Abstract
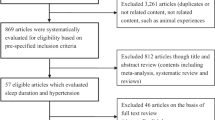
The association between sleep duration and obesity risk remains unclear. We performed an updated meta-analysis to quantify a potential dose-response relation between sleep duration and risk of obesity. PubMed and Embase were searched for prospective cohort studies examining the association between sleep duration and risk of obesity that were published up to October 28, 2017. Random effects models were used to evaluate the pooled relative risks (RRs) and 95% confidence intervals (CIs) for the association of sleep duration and obesity. Restricted cubic splines were used to model the dose-response association. The meta-analysis included 12 studies (16 reports). We found a reverse J-shaped relation between sleep duration and obesity, with the lowest risk at 7–8-h sleep per day. Compared with 7-h sleep duration per day, the pooled relative risks for obesity were 1.09 (95% CI 1.05–1.14) for each 1-h decrement among individuals who slept < 7 h per day and 1.02 (95% CI 0.99–1.05) for each 1-h increment of sleep duration among individuals with longer sleep duration. Short sleep duration significantly increased the risk of obesity. Compared with 7-h sleep duration per day, the risk of obesity increases 9% for each 1-h decrease in sleep duration.




Similar content being viewed by others
References
Leandra Abarca-Gomez ZAA, Hamid ZA, Abu-Rmeileh NM (2017) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 390(10113):2627–2642. https://doi.org/10.1016/s0140-6736(17)32129-3
Haslam DW, James WP (2005) Obesity. Lancet 366(9492):1197–1209. https://doi.org/10.1016/s0140-6736(05)67483-1
Kirszenblat L, van Swinderen B (2015) The yin and yang of sleep and attention. Trends Neurosci 38(12):776–786. https://doi.org/10.1016/j.tins.2015.10.001
Shen X, Wu Y, Zhang D (2016) Nighttime sleep duration, 24-hour sleep duration and risk of all-cause mortality among adults: a meta-analysis of prospective cohort studies. Sci Rep 6:21480. https://doi.org/10.1038/srep21480
Cappuccio FP, D’Elia L, Strazzullo P, Miller MA (2010) Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep 33(5):585–592
Gallicchio L, Kalesan B (2009) Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res 18(2):148–158. https://doi.org/10.1111/j.1365-2869.2008.00732.x
Cappuccio FP, D’Elia L, Strazzullo P, Miller MA (2010) Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care 33(2):414–420. https://doi.org/10.2337/dc09-1124
Shan Z, Ma H, Xie M, Yan P, Guo Y, Bao W, Rong Y, Jackson CL, Hu FB, Liu L (2015) Sleep duration and risk of type 2 diabetes: a meta-analysis of prospective studies. Diabetes Care 38(3):529–537. https://doi.org/10.2337/dc14-2073
Guo X, Zheng L, Wang J, Zhang X, Zhang X, Li J, Sun Y (2013) Epidemiological evidence for the link between sleep duration and high blood pressure: a systematic review and meta-analysis. Sleep Med 14(4):324–332. https://doi.org/10.1016/j.sleep.2012.12.001
Wang Y, Mei H, Jiang YR, Sun WQ, Song YJ, Liu SJ, Jiang F (2015) Relationship between duration of sleep and hypertension in adults: a meta-analysis. J Clin Sleep Med 11(9):1047–1056. https://doi.org/10.5664/jcsm.5024
Cappuccio FP, Cooper D, D’Elia L, Strazzullo P, Miller MA (2011) Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J 32(12):1484–1492. https://doi.org/10.1093/eurheartj/ehr007
Leng Y, Cappuccio FP, Wainwright NW, Surtees PG, Luben R, Brayne C, Khaw KT (2015) Sleep duration and risk of fatal and nonfatal stroke: a prospective study and meta-analysis. Neurology 84(11):1072–1079. https://doi.org/10.1212/wnl.0000000000001371
Wang D, Li W, Cui X, Meng Y, Zhou M, Xiao L, Ma J, Yi G, Chen W (2016) Sleep duration and risk of coronary heart disease: a systematic review and meta-analysis of prospective cohort studies. Int J Cardiol 219:231–239. https://doi.org/10.1016/j.ijcard.2016.06.027
