Abstract
Purpose
In patients with overlap syndrome (OVS), the pathophysiologies of obstructive sleep apnea (OSA) and chronic obstructive pulmonary disease can interact with one another. Focusing on low arousal threshold, the authors evaluated polysomnographic features of OVS patients.
Methods
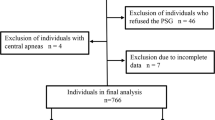
This retrospective, multicenter study was conducted at three hospitals in Japan. Patients aged ≥ 60 years who underwent polysomnography and pulmonary function testing were reviewed. Severity of airflow limitation (AFL) was classified according to the Global Initiative for Chronic Obstructive Lung Disease criteria. Low arousal threshold was predicted based on the following polysomnography features: lower apnea-hypopnea index (AHI); higher nadir oxygen saturation, and larger hypopnea fraction of total respiratory events. These features were compared among patients with only OSA (n = 126), OVS with mild AFL (n = 16), and OVS with moderate/severe AFL (n = 22).
Results
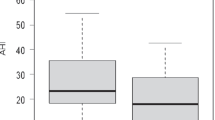
A low arousal threshold was more frequently exhibited by OVS patients with moderate/severe AFL than by those with OSA only (p = 0.016) and OVS with mild AFL (p = 0.026). As forced expiratory volume in 1 s/forced vital capacity (FEV1/FVC) decreased in OVS patients, the mean length of apnea decreased (r = 0.388, p = 0.016), hypopnea fractions increased (r = − 0.337, p = 0.039), and AHI decreased (r = 0.424, p = 0.008). FEV1/FVC contributed to low arousal threshold independent of age, sex, smoking history, hospital, or body mass index in all subjects (OR 0.946 [95% CI 0.909–0.984]) and in OVS patients (OR 0.799 [95% CI 0.679–0.940]).
Conclusions
This study first described peculiar polysomnographic features in OVS patients with moderate/severe AFL, suggesting a high prevalence of low arousal threshold.
Similar content being viewed by others
References
Fukuchi Y, Nishimura M, Ichinose M, Adachi M, Nagai A, Kuriyama T, Takahashi K, Nishimura K, Ishioka S, Aizawa H, Zaher C (2004) COPD in Japan: the Nippon COPD epidemiology study. Respirology 9(4):458–465
Ueyama M, Kokuto H, Sugihara H, Oikawa S, Suzuki F, Goto H, Kudoh S (2018) Investigation of obstructive sleep apnea using portable monitors and health check data in Japanese drivers. J Atheroscler Thromb 25:1118–1127. https://doi.org/10.5551/jat.41806
Shawon MS, Perret JL, Senaratna CV, Lodge C, Hamilton GS, Dharmage SC (2017) Current evidence on prevalence and clinical outcomes of co-morbid obstructive sleep apnea and chronic obstructive pulmonary disease: a systematic review. Sleep Med Rev 32:58–68. https://doi.org/10.1016/j.smrv.2016.02.007
Zhao YY, Blackwell T, Ensrud KE, Stone KL, Omachi TA, Redline S, Osteoporotic Fractures in Men (MrOS) Study Group (2016) Sleep apnea and obstructive airway disease in older men: outcomes of sleep disorders in older men study. Sleep 39(7):1343–1351. https://doi.org/10.5665/sleep.5960
Marin JM, Soriano JB, Carrizo SJ, Boldova A, Celli BR (2010) Outcomes in patients with chronic obstructive pulmonary disease and obstructive sleep apnea: the overlap syndrome. Am J Respir Crit Care Med 182(3):325–331. https://doi.org/10.1164/rccm.200912-1869OC
Owens RL, Macrea MM, Teodorescu M (2017) The overlaps of asthma or COPD with OSA: a focused review. Respirology 22(6):1073–1083. https://doi.org/10.1111/resp.13107
Malhotra A, Schwartz AR, Schneider H, Owens RL, DeYoung P, Han MK, Wedzicha JA, Hansel NN, Zeidler MR, Wilson KC, Badr MS, ATS Assembly on Sleep and Respiratory Neurobiology (2018) Research Priorities in Pathophysiology for Sleep-disordered Breathing in Patients with Chronic Obstructive Pulmonary Disease. An Official American Thoracic Society Research Statement. Am J Respir Crit Care Med 197(3):289–299. https://doi.org/10.1164/rccm.201712-2510ST
Bosi M, De Vito A, Kotecha B, Viglietta L, Braghiroli A, Steier J, Pengo M, Sorrenti G, Gobbi R, Vicini C, Poletti V (2018) Phenotyping the pathophysiology of obstructive sleep apnea using polygraphy/polysomnography: a review of the literature. Sleep Breath 22(3):579–592. https://doi.org/10.1007/s11325-017-1613-3
