Abstract
Purpose
Excessive daytime sleepiness (EDS) is a debilitating symptom which occurs commonly in both primary sleep and mood disorders. The prevalence of mood disorders in patients with EDS, evaluated objectively with a mean sleep latency test (MSLT), has not been reported. We hypothesize that mood disorders are highly prevalent in patients being investigated for EDS. This study aims to report the prevalence of mood disorder in the MSLT population and investigate the association between mood disorder and objective and subjective scores of sleepiness.
Methods
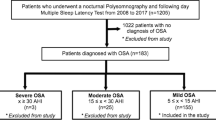
A retrospective multicenter study of adults with a MSLT and Hospital Anxiety and Depression Score (HADS) identified over a 3-year period. The HADS is a validated questionnaire in detecting depression (HADS-D ≥ 8) and anxiety (HADS-A ≥ 11) in the sleep clinic population. Data collected included demographics, medical, and sleep study information. Mood disorder prevalence was compared to the general sleep clinic population. Correlation between measures of sleepiness and mood was performed.
Results
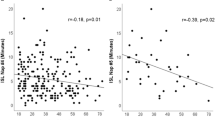
Two hundred twenty patients were included with mean age 41.1 ± 15.7 years, mean body mass index 28.6 kg/m2 of whom 30% had anxiety (HADS-A > 11) and 43% depression (HADS-D > 8). Mean results for the cohort are ESS 13.7, mean sleep latency 11.5 min, HADS-A 8.2, and HADS-D 7. There was no significant correlation between objective sleepiness, as measured by the mean sleep latency, and either HADS-A (−0.006, p = 0.93) or HADS-D score (0.002, p = 0.98). There was, however, a weak correlation between subjective sleepiness, as measured by the ESS, and the mean sleep latency (−0.25, p < 0.01), HADS-A (0.15, p = 0.03), and HADS-D (0.2, p = 0.004). There was no significant association between diagnosis of hypersomnia disorders and presence of anxiety (p = 0.71) or depression (p = 0.83).
Conclusions
Mood disorders are highly prevalent in the MSLT population. There was a weak correlation found between subjective measures of sleepiness and mood disorders, but not between objective measures of sleepiness and mood disorders. Routine screening for mood disorders in patients with hypersomnolence should be considered.

Similar content being viewed by others
References
Guilleminault CBS (2001) Excessive daytime sleepiness a challence for the practising neurologist. Brain 124:1482–1491
Swanson LMAJ, Rosekind MR et al (2011) Sleep disorders and work performance: findings from the 2008 National Sleep Foundation Sleep in America poll. J Sleep Res 20:487–494
Ohayon MM, Dauvilliers Y, Reynolds CF 3rd (2012) Operational definitions and algorithms for excessive sleepiness in the general population: implications for DSM-5 nosology. Arch Gen Psychiatry 69(1):71–79
Slater GSJ (2012) Excessive daytime sleepiness in sleep disorders. J Thorac Dis 4(6):608–616
Chervin RD (2000) Sleepiness, fatigue, tiredness, and lack of energy in obstructive sleep apnea. Chest 118(2):372–379
Cai SJ, Chen R, Zhang YL, Xiong KP, Lian YX, Li J et al (2013) Correlation of Epworth sleepiness scale with multiple sleep latency test and its diagnostic accuracy in assessing excessive daytime sleepiness in patients with obstructive sleep apnea hypopnea syndrome. Chin Med J 126(17):3245–3250
Leng PH, Low SY, Hsu A, Chong SF (2003) The clinical predictors of sleepiness correlated with the multiple sleep latency test in an Asian Singapore population. Sleep 26(7):878–881
Chervin RD, Aldrich MS, Pickett R, Guilleminault C (1997) Comparison of the results of the Epworth sleepiness scale and the multiple sleep latency test. J Psychosom Res 42(2):145–155
Thorpy MJ (1992) The clinical use of the multiple sleep latency test. The standards of practice Committee of the American Sleep Disorders Association. Sleep 15(3):268–276