Kronholm E, Partonen T, Laatikainen T, Peltonen M, Harma M, Hublin C, Kaprio J, Aro AR, Partinen M, Fogelholm M, Valve R, Vahtera J, Oksanen T, Kivimaki M, Koskenvuo M, Sutela H (2008) Trends in self-reported sleep duration and insomnia-related symptoms in Finland from 1972 to 2005: a comparative review and re-analysis of Finnish population samples. J Sleep Res 17(1):54–62. https://doi.org/10.1111/j.1365-2869.2008.00627.x
Knutson KL, Van Cauter E, Rathouz PJ, DeLeire T, Lauderdale DS (2010) Trends in the prevalence of short sleepers in the USA: 1975-2006. Sleep 33(1):37–45
Rowshan Ravan A, Bengtsson C, Lissner L, Lapidus L, Bjorkelund C (2010) Thirty-six-year secular trends in sleep duration and sleep satisfaction, and associations with mental stress and socioeconomic factors—results of the Population Study of Women in Gothenburg, Sweden. J Sleep Res 19(3):496–503. https://doi.org/10.1111/j.1365-2869.2009.00815.x
Van Cauter E, Knutson KL (2008) Sleep and the epidemic of obesity in children and adults. Eur J Endocrinol 159(Suppl 1):S59–S66. https://doi.org/10.1530/eje-08-0298
Chaput JP, Despres JP, Bouchard C, Tremblay A (2008) The association between sleep duration and weight gain in adults: a 6-year prospective study from the Quebec Family Study. Sleep 31(4):517–523
Patel SR, Malhotra A, White DP, Gottlieb DJ, Hu FB (2006) Association between reduced sleep and weight gain in women. Am J Epidemiol 164(10):947–954. https://doi.org/10.1093/aje/kwj280
Kobayashi D, Takahashi O, Shimbo T, Okubo T, Arioka H, Fukui T (2013) High sleep duration variability is an independent risk factor for weight gain. Sleep Breath 17(1):167–172. https://doi.org/10.1007/s11325-012-0665-7
Gangwisch JE, Malaspina D, Boden-Albala B, Heymsfield SB (2005) Inadequate sleep as a risk factor for obesity: analyses of the NHANES I. Sleep 28(10):1289–1296
Hasler G, Buysse DJ, Klaghofer R, Gamma A, Ajdacic V, Eich D, Rossler W, Angst J (2004) The association between short sleep duration and obesity in young adults: a 13-year prospective study. sleep 27(4):661–666
Gutierrez-Repiso C, Soriguer F, Rubio-Martin E, Esteva de Antonio I, Ruiz de Adana MS, Almaraz MC, Olveira-Fuster G, Morcillo S, Valdes S, Lago-Sampedro AM, Garcia-Fuentes E, Rojo-Martinez G (2014) Night-time sleep duration and the incidence of obesity and type 2 diabetes. Findings from the prospective Pizarra study. Sleep Med 15(11):1398–1404. https://doi.org/10.1016/j.sleep.2014.06.014
Itani O, Kaneita Y, Murata A, Yokoyama E, Ohida T (2011) Association of onset of obesity with sleep duration and shift work among Japanese adults. Sleep Med 12(4):341–345. https://doi.org/10.1016/j.sleep.2010.09.007
Nishiura C, Hashimoto H (2010) A 4-year study of the association between short sleep duration and change in body mass index in Japanese male workers. J Epidemiol 20(5):385–390
Xiao Q, Arem H, Moore SC, Hollenbeck AR, Matthews CE (2013) A large prospective investigation of sleep duration, weight change, and obesity in the NIH-AARP Diet and Health Study cohort. Am J Epidemiol 178(11):1600–1610. https://doi.org/10.1093/aje/kwt180
Bjorkelund C, Bondyr-Carlsson D, Lapidus L, Lissner L, Mansson J, Skoog I, Bengtsson C (2005) Sleep disturbances in midlife unrelated to 32-year diabetes incidence: the prospective population study of women in Gothenburg. Diabetes Care 28(11):2739–2744
Stranges S, Cappuccio FP, Kandala NB, Miller MA, Taggart FM, Kumari M, Ferrie JE, Shipley MJ, Brunner EJ, Marmot MG (2008) Cross-sectional versus prospective associations of sleep duration with changes in relative weight and body fat distribution: the Whitehall II Study. Am J Epidemiol 167(3):321–329. https://doi.org/10.1093/aje/kwm302
