.2009.09.003
Ibrahim LH, Jacono FJ, Patel SR, Thomas RJ, Larkin EK, Mietus JE, Peng CK, Goldberger AL, Redline S (2010) Heritability of abnormalities in cardiopulmonary coupling in sleep apnea: use of an electrocardiogram-based technique. Sleep 33(5):643–646
Thomas RJ, Mietus JE, Peng CK, Gilmartin G, Daly RW, Goldberger AL, Gottlieb DJ (2007) Differentiating obstructive from central and complex sleep apnea using an automated electrocardiogram-based method. Sleep 30(12):1756–1769
Schramm PJ, Thomas RJ (2012) Assessment of therapeutic options for mild obstructive sleep apnea using cardiopulmonary coupling measures. J Clin Sleep Med 8(3):315–320. https://doi.org/10.5664/jcsm.1924
Lee WH, Hong SN, Kim HJ, Rhee CS, Lee CH, Yoon IY, Kim JW (2016) A comparison of different success definitions in non-continuous positive airway pressure treatment for obstructive sleep apnea using cardiopulmonary coupling. J Clin Sleep Med 12(1):35–41. https://doi.org/10.5664/jcsm.5388
Choi JH, Thomas RJ, Suh SY, Park IH, Kim TH, Lee SH, Lee HM, Yun CH, Lee SH (2015) Sleep quality change after upper airway surgery in obstructive sleep apnea: electrocardiogram-based cardiopulmonary coupling analysis. Laryngoscope 125(7):1737–1742. https://doi.org/10.1002/lary.25101
Lee WH, Ahn JC, We J, Rhee CS, Lee CH, Yun PY, Yoon IY, Kim JW (2014) Cardiopulmonary coupling analysis: changes before and after treatment with a mandibular advancement device. Sleep Breath 18(4):891–896. https://doi.org/10.1007/s11325-014-0961-5
Ramar K, Desrues B, Ramar P, Morgenthaler TI (2013) Analysis of cardiopulmonary coupling to assess adaptive servo-ventilation success in complex sleep apnea management. Sleep Breath 17(2):861–866. https://doi.org/10.1007/s11325-012-0780-5
Lee SH, Choi JH, Park IH, Lee SH, Kim TH, Lee HM, Park HK, Thomas RJ, Shin C, Yun CH (2012) Measuring sleep quality after adenotonsillectomy in pediatric sleep apnea. Laryngoscope 122(9):2115–2121. https://doi.org/10.1002/lary.23356
Ma Y, Hou F, Yang AC, Ahn AC, Fan L, Peng C-K (2019) Symbolic dynamics of electroencephalography is associated with the sleep depth and overall sleep quality in healthy adults. Physica A 513:22–31. https://doi.org/10.1016/j.physa.2018.08.043
Xiong H, Shang P, Hou F, Ma Y (2019) Visibility graph analysis of temporal irreversibility in sleep electroencephalograms. Nonlinear Dyn 96(1):1–11. https://doi.org/10.1007/s11071-019-04768-2
Hou F, Yu Z, Peng CK, Yang A, Wu C, Ma Y (2018) Complexity of wake electroencephalography correlates with slow wave activity after sleep onset. Front Neurosci 12:809. https://doi.org/10.3389/fnins.2018.00809
Mao X, Shang P, Wang J, Ma Y (2018) Characterizing time series by extended complexity-entropy curves based on Tsallis, Renyi, and power spectral entropy. Chaos (Woodbury, NY) 28(11):113106. https://doi.org/10.1063/1.5038758
Ma Y, Shi W, Peng CK, Yang AC (2018) Nonlinear dynamical analysis of sleep electroencephalography using fractal and entropy approaches. Sleep Med Rev 37:85–93. https://doi.org/10.1016/j.smrv.2017.01.003
Shi W, Shang P, Ma Y, Sun S, Yeh C-H (2017) A comparison study on stages of sleep: quantifying multiscale complexity using higher moments on coarse-graining. Commun Nonlinear Sci Numer Simul 44:292–303. https://doi.org/10.1016/j.cnsns.2016.08.019
Thomas RJ, Mietus JE, Peng CK, Guo D, Gozal D, Montgomery-Downs H, Gottlieb DJ, Wang CY, Goldberger AL (2014) Relationship between delta power and the electrocardiogram-derived cardiopulmonary spectrogram: possible implications for assessing the effectiveness of sleep. Sleep Med 15(1):125–131. https://doi.org/10.1016/j.sleep.2013.10.002