Carskadon MA, Dement WC, Mitler MM, Roth T, Westbrook PR, Keenan S (1986) Guidelines for the multiple sleep latency test (MSLT): a standard measure of sleepiness. Sleep 9(4):519–524
Aldrich MS, Chervin RD, Malow BA (1997) Value of the multiple sleep latency test (MSLT) for the diagnosis of narcolepsy. Sleep 20(8):620–629
Coelho FNM, Murray B (2011) Testing sleepiness and vigilance in the sleep laboratory. Curr Opin Pulm Med 17(6):406–411
Scammell TE (2015) Narcolepsy. N Engl J Med 373(27):2654–2662
Billiard M, Sonka K (2016) Idiopathic hypersomnia. Sleep Med Rev 29:23–33
Launois SHTR, Levy P, Pepin JL (2013) On treatment but still sleepy: cause and management of residual sleepiness in obstructive sleep apnea. Curr Opin Pulm Med 19(6):601–608
Law M, Naughton MT, Dhar A, Barton D, Dabscheck E (2014) Validation of two depression screening instruments in a sleep disorders clinic. J Clin Sleep Med 10(6):683–688
Millman RP, Fogel BS, McNamara ME, Carlisle CC (1989) Depression as a manifestation of obstructive sleep apnea: reversal with nasal continuous positive airway pressure. J Clin Psychiatry 50(9):348–351
Mosko S, Zetin M, Glen S, Garber D, DeAntonio M, Sassin J et al (1989) Self-reported depressive symptomatology, mood ratings, and treatment outcome in sleep disorders patients. J Clin Psychol 45(1):51–60
Ejaz SM, Khawaja IS, Bhatia S, Hurwitz TD (2011) Obstructive sleep apnea and depression: a review. Innov Clin Neurosci 8(8):17–25
Douglas N, Young A, Roebuck T, Ho S, Miller BR, Kee K et al (2013) Prevalence of depression in patients referred with snoring and obstructive sleep apnoea. Intern Med J 43(6):630–634
Bardwell WAMP, Ancoli-Isreal S, Dimsdale JE (2003) Fatigue in obstructive sleep apnea: driven by depressive symptoms instead of apnea severity? Am J Psychiatry 160(2):350–355
Plante DT (2015) Hypersomnia in mood disorders: a rapidly changing landscape. Curr Sleep Med Rep 1(2):122–130
Kaplan KA, Harvey AG (2009) Hypersomnia across mood disorders: a review and synthesis. Sleep Medicine Reviews 13(4):275–285
Bixler EO, Vgontzas AN, Lin H-M, Calhoun SL, Vela-Bueno A, Kales A (2005) Excessive daytime sleepiness in a general population sample: the role of sleep apnea, age, obesity, diabetes, and depression. J Clin Endocrinol Metab 90(8):4510–4515
Chai-Coetzer CDJ, McEvoy D, Naughton M, Neill A, Rochford P, Wheatley J, Worsnop C (2014) Guidelines for Sleep Studies in Adults. Australasian Sleep Association, Australia
Littner MR, Kushida C, Wise M, Davila DG, Morgenthaler T, Lee-Chiong T, Hirshkowitz M et al (2005) Practice parameters for clinical use of the multiple sleep latency test and the maintenance of wakefulness test. Sleep 28(1):113–121
Ruoff C, Rye D (2016) The ICSD-3 and DSM-5 guidelines for diagnosing narcolepsy: clinical relevance and practicality. Curr Med Res Opin:1–12
Sateia MJ (2014) International classification of sleep disorders-third edition: highlights and modifications. Chest 146(5):1387–1394
Hillman DR, Murphy AS, Pezzullo L (2006) The economic cost of sleep disorders. Sleep 29(3):299–305
Australian Bureau of Statistics (2007) National Survey of Mental Health and Wellbeing: summary of results. ABS, Canberra
Breslau N, Roth T, Rosenthal L, Andreski P (1996) Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biol Psychiatry 39(6):411–418
Acknowledgements
This study was a retrospective multicenter study of the Institute for Breathing and Sleep, Austin Hospital, Melbourne and Sleep Department, Alfred Hospital, Melbourne.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
For this type of study formal consent is not required. However, the study was approved by the Human Research Ethics Committees at both Institutions.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Denton, E.J., Barnes, M., Churchward, T. et al. Mood disorders are highly prevalent in patients investigated with a multiple sleep latency test. Sleep Breath 22, 305–309 (2018). https://doi.org/10.1007/s11325-017-1572-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-017-1572-8