Abstract
Purpose
To analyze the presence of a floppy epiglottis (FE) during drug-induced sleep endoscopy in non-apneic snoring patients, non-positional obstructive sleep apnea (OSA) patients (NPP), and position-dependent OSA patients (PP) and to evaluate the impact of maneuvers and body position during drug-induced sleep endoscopy, including jaw thrust and supine and lateral head (and trunk) position.
Methods
Retrospective cohort study.
Results
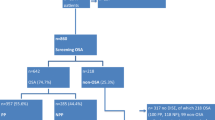
In total, 324 patients were included. In 60 patients (18.5%), a FE was found in supine position: seven non-apneic snoring patients and 53 OSA patients. When performing lateral head rotation only, a FE was present in four patients (NPP, N = 0; PP, N = 4). When patients were tilted to both lateral head and trunk position, a FE was found in only one subject. After applying jaw thrust, a FE was still present in 10 patients. The prevalence of a FE did not differ between NPP and PP. When comparing baseline characteristics between patients with and without a FE in supine position, no significant differences were found.
Conclusion
A FE appears almost exclusively in supine position. In patients with a FE, positional therapy can be a promising alternative as a standalone treatment, but also as part of combination therapy with for example mandibular advancement devices or less invasive forms of upper airway surgery.
Similar content being viewed by others
References
Ravesloot M, Van Maanen J, Dun L, De Vries N (2013) The undervalued potential of positional therapy in position-dependent snoring and obstructive sleep apnea—a review of the literature. Sleep Breath 17(1):39–49
Ravesloot MJ, Frank MH, van Maanen JP, Verhagen EA, de Lange J, de Vries N (2016) Positional OSA part 2: retrospective cohort analysis with a new classification system (APOC). Sleep Breath 20(2):881–888. https://doi.org/10.1007/s11325-015-1206-y
Cartwright RD (1984) Effect of sleep position on sleep apnea severity. Sleep 7(2):110–114
Oksenberg A (2005) Positional and non-positional obstructive sleep apnea patients. Sleep Med 6(4):377–378. https://doi.org/10.1016/j.sleep.2005.03.012
Richard W, Kox D, den Herder C, Laman M, van Tinteren H, de Vries N (2006) The role of sleep position in obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol 263(10):946–950. https://doi.org/10.1007/s00405-006-0090-2
Mador MJ, Kufel TJ, Magalang UJ, Rajesh SK, Watwe V, Grant BJ (2005) Prevalence of positional sleep apnea in patients undergoing polysomnography. Chest 128(4):2130–2137. https://doi.org/10.1378/chest.128.4.2130
Marques M, Genta PR, Sands SA, Azarbazin A, de Melo C, Taranto-Montemurro L, White DP, Wellman A (2017) Effect of sleeping position on upper airway patency in obstructive sleep apnea is determined by the pharyngeal structure causing collapse. Sleep 40(3). https://doi.org/10.1093/sleep/zsx005
Victores AJ, Hamblin J, Gilbert J, Switzer C, Takashima M (2014) Usefulness of sleep endoscopy in predicting positional obstructive sleep apnea. Otolaryngol Head Neck Surg 150(3):487–493. https://doi.org/10.1177/0194599813517984
Azarbarzin A, Marques M, Sands SA, Op de Beeck S, Genta PR, Taranto-Montemurro L, de Melo CM, Messineo L, Vanderveken OM, White DP, Wellman A (2017) Predicting epiglottic collapse in patients with obstructive sleep apnoea. Eur Respir J 50(3):1700345. https://doi.org/10.1183/13993003.00345-2017
Verse T, Pirsig W (1999) Age-related changes in the epiglottis causing failure of nasal continuous positive airway pressure therapy. J Laryngol Otol 113(11):1022–1025
Dedhia RC, Rosen CA, Soose RJ (2014) What is the role of the larynx in adult obstructive sleep apnea? Laryngoscope 124(4):1029–1034. https://doi.org/10.1002/lary.24494
Shimohata T, Tomita M, Nakayama H, Aizawa N, Ozawa T, Nishizawa M (2011) Floppy epiglottis as a contraindication of CPAP in patients with multiple system atrophy. Neurology 76(21):1841–1842. https://doi.org/10.1212/WNL.0b013e31821ccd07
Kent DT, Rogers R, Soose RJ (2015) Drug-induced sedation endoscopy in the evaluation of OSA patients with incomplete oral appliance therapy response. Otolaryngol Head Neck Surg 153(2):302–307. https://doi.org/10.1177/0194599815586978
Catalfumo FJ, Golz A, Westerman ST, Gilbert LM, Joachims HZ, Goldenberg D (1998) The epiglottis and obstructive sleep apnoea syndrome. J Laryngol Otol 112(10):940–943
Golz A, Goldenberg D, Westerman ST, Catalfumo FJ, Netzer A, Westerman LM, Joachims HZ (2000) Laser partial epiglottidectomy as a treatment for obstructive sleep apnea and laryngomalacia. Ann Otol Rhinol Laryngol 109(12 Pt 1):1140–1145. https://doi.org/10.1177/000348940010901211
Bourolias C, Hajiioannou J, Sobol E, Velegrakis G, Helidonis E (2008) Epiglottis reshaping using CO2 laser: a minimally invasive technique and its potent applications. Head Face Med 4:15. https://doi.org/10.1186/1746-160X-4-15
