Abstract
Purpose
The purpose of this study is to establish if obstructive sleep apnoea (OSA) predicted by the STOP-BANG questionnaire would be associated with higher rates of post-operative cardiac, respiratory or neurological complications among a selected high-risk population with established major comorbidities undergoing major surgery. We hypothesise that a cohort selected for major comorbidities will show a higher post-operative complication rate that may power any potential association with co-existent OSA and identify an important target group for OSA screening and treatment pathways in preparation for major surgery.
Methods
Patients attending a high-risk preadmission clinic prior to major surgery from May 2015 to November 2015 were prospectively screened for OSA using the STOP-BANG questionnaire. Patients with treated OSA were excluded. Patient data and complications were attained from the pre-admission clinic and subsequent inpatient medical record at discharge.
Results
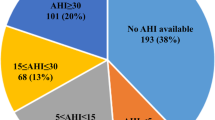
Three-hundred-and-ten patients were included in the study (age 68.6 ± 13.1 years, body mass index [BMI] 30.6 ± 7.4 kg/m2; 52.9% female). Sixty-four patients (20.6%) experienced 82 post-operative complications. Seventy-five percent of the cohort had a STOP-BANG ≥ 3. There was no association between the STOP-BANG score (unadjusted and adjusted for comorbidity) with the development of post-operative complications.
Conclusions
OSA predicted by the STOP-BANG score was not associated with higher rates of post-operative complications in patients with major comorbidities undergoing high-risk surgery. As the findings from this cohort contrast with other observational studies, more definitive studies are required to establish a causative link between OSA and post-operative complications and determine whether treating OSA reduces this complication rate.
Similar content being viewed by others
References
Narkiewicz K, Somers VK (1997) The sympathetic nervous system and obstructive sleep apnea: implications for hypertension. J Hypertens 15(12 Pt 2):1613–1619
Senaratna CV, Perret JL, Lodge CJ, Lowe AJ, Campbell BE, Matheson MC, Hamilton GS, Dharmage SC (2017) Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev 34:70–81
Knauert M, Naik S, Gillespie MB, Kryger M (2015) Clinical consequences and economic costs of untreated obstructive sleep apnea syndrome. World J Otorhinolaryngol Head Neck Surg 1(1):17–27
Marin JM, Carrizo SJ, Vicente E, Agusti AG (2005) Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 365(9464):1046–1053
Yu J, Zhou Z, McEvoy R et al (2017) Association of positive airway pressure with cardiovascular events and death in adults with sleep apnea: a systematic review and meta-analysis. Jama. 318(2):156–166
Finkel KJ, Searleman AC, Tymkew H, Tanaka CY, Saager L, Safer-Zadeh E, Bottros M, Selvidge JA, Jacobsohn E, Pulley D, Duntley S, Becker C, Avidan MS (2009) Prevalence of undiagnosed obstructive sleep apnea among adult surgical patients in an academic medical center. Sleep Med 10(7):753–758
Chung F, Liao P, Elsaid H, Shapiro CM, Kang W (2014) Factors associated with postoperative exacerbation of sleep-disordered breathing. Anesthesiology. 120(2):299–311
Gupta RM, Parvizi J, Hanssen AD, Gay PC (2001) Postoperative complications in patients with obstructive sleep apnea syndrome undergoing hip or knee replacement: a case-control study. Mayo Clin Proc 76(9):897–905
Abdelsattar ZM, Hendren S, Wong SL, Campbell DA Jr, Ramachandran SK (2015) The impact of untreated obstructive sleep apnea on cardiopulmonary complications in general and vascular surgery: a cohort study. Sleep. 38(8):1205–1210
Ahmad S, Nagle A, McCarthy RJ, Fitzgerald PC, Sullivan JT, Prystowsky J (2008) Postoperative hypoxemia in morbidly obese patients with and without obstructive sleep apnea undergoing laparoscopic bariatric surgery. Anesth Analg 107(1):138–143
Ursavaş A, Güven T, Coskun F, Ege E, Yılmazlar A (2013) Association between self reported snoring, STOP questionnaire and postoperative pulmonary complications in patients submitted to ortophaedic surgery. Multidiscip Respir Med 8(1):3
Hai F, Porhomayon J, Vermont L, Frydrych L, Jaoude P, El-Solh AA (2014) Postoperative complications in patients with obstructive sleep apnea: a meta-analysis. J Clin Anesth 26(8):591–600
Kaw R, Chung F, Pasupuleti V, Mehta J, Gay PC, Hernandez AV (2012) Meta-analysis of the association between obstructive sleep apnoea and postoperative outcome. Br J Anaesth 109(6):897–906
Liao P, Luo Q, Elsaid H, Kang W, Shapiro CM, Chung F (2013) Perioperative auto-titrated continuous positive airway pressure treatment in surgical patients with obstructive sleep apnea: a randomized controlled trial. Anesthesiology. 119(4):837–847