Nagai M, Tomata Y, Watanabe T, Kakizaki M, Tsuji I (2013) Association between sleep duration, weight gain, and obesity for long period. Sleep Med 14(2):206–210. https://doi.org/10.1016/j.sleep.2012.09.024
Nishiura C, Hashimoto H (2014) Sleep duration and weight gain: reconsideration by panel data analysis. J Epidemiol 24(5):404–409
Cappuccio FP, Taggart FM, Kandala NB, Currie A, Peile E, Stranges S, Miller MA (2008) Meta-analysis of short sleep duration and obesity in children and adults. Sleep 31(5):619–626
Wu Y, Zhai L, Zhang D (2014) Sleep duration and obesity among adults: a meta-analysis of prospective studies. Sleep Med 15(12):1456–1462. https://doi.org/10.1016/j.sleep.2014.07.018
Well G, Shea B, O’Connell D, Robertson J, Peterson J, Welch V, Losos M, Tugwell P The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses
Orsini N, Li R, Wolk A, Khudyakov P, Spiegelman D (2012) Meta-analysis for linear and nonlinear dose-response relations: examples, an evaluation of approximations, and software. Am J Epidemiol 175(1):66–73. https://doi.org/10.1093/aje/kwr265
Bekkering GE, Harris RJ, Thomas S, Mayer AM, Beynon R, Ness AR, Harbord RM, Bain C, Smith GD, Sterne JA (2008) How much of the data published in observational studies of the association between diet and prostate or bladder cancer is usable for meta-analysis? Am J Epidemiol 167(9):1017–1026. https://doi.org/10.1093/aje/kwn005
Hamling J, Lee P, Weitkunat R, Ambuhl M (2008) Facilitating meta-analyses by deriving relative effect and precision estimates for alternative comparisons from a set of estimates presented by exposure level or disease category. Stat Med 27(7):954–970. https://doi.org/10.1002/sim.3013
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7(3):177–188
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560. https://doi.org/10.1136/bmj.327.7414.557
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634
Nishiura C, Noguchi J, Hashimoto H (2010) Dietary patterns only partially explain the effect of short sleep duration on the incidence of obesity. sleep 33(6):753–757
Watanabe M, Kikuchi H, Tanaka K, Takahashi M (2010) Association of short sleep duration with weight gain and obesity at 1-year follow-up: a large-scale prospective study. Sleep 33(2):161–167
Vgontzas AN, Fernandez-Mendoza J, Miksiewicz T, Kritikou I, Shaffer ML, Liao D, Basta M, Bixler EO (2014) Unveiling the longitudinal association between short sleep duration and the incidence of obesity: the Penn State Cohort. Int J Obes (Lond) 38(6):825–832. https://doi.org/10.1038/ijo.2013.172
Sayon-Orea C, Bes-Rastrollo M, Carlos S, Beunza JJ, Basterra-Gortari FJ, Martinez-Gonzalez MA (2013) Association between sleeping hours and siesta and the risk of obesity: the SUN Mediterranean Cohort. Obes Facts 6(4):337–347. https://doi.org/10.1159/000354746
Kobayashi D, Takahashi O, Deshpande GA, Shimbo T, Fukui T (2012) Association between weight gain, obesity, and sleep duration: a large-scale 3-year cohort study. Sleep Breath 16(3):829–833. https://doi.org/10.1007/s11325-011-0583-0
Chaput JP, Sjodin AM, Astrup A, Despres JP, Bouchard C, Tremblay A (2010) Risk factors for adult overweight and obesity: the importance of looking beyond the ‘big two’. Obes Facts 3(5):320–327. https://doi.org/10.1159/000321398
Magee CA, Huang XF, Iverson DC, Caputi P (2010) Examining the pathways linking chronic sleep restriction to obesity. J Obes 2010:1–8. https://doi.org/10.1155/2010/821710
Leproult R, Van Cauter E (2010) Role of sleep and sleep loss in hormonal release and metabolism. Endocr Dev 17:11–21. https://doi.org/10.1159/000262524
Chaput JP, Despres JP, Bouchard C, Tremblay A (2007) Short sleep duration is associated with reduced leptin levels and increased adiposity: results from the Quebec family study. Obes (Silver Spring) 15(1):253–261. https://doi.org/10.1038/oby.2007.512