Heiser C (2016) Advanced titration to treat a floppy epiglottis in selective upper airway stimulation. Laryngoscope 126(Suppl 7):S22–S24. https://doi.org/10.1002/lary.26118
De Vito A, Carrasco Llatas M, Ravesloot MJ, Kotecha B, De Vries N, Hamans E, Maurer J, Bosi M, Blumen M, Heiser C (2018) European position paper on drug-induced sleep endoscopy: 2017 update. Clin Otolaryngol 43(6):1541–1552
Schnider T, Minto C (2008) Pharmacokinetic models of propofol for TCI. Anaesthesia 63(2):206–206 author reply 207
Schnider TW, Minto CF, Gambus PL, Andresen C, Goodale DB, Shafer SL, Youngs EJ (1998) The influence of method of administration and covariates on the pharmacokinetics of propofol in adult volunteers. Anesthesiology 88(5):1170–1182
Safiruddin F, Koutsourelakis I, de Vries N (2015) Upper airway collapse during drug induced sleep endoscopy: head rotation in supine position compared with lateral head and trunk position. Eur Arch Otorhinolaryngol 272(2):485–488
Vonk PE, van de Beek MJ, Ravesloot MJL, de Vries N (2018) Drug-induced sleep endoscopy (DISE): new insights in lateral head rotation compared to lateral head and trunk rotation in (non) positional obstructive sleep apnea patients. Laryngoscope. https://doi.org/10.1002/lary.27703
Kezirian EJ, Hohenhorst W, de Vries N (2011) Drug-induced sleep endoscopy: the VOTE classification. Eur Arch Otorhinolaryngol 268(8):1233–1236. https://doi.org/10.1007/s00405-011-1633-8
Oksenberg A, Silverberg DS, Arons E, Radwan H (1997) Positional vs nonpositional obstructive sleep apnea patients: anthropomorphic, nocturnal polysomnographic, and multiple sleep latency test data. Chest 112(3):629–639
Itasaka Y, Miyazaki S, Ishikawa K, Togawa K (2000) The influence of sleep position and obesity on sleep apnea. Psychiatry Clin Neurosci 54(3):340–341. https://doi.org/10.1046/j.1440-1819.2000.00705.x
Torre C, Camacho M, Liu SY, Huon LK, Capasso R (2016) Epiglottis collapse in adult obstructive sleep apnea: a systematic review. Laryngoscope 126(2):515–523. https://doi.org/10.1002/lary.25589
Frank MH, Ravesloot MJ, van Maanen JP, Verhagen E, de Lange J, de Vries N (2015) Positional OSA part 1: towards a clinical classification system for position-dependent obstructive sleep apnoea. Sleep Breath 19(2):473–480. https://doi.org/10.1007/s11325-014-1022-9
Safiruddin F, Koutsourelakis I, de Vries N (2014) Analysis of the influence of head rotation during drug-induced sleep endoscopy in obstructive sleep apnea. Laryngoscope 124(9):2195–2199
Sutthiprapaporn P, Tanimoto K, Ohtsuka M, Nagasaki T, Iida Y, Katsumata A (2008) Positional changes of oropharyngeal structures due to gravity in the upright and supine positions. Dentomaxillofac Radiol 37(3):130–135
Vroegop AV, Vanderveken OM, Wouters K, Hamans E, Dieltjens M, Michels NR, Hohenhorst W, Kezirian EJ, Kotecha BT, de Vries N, Braem MJ, Van de Heyning PH (2013) Observer variation in drug-induced sleep endoscopy: experienced versus nonexperienced ear, nose, and throat surgeons. Sleep 36(6):947–953. https://doi.org/10.5665/sleep.2732
Benoist LB, Verhagen M, Torensma B, van Maanen JP, de Vries N (2016) Positional therapy in patients with residual positional obstructive sleep apnea after upper airway surgery. Sleep Breath 21:279–288. https://doi.org/10.1007/s11325-016-1397-x
van Maanen JP, de Vries N (2014) Long-term effectiveness and compliance of positional therapy with the sleep position trainer in the treatment of positional obstructive sleep apnea syndrome. Sleep 37(7):1209–1215. https://doi.org/10.5665/sleep.3840
van Maanen JP, Meester KA, Dun LN, Koutsourelakis I, Witte BI, Laman DM, Hilgevoord AA, de Vries N (2013) The sleep position trainer: a new treatment for positional obstructive sleep apnoea. Sleep Breath 17(2):771–779
Ravesloot M, White D, Heinzer R, Oksenberg A, Pépin J (2017) Efficacy of the new generation of devices for positional therapy for patients with positional obstructive sleep apnea: a systematic review of the literature and meta-analysis. J Clin Sleep Med 13(6):813–824
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
N. de Vries is a member of the Medical Advisory Board of NightBalance and has shares in NightBalance. He is also an investigator of Inspire and Jazz Pharmaceutics, consultant of Philips, Olympus, and the AE Mann Foundation, and has inventor patent on PCT/US2010/062576 including devices, systems, and methods for monitoring sleep position. All other authors declare that they have no conflicts of interest or financial ties to disclose.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent is not required for this type of study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vonk, P.E., Ravesloot, M.J.L., Kasius, K.M. et al. Floppy epiglottis during drug-induced sleep endoscopy: an almost complete resolution by adopting the lateral posture. Sleep Breath 24, 103–109 (2020). https://doi.org/10.1007/s11325-019-01847-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-019-01847-x