Abstract
Purpose
According to many studies in the literature, there is a strong association between restless leg syndrome and dopaminergic dysfunction. Dopamine is also the major catecholamine in the retina and is also a possible transmitter of the amacrine and interplexiform cells. The aim of this study is to investigate the possible association between RLS and retinal thickness.
Methods
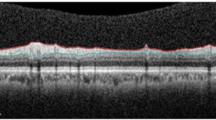
In this study, we included 33 patients who were diagnosed with idiopathic RLS according to the “International RLS Study Group” criteria and 31 healthy subjects. All the patients and controls underwent routine ophthalmologic examination and had spectral-domain optical coherence tomography (OCT) performed. We compared the retinal thickness of the patients and control subjects.
Results
In the RLS group, foveal thickness was thinner then controls. Also, only inferior, superior, and temporal quadrant retina nerve fiber layer (RNFL) thickness were significantly thinner in the RLS group. The parafoveal ganglion cell complex (GCC) in the superior temporal, inferior temporal, inferior nasal quadrant, and perifoveal superior nasal thickness was also significantly thinner in the patient group. Pearson correlation analyses showed that there were statistically significant negative correlations between disease duration and macular GCC and RNFL thickness. Negative correlations were also detected between parafoveal superior, temporal, inferior and nasal macular thickness, parafoveal superior nasal, inferior temporal GCC thickness, and perifoveal superior nasal GCC thickness and disease duration.
Conclusion
According to our results; most retinal layers are thinner in RLS patients, so it can be considered that OCT has a predictive value for progression of RLS.
Similar content being viewed by others
References
Trotti LM (2017) Restless legs syndrome and sleep-related movement disorders. Continuum (Minneap Minn) 23(4, Sleep Neurology):1005–1016. https://doi.org/10.1212/CON.0000000000000488
Allen RP, Picchietti DL, Garcia-Borreguero D, Ondo WG, Walters AS, Winkelman JW, Zucconi M, Ferri R, Trenkwalder C, Lee HB (2014) Restless legs syndrome/Willis-Ekbom disease diagnostic criteria: updated International Restless Legs Syndrome Study Group (IRLSSG) consensus criteria--history, rationale, description, and significance. Sleep Med 15(8):860–873. https://doi.org/10.1016/j.sleep.2014.03.025
Marin LF, Carvalho LBC, Prado LBF, Oliveira ASB, Prado GF (2017) Restless legs syndrome is highly prevalent in patients with post-polio syndrome. Sleep Med 37:147–150. https://doi.org/10.1016/j.sleep.2017.06.025
Chesson AL Jr, Wise M, Davila D, Johnson S, Littner M, Anderson WM, Hartse K, Rafecas J (1999) Practice parameters for the treatment of restless legs syndrome and periodic limb movement disorder. An American Academy of Sleep Medicine report. Standards of Practice Committee of the American Academy of Sleep Medicine. Sleep 22(7):961–968
Connor JR, Wang XS, Allen RP, Beard JL, Wiesinger JA, Felt BT, Earley CJ (2009) Altered dopaminergic profile in the putamen and substantia nigra in restless leg syndrome. Brain 132(Pt 9):2403–2412. https://doi.org/10.1093/brain/awp125
Thorpy MJ (2012) Classification of sleep disorders. Neurotherapeutics 9(4):687–701. https://doi.org/10.1007/s13311-012-0145-6
Turjanski N, Lees AJ, Brooks DJ (1999) Striatal dopaminergic function in restless legs syndrome: 18F-dopa and 11C-raclopride PET studies. Neurology 52(5):932–937. https://doi.org/10.1212/WNL.52.5.932
Bogan RK (2014) From bench to bedside: an overview of rotigotine for the treatment of restless legs syndrome. Clin Ther 36(3):436–455. https://doi.org/10.1016/j.clinthera.2014.01.021
Rohrer B, Stell WK (1995) Localization of putative dopamine D2-like receptors in the chick retina, using in situ hybridization and immunocytochemistry. Brain Res 695(2):110–116. https://doi.org/10.1016/0006-8993(95)00700-Z
Tian N, Xu HP, Wang P (2015) Dopamine D2 receptors preferentially regulate the development of light responses of the inner retina. Eur J Neurosci 41(1):17–30. https://doi.org/10.1111/ejn.12783
Dearry A, Edelman JL, Miller S, Burnside B (1990) Dopamine induces light-adaptive retinomotor movements in bullfrog cones via D2 receptors and in retinal pigment epithelium via D1 receptors. J Neurochem 54(4):1367–1378. https://doi.org/10.1111/j.1471-4159.1990.tb01971.x
Kafieh R, Rabbani H, Kermani S (2013) A review of algorithms for segmentation of optical coherence tomography from retina. J Med Signals Sens 3(1):45–60
