Abstract
Purpose
To determine independent relationship of aging with chronic intermittent hypoxia, we compared hypoxia-related polysomnographic variables of geriatric patients (aged ≥ 65 years) with an apnea–hypopnea index (AHI)-, gender-, body mass index (BMI)-, and neck circumference-matched cohort of non-geriatric patients.
Methods
The study was conducted using clinical and polysomnographic data of 1280 consecutive patients who underwent complete polysomnographic evaluation for suspected sleep-disordered breathing (SDB) at a single sleep disorder center. A propensity score-matched analysis was performed to obtain matched cohorts of geriatric and non-geriatric patients, which resulted in successful matching of 168 patients from each group.
Results
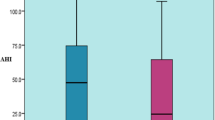
Study groups were comparable for gender (P = 0.999), BMI (P = 0.940), neck circumference (P = 0.969), AHI (P = 0.935), and severity of SDB (P = 0.089). The oximetric variables representing the duration of chronic intermittent hypoxia such as mean (P = 0.001), the longest (P = 0.001) and total apnea durations (P = 0.003), mean (P = 0.001) and the longest hypopnea durations (P = 0.001), and total sleep time with oxygen saturation below 90% (P = 0.008) were significantly higher in the geriatric patients as compared with younger adults. Geriatric patients had significantly lower minimum (P = 0.013) and mean oxygen saturation (P = 0.001) than non-geriatric patients.
Conclusions
The study provides evidence that elderly patients exhibit more severe and deeper nocturnal intermittent hypoxia than the younger adults, independent of severity of obstructive sleep apnea, BMI, gender, and neck circumference. Hypoxia-related polysomnographic variables in geriatric patients may in fact reflect a physiological aging process rather than the severity of a SDB.

Similar content being viewed by others
References
Guilleminault C, Ramar K (2009) Neurologic aspects of sleep apnea: is obstructive sleep apnea a neurologic disorder? Semin Neurol 29:368–371
Garvey JF, Pengo MF, Drakatos P, Kent BD (2015) Epidemiological aspects of obstructive sleep apnea. J Thorac Dis 7:920–929
Prabhakar NR, Kumar GK (2004) Oxidative stress in the systemic and cellular responses to intermittent hypoxia. Biol Chem 385:217–221
Lavie L (2003) Obstructive sleep apnoea syndrome—an oxidative stress disorder. Sleep Med Rev 7:35–51
Bostanci A, Turhan M, Bozkurt S (2015) Factors influencing sleep time with oxygen saturation below 90% in sleep-disordered breathing. Laryngoscope 125:1008–1012
Heinzer R, Vat S, Marques-Vidal P, Marti-Soler H, Andries D, Tobback N, Mooser V, Preisig M, Malhotra A, Waeber G, Vollenweider P, Tafti M, Haba-Rubio J (2015) Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med 3:310–318
Kawaguchi Y, Fukumoto S, Inaba M, Koyama H, Shoji T, Shoji S, Nishizawa Y (2011) Different impacts of neck circumference and visceral obesity on the severity of obstructive sleep apnea syndrome. Obesity (Silver Spring) 19:276–282
Tishler PV, Larkin EK, Schluchter MD, Redline S (2003) Incidence of sleep-disordered breathing in an urban adult population: the relative importance of risk factors in the development of sleep-disordered breathing. JAMA 289:2230–2237
Hongyo K, Ito N, Yamamoto K, Yasunobe Y, Takeda M, Oguro R, Takami Y, Takeya Y, Sugimoto K, Rakugi H (2017) Factors associated with the severity of obstructive sleep apnea in older adults. Geriatr Gerontol Int 17:614–621
Lavie P, Lavie L (2009) Unexpected survival advantage in elderly people with moderate sleep apnoea. J Sleep Res 18:397–403
Sforza E, Roche F (2016) Chronic intermittent hypoxia and obstructive sleep apnea: an experimental and clinical approach. Hypoxia (Auckl) 4:99–108
Hua-Huy T, Rouhani S, Nguyen XY, Luchon L, Meurice JC, Dinh-Xuan AT (2015) Cardiovascular comorbidities in obstructive sleep apnoea according to age: a sleep clinic population study. Aging Clin Exp Res 27:611–619
McMillan A, Morrell MJ (2016) Sleep disordered breathing at the extremes of age: the elderly. Breathe (Sheff) 12:50–60
Chiang AA (2006) Obstructive sleep apnea and chronic intermittent hypoxia: a review. Chin J Phys 49:234–243
Wang X, Ouyang Y, Wang Z, Zhao G, Liu L, Bi Y (2013) Obstructive sleep apnea and risk of cardiovascular disease and all-cause mortality: a meta-analysis of prospective cohort studies. Int J Cardiol 169:207–214
Kendzerska T, Gershon AS, Hawker G, Tomlinson G, Leung RS (2014) Obstructive sleep apnea and incident diabetes. A historical cohort study. Am J Respir Crit Care Med 190:218–225
Malhotra A, Huang Y, Fogel R, Lazic S, Pillar G, Jakab M, Kikinis R, White DP (2006) Aging influences on pharyngeal anatomy and physiology: the predisposition to pharyngeal collapse. Am J Med 119:72.e9–72.14
Punjabi NM, Caffo BS, Goodwin JL, Gottlieb DJ, Newman AB, O'Connor GT, Rapoport DM, Redline S, Resnick HE, Robbins JA, Shahar E, Unruh ML, Samet JM (2009) Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med 6:e1000132
Lavie P, Lavie L, Herer P (2005) All-cause mortality in males with sleep apnoea syndrome: declining mortality rates with age. Eur Respir J 25:514–520
Marti S, Sampol G, Muñoz X, Torres F, Roca A, Lloberes P, Sagalés T, Quesada P, Morell F (2002) Mortality in severe sleep apnoea/hypopnoea syndrome patients: impact of treatment. Eur Respir J 20:1511–1518
Yellon DM, Alkhulaifi AM, Pugsley WB (1993) Preconditioning the human myocardium. Lancet 342:276–277
Kloner RA, Jennings RB (2001) Consequences of brief ischemia: stunning, preconditioning, and their clinical implications: part 1. Circulation 104:2981–2989
Eckert DJ, Catcheside PG, Smith JH, Frith PA, McEvoy RD (2004) Hypoxia suppresses symptom perception in asthma. Am J Respir Crit Care Med 169:1224–1230
Neubauer JA, Melton JE, Edelman NH (1990) Modulation of respiration during brain hypoxia. J Appl Physiol (1985) 68:441–451
Quintero M, Olea E, Conde SV, Obeso A, Gallego-Martin T, Gonzalez C, Monserrat JM, Gómez-Niño A, Yubero S, Agapito T (2016) Age protects from harmful effects produced by chronic intermittent hypoxia. J Physiol 594:1773–1790
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Bostanci, A., Bozkurt, S. & Turhan, M. Impact of age on intermittent hypoxia in obstructive sleep apnea: a propensity-matched analysis. Sleep Breath 22, 317–322 (2018). https://doi.org/10.1007/s11325-017-1560-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-017-1560-z