Edwards BA, Eckert DJ, Jordan AS (2017) Obstructive sleep apnoea pathogenesis from mild to severe: is it all the same? Respirology 22(1):33–42. https://doi.org/10.1111/resp.12913
White DP (2005) Pathogenesis of obstructive and central sleep apnea. Am J Respir Crit Care Med 172(11):1363–1370
Edwards BA, Eckert DJ, McSharry DG, Sands SA, Desai A, Kehlmann G, Bakker JP, Genta PR, Owens RL, White DP, Wellman A, Malhotra A (2014) Clinical predictors of the respiratory arousal threshold in patients with obstructive sleep apnea. Am J Respir Crit Care Med 190(11):1293–1300. https://doi.org/10.1164/rccm.201404-0718OC
Eckert DJ, Younes MK (2014) Arousal from sleep: implications for obstructive sleep apnea pathogenesis and treatment. J Appl Physiol (1985) 116(3):302–313. https://doi.org/10.1152/japplphysiol.00649.2013
Budhiraja R, Siddiqi TA, Quan SF (2015) Sleep disorders in chronic obstructive pulmonary disease: etiology, impact, and management. J Clin Sleep Med 11(3):259–270. https://doi.org/10.5664/jcsm.4540
Tamura G, Aizawa H, Nagai A, Inoue H (2007) Common prediction equations of respiratory function tests from children to adults in Japan. Nihon Kokyuki Gakkai Zasshi 45(7):526–542
Biselli P, Grossman PR, Kirkness JP, Patil SP, Smith PL, Schwartz AR, Schneider H (2015) The effect of increased lung volume in chronic obstructive pulmonary disease on upper airway obstruction during sleep. J Appl Physiol (1985) 119(3):266–271. https://doi.org/10.1152/japplphysiol.00455.2014
Krachman SL, Tiwari R, Vega ME, Yu D, Soler X, Jaffe F, Kim V, Swift I, D’Alonzo GE, Criner GJ, Investigators COPDG (2016) Effect of emphysema severity on the apnea-hypopnea index in smokers with obstructive sleep apnea. Ann Am Thorac Soc 13(7):1129–1135. https://doi.org/10.1513/AnnalsATS.201511-765OC
Zinchuk A, Edwards BA, Jeon S, Koo BB, Concato J, Sands S, Wellman A, Yaggi HK (2018) Prevalence, associated clinical features, and impact on continuous positive airway pressure use of a low respiratory arousal threshold among male United States veterans with obstructive sleep apnea. J Clin Sleep Med 14(5):809–817. https://doi.org/10.5664/jcsm.7112
Eckert DJ, Owens RL, Kehlmann GB, Wellman A, Rahangdale S, Yim-Yeh S, White DP, Malhotra A (2011) Eszopiclone increases the respiratory arousal threshold and lowers the apnoea/hypopnoea index in obstructive sleep apnoea patients with a low arousal threshold. Clin Sci (Lond) 120(12):505–514. https://doi.org/10.1042/CS20100588
Smith PR, Sheikh KL, Costan-Toth C, Forsthoefel D, Bridges E, Andrada TF, Holley AB (2017) Eszopiclone and zolpidem do not affect the prevalence of the low arousal threshold phenotype. J Clin Sleep Med 13(1):115–119. https://doi.org/10.5664/jcsm.6402
Lancaster LH, Mason WR, Parnell JA, Rice TW, Loyd JE, Milstone AP, Collard HR, Malow BA (2009) Obstructive sleep apnea is common in idiopathic pulmonary fibrosis. Chest 136(3):772–778. https://doi.org/10.1378/chest.08-2776
Lee RWW, Sutherland K, Sands SA, Edwards BA, Chan TO, S S Ng S, Hui DS, Cistulli PA (2017) Differences in respiratory arousal threshold in Caucasian and Chinese patients with obstructive sleep apnoea. Respirology 22(5):1015–1021. https://doi.org/10.1111/resp.13022
Acknowledgements
We thank Dr. Takeo Ishii from GlaxoSmithKline for helpful discussion while he was a member of the Respiratory Care clinic.
Funding
The present study was supported by GOLD-Jac.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Given the retrospective nature of the study and the use of anonymized patient data, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PDF 159 kb)
Rights and permissions
About this article
Cite this article
Yamaguchi, Y., Shiota, S., Kusunoki, Y. et al. Polysomnographic features of low arousal threshold in overlap syndrome involving obstructive sleep apnea and chronic obstructive pulmonary disease. Sleep Breath 23, 1095–1100 (2019). https://doi.org/10.1007/s11325-019-01786-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-019-01786-7