Chorostecki J, Seraji-Bozorgzad N, Shah A, Bao F, Bao G, George E, Gorden V, Caon C, Frohman E, Bhatti MT, Khan O (2015) Characterization of retinal architecture in Parkinson’s disease. J Neurol Sci 355(1–2):44–48. https://doi.org/10.1016/j.jns.2015.05.007
Bittersohl D, Stemplewitz B, Keseru M, Buhmann C, Richard G, Hassenstein A (2015) Detection of retinal changes in idiopathic Parkinson’s disease using high-resolution optical coherence tomography and Heidelberg retina tomography. Acta Ophthalmol 93(7):e578–e584. https://doi.org/10.1111/aos.12757
Guler S, Nesrin Turan F (2015) Turkish version of the Johns Hopkins Restless Legs Syndrome Quality of Life Questionnaire (RLS-QoL): validity and reliability study. Qual Life Res Int J Qual Life Asp Treat Care Rehab 24(11):2789–2794. https://doi.org/10.1007/s11136-015-1003-x
Walters AS, LeBrocq C, Dhar A, Hening W, Rosen R, Allen RP, Trenkwalder C (2003) Validation of the International Restless Legs Syndrome Study Group rating scale for restless legs syndrome. Sleep Med 4(2):121–132. https://doi.org/10.1016/S1389-9457(02)00258-7
Koskderelioglu A, Kusbeci T, Kusbeci OY, Gedizlioglu M (2016) Optic nerve head, retinal nerve fiber layer and macular thickness analysis in restless legs syndrome. Parkinsonism Relat Disord 31:110–115. https://doi.org/10.1016/j.parkreldis.2016.08.003
Bara-Jimenez W, Aksu M, Graham B, Sato S, Hallett M (2000) Periodic limb movements in sleep: state-dependent excitability of the spinal flexor reflex. Neurology 54(8):1609–1616
Inzelberg R, Ramirez JA, Nisipeanu P, Ophir A (2004) Retinal nerve fiber layer thinning in Parkinson disease. Vis Res 44(24):2793–2797. https://doi.org/10.1016/j.visres.2004.06.009
Moschos MM, Tagaris G, Markopoulos I, Margetis I, Tsapakis S, Kanakis M, Koutsandrea C (2011) Morphologic changes and functional retinal impairment in patients with Parkinson disease without visual loss. Eur J Ophthalmol 21(1):24–29
Yu JG, Feng YF, Xiang Y, Huang JH, Savini G, Parisi V, Yang WJ, Fu XA (2014) Retinal nerve fiber layer thickness changes in Parkinson disease: a meta-analysis. PLoS One 9(1):e85718. https://doi.org/10.1371/journal.pone.0085718
Yavas GF, Yilmaz O, Kusbeci T, Ozturk F (2007) The effect of levodopa and dopamine agonists on optic nerve head in Parkinson disease. Eur J Ophthalmol 17(5):812–816
Carelli V, La Morgia C, Valentino ML, Barboni P, Ross-Cisneros FN, Sadun AA (2009) Retinal ganglion cell neurodegeneration in mitochondrial inherited disorders. Biochim Biophys Acta 1787(5):518–528. https://doi.org/10.1016/j.bbabio.2009.02.024
Mailankody P, Battu R, Khanna A, Lenka A, Yadav R, Pal PK (2015) Optical coherence tomography as a tool to evaluate retinal changes in Parkinson’s disease. Parkinsonism Relat Disord 21(10):1164–1169. https://doi.org/10.1016/j.parkreldis.2015.08.002
Frederick JM, Rayborn ME, Laties AM, Lam DM, Hollyfield JG (1982) Dopaminergic neurons in the human retina. J Comp Neurol 210(1):65–79. https://doi.org/10.1002/cne.902100108
Hirasawa H, Puopolo M, Raviola E (2009) Extrasynaptic release of GABA by retinal dopaminergic neurons. J Neurophysiol 102(1):146–158. https://doi.org/10.1152/jn.00130.2009
Djamgoz MB, Hankins MW, Hirano J, Archer SN (1997) Neurobiology of retinal dopamine in relation to degenerative states of the tissue. Vis Res 37(24):3509–3529. https://doi.org/10.1016/S0042-6989(97)00129-6
Garcia-Martin E, Larrosa JM, Polo V, Satue M, Marques ML, Alarcia R, Seral M, Fuertes I, Otin S, Pablo LE (2014) Distribution of retinal layer atrophy in patients with Parkinson disease and association with disease severity and duration. Am J Ophthalmol 157(2):470–478 e472. https://doi.org/10.1016/j.ajo.2013.09.028
Satue M, Obis J, Rodrigo MJ, Otin S, Fuertes MI, Vilades E, Gracia H, Ara JR, Alarcia R, Polo V, Larrosa JM, Pablo LE, Garcia-Martin E (2016) Optical coherence tomography as a biomarker for diagnosis, progression, and prognosis of neurodegenerative diseases. J Ophthalmol 2016:8503859. https://doi.org/10.1155/2016/8503859
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria, educational grants, participation in speakers’ bureaus, membership, employment, consultancies, stock ownership, or other equity interest, and expert testimony or patent-licensing arrangements) or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Kose Ozlece, H., Solmaz, V., Özal, S.A. et al. Do you have restless leg syndrome? I understood from your eyes. Sleep Breath 23, 551–557 (2019). https://doi.org/10.1007/s11325-018-1740-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-018-1740-5