Jonas DE, Amick HR, Feltner C, Weber RP, Arvanitis M, Stine A, Lux L, Harris RP (2017) Screening for obstructive sleep apnea in adults: evidence report and systematic review for the US preventive services task force. Jama 317(4):415–433. https://doi.org/10.1001/jama.2016.19635
Ma Y, Yeh J, Sun S, Qiao J, Peng C (2013) Detecting pediatric sleep apnea: consistency on cardiopulmonary coupling and oximetry measurement. Sleep Med 14:e189
Ma Y, Wei Y, Peng C-K (2016) Comparison of wristband-based and ECG-based sleep analyses. J Sleep Disord Ther 05. https://doi.org/10.4172/2167-0277.C1.005
Young A, Home M, Churchward T, Freezer N, Holmes P, Ho M (2002) Comparison of sleep disturbance in mild versus severe Parkinson's disease. Sleep 25(5):573–577
Diederich NJ, Rufra O, Pieri V, Hipp G, Vaillant M (2013) Lack of polysomnographic non-REM sleep changes in early Parkinson’s disease. Mov Disord 28(10):1443–1446. https://doi.org/10.1002/mds.25520
Martinez-Ramirez D, De Jesus S, Walz R, Cervantes-Arriaga A, Peng-Chen Z, Okun MS, Alatriste-Booth V, Rodriguez-Violante M (2015) A polysomnographic study of Parkinson’s disease sleep architecture. J Park Dis 2015:570375. https://doi.org/10.1155/2015/570375
Parrino L, Smerieri A, Spaggiari MC, Terzano MG (2000) Cyclic alternating pattern (CAP) and epilepsy during sleep: how a physiological rhythm modulates a pathological event. Clin Neurophysiol 111(Suppl 2):S39–S46
Tseng PH, Lee PL, Hsu WC, Ma Y, Lee YC, Chiu HM, Ho YL, Chen MF, Wu MS, Peng CK (2017) A higher proportion of metabolic syndrome in Chinese subjects with sleep-disordered breathing: a case-control study based on electrocardiogram-derived sleep analysis. PLoS One 12(1):e0169394. https://doi.org/10.1371/journal.pone.0169394
Ma Y, Yeung A, Yang AC, Peng CK, Clain A, Alpert J, Fava M, Yeung AS (2016) The effects of tai chi on sleep quality in Chinese American patients with major depressive disorder: a pilot study. Behav Sleep Med 16:1–17. https://doi.org/10.1080/15402002.2016.1228643
Funding
Yan Ma would like to acknowledge the grant support from the National Institutes of Health of the USA (T32AT000051). Yulin Wei would like to acknowledge the grant support from the National Natural Science Foundation of China (81273820).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
Chung-Kang Peng is a co-patent holder for the ECG-based analytic technique for phenotyping sleep and sleep apnea, known as cardiopulmonary coupling (CPC) analysis. He also receives royalties from a license issued by Beth Israel Deaconess Medical Center to MyCardio, LLC. The other authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Ethical approval and informed consent
The datasets included in this study were collected previously from clinical studies with separate protocols approved by different Institutional Review Boards (IRB) accordingly, and all procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the studies. All the data we used in this secondary analysis study were de-identified. Therefore, additional IRB approval was waived.
Additional information
Comment
With the caveats of limitations, cardiopulmonary coupling patterns may be a useful approach to screen for apnea in high risk populations. However, the addition of oximetry to the assessment would be complementary - thus those with mildly hypoxic disease will be detected, while those with severe hypoxia can be risk stratified.
Robert Thomas
MA, USA
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ma, Y., Sun, S., Zhang, M. et al. Electrocardiogram-based sleep analysis for sleep apnea screening and diagnosis. Sleep Breath 24, 231–240 (2020). https://doi.org/10.1007/s11325-019-01874-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-019-01874-8