O'Gorman SM, Gay PC, Morgenthaler TI (2013) Does autotitrating positive airway pressure therapy improve postoperative outcome in patients at risk for obstructive sleep apnea syndrome? A randomized controlled clinical trial. Chest. 144(1):72–78
Chung F, Subramanyam R, Liao P, Sasaki E, Shapiro C, Sun Y (2012) High STOP-Bang score indicates a high probability of obstructive sleep apnoea. Br J Anaesth 108(5):768–775
Chiu HY, Chen PY, Chuang LP, Chen NH, Tu YK, Hsieh YJ, Wang YC, Guilleminault C (2017) Diagnostic accuracy of the Berlin questionnaire, STOP-BANG, STOP, and Epworth Sleepiness Scale in detecting obstructive sleep apnea: a bivariate meta-analysis. Sleep Med Rev 36:57–70
Vasu TS, Doghramji K, Cavallazzi R, Grewal R, Hirani A, Leiby B, Markov D, Reiter D, Kraft WK, Witkowski T (2010) Obstructive sleep apnea syndrome and postoperative complications: clinical use of the STOP-BANG questionnaire. Arch Otolaryngol Head Neck Surg 136(10):1020–1024
Schaumburg I (2017) ASA physical status classification system; [approved 2014 Oct 15; cited 2017 Feb 6]; 1 screen. American Society of Anesthesiologists Clinical Information [Internet]
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP (2008) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 61(4):344–349
Nagappa M, Mokhlesi B, Wong J, Wong DT, Kaw R, Chung F (2015) The effects of continuous positive airway pressure on postoperative outcomes in obstructive sleep apnea patients undergoing surgery: a systematic review and meta-analysis. Anesth Analg 120(5):1013–1023
Gali B, Whalen FX, Gay PC, Olson EJ, Schroeder DR, Plevak DJ et al (2007) Management plan to reduce risks in perioperative care of patients with presumed obstructive sleep apnea syndrome. J Clin Sleep Med 3(6):582–588
Lockhart EM, Willingham MD, Abdallah AB, Helsten DL, Bedair BA, Thomas J, Duntley S, Avidan MS (2013) Obstructive sleep apnea screening and postoperative mortality in a large surgical cohort. Sleep Med 14(5):407–415
Hwang D, Shakir N, Limann B, Sison C, Kalra S, Shulman L, Souza AC, Greenberg H (2008) Association of sleep-disordered breathing with postoperative complications. Chest. 133(5):1128–1134
Memtsoudis S, Liu SS, Ma Y, Chiu YL, Walz JM, Gaber-Baylis LK, Mazumdar M (2011) Perioperative pulmonary outcomes in patients with sleep apnea after noncardiac surgery. Anesth Analg 112(1):113–121
Mokhlesi B, Hovda MD, Vekhter B, Arora VM, Chung F, Meltzer DO (2013) Sleep-disordered breathing and postoperative outcomes after bariatric surgery: analysis of the nationwide inpatient sample. Obes Surg 23(11):1842–1851
Mokhlesi B, Hovda MD, Vekhter B, Arora VM, Chung F, Meltzer DO (2013) Sleep-disordered breathing and postoperative outcomes after elective surgery: analysis of the nationwide inpatient sample. Chest. 144(3):903–914
Auckley D, Bolden N (2012) Preoperative screening and perioperative care of the patient with sleep-disordered breathing. Curr Opin Pulm Med 18(6):588–595
Chung F, Memtsoudis SG, Ramachandran SK, Nagappa M, Opperer M, Cozowicz C, Patrawala S, Lam D, Kumar A, Joshi GP, Fleetham J, Ayas N, Collop N, Doufas AG, Eikermann M, Englesakis M, Gali B, Gay P, Hernandez AV, Kaw R, Kezirian EJ, Malhotra A, Mokhlesi B, Parthasarathy S, Stierer T, Wappler F, Hillman DR, Auckley D (2016) Society of Anesthesia and Sleep Medicine Guidelines on preoperative screening and assessment of adult patients with obstructive sleep apnea. Anesth Analg 123(2):452–473
Acknowledgements
Dr. Ai-Ming Wong received an RTP stipend by Monash University for graduate research studies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Associate Professor Garun Hamilton has received equipment to support research from Resmed, Phillips Respironics and Air Liquide Healthcare, outside the submitted work. All other co-authors including Dr. Ai-Ming Wong, Dr. Michael Wang, Dr. Daniel Garner, Ms. Sara Bowditch, Dr. Eldho Paul, Dr. Mark Adams and Associate Professor Darren Mansfield declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of Monash Health, the National Health and Medical Research Council (NHMRC) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- ASAPS
-
American Society of Anesthesiologists Physical Status classification score
- BMI
-
Body mass index
- BPAP
-
Bilevel positive airway pressure
- CPAP
-
Continuous positive airway pressure
- ESS
-
Epworth Sleepiness Scale
- HDU
-
High-dependency unit
- ICU
-
Intensive care unit
- NIV
-
Non-invasive ventilation
- OSA
-
Obstructive sleep apnoea
- RCT
-
Randomised controlled trials
Rights and permissions
About this article
Cite this article
Wong, AM., Wang, M., Garner, D.J. et al. Obstructive sleep apnoea predicted by the STOP-BANG questionnaire is not associated with higher rates of post-operative complications among a high-risk surgical cohort. Sleep Breath 24, 135–142 (2020). https://doi.org/10.1007/s11325-019-01825-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-019-01825-3