Spiegel K, Tasali E, Penev P, Van Cauter E (2004) Brief communication: sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med 141(11):846–850
Schmid SM, Hallschmid M, Jauch-Chara K, Born J, Schultes B (2008) A single night of sleep deprivation increases ghrelin levels and feelings of hunger in normal-weight healthy men. J Sleep Res 17(3):331–334. https://doi.org/10.1111/j.1365-2869.2008.00662.x
Taheri S, Lin L, Austin D, Young T, Mignot E (2004) Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med 1(3):e62. https://doi.org/10.1371/journal.pmed.0010062
Ohida T, Kamal AM, Uchiyama M, Kim K, Takemura S, Sone T, Ishii T (2001) The influence of lifestyle and health status factors on sleep loss among the Japanese general population. Sleep 24(3):333–338
Stamatakis KA, Brownson RC (2008) Sleep duration and obesity-related risk factors in the rural Midwest. Prev Med 46(5):439–444. https://doi.org/10.1016/j.ypmed.2007.11.008
Cizza G, Requena M, Galli G, de Jonge L (2011) Chronic sleep deprivation and seasonality: implications for the obesity epidemic. J Endocrinol Investig 34(10):793–800. https://doi.org/10.3275/7808
Kyrou I, Tsigos C (2009) Stress hormones: physiological stress and regulation of metabolism. Curr Opin Pharmacol 9(6):787–793. https://doi.org/10.1016/j.coph.2009.08.007
Tan DX, Manchester LC, Fuentes-Broto L, Paredes SD, Reiter RJ (2011) Significance and application of melatonin in the regulation of brown adipose tissue metabolism: relation to human obesity. Obes Rev 12(3):167–188. https://doi.org/10.1111/j.1467-789X.2010.00756.x
Puig-Domingo M, Guerrero JM, Menendez-Pelaez A, Reiter RJ (1989) Melatonin specifically stimulates type-II thyroxine 5′-deiodination in brown adipose tissue of Syrian hamsters. J Endocrinol 122(2):553–556
Prunet-Marcassus B, Desbazeille M, Bros A, Louche K, Delagrange P, Renard P, Casteilla L, Penicaud L (2003) Melatonin reduces body weight gain in Sprague Dawley rats with diet-induced obesity. Endocrinology 144(12):5347–5352. https://doi.org/10.1210/en.2003-0693
Puchalski SS, Green JN, Rasmussen DD (2003) Melatonin effect on rat body weight regulation in response to high-fat diet at middle age. Endocrine 21(2):163–167. https://doi.org/10.1385/endo:21:2:163
St-Onge MP, Perumean-Chaney S, Desmond R, Lewis CE, Yan LL, Person SD, Allison DB (2010) Gender differences in the association between sleep duration and body composition: the Cardia Study. Int J Endocrinol 2010:726071. https://doi.org/10.1155/2010/726071
Chandola T, Ferrie JE, Perski A, Akbaraly T, Marmot MG (2010) The effect of short sleep duration on coronary heart disease risk is greatest among those with sleep disturbance: a prospective study from the Whitehall II cohort. Sleep 33(6):739–744
Funding
This study was funded by the National Natural Science Foundation of China (grant nos. 81373074, 81402752, and 81673260); the Natural Science Foundation of Guangdong Province (grant no. 2017A030313452); the Science and Technology Development Foundation of Shenzhen (grant nos. JCYJ 20170302143855721 and JCYJ 20170412110537191); and the Postgraduate Innovation Development Fund Project of Shenzhen University (grant no. 31500004151).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Not applicable for this meta-analysis in which all analyses were based on published literature.
Informed consent
Not applicable for this meta-analysis in which all analyses were based on published literature.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOC 1274 kb)
Rights and permissions
About this article
Cite this article
Zhou, Q., Zhang, M. & Hu, D. Dose-response association between sleep duration and obesity risk: a systematic review and meta-analysis of prospective cohort studies. Sleep Breath 23, 1035–1045 (2019). https://doi.org/10.1007/s11325-019-01824-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-019-01824-4