Abstract
Aim
Willis-Ekbom disease (RLS/WED) is common in chronic obstructive pulmonary disease (COPD). Patients with RLS/WED have poorer quality of sleep and more fatigue and depressive symptoms. The prevalence of RLS/WED in patients with COPD has been reported to vary between 29.1 and 36.8 %. However, during exacerbation, the prevalence can increase up to 54 %. These rates are higher than those seen in general population. We have not enough knowledge regarding the association between RLS and COPD. In this study, we aimed to determine the frequency of RLS in patients with stable COPD without comorbid conditions. In addition, we also aimed to determine possible related causative factors.
Method
We included 80 COPD patients without comorbid conditions who presented to our outpatient clinic between April 2013 and September 2013 for RLS/WED evaluation. Three cases that have polyneuropathy and one case that refused undergoing electromyography (EMG) examination were excluded from the study. Demographic data, P-A chest X-rays, pulmonary function tests (PFT), biochemical parameters (including hemogram), and dyspnea scales were evaluated for each patient. In addition, the RLS/WED rating scale and Epworth Sleep Scale (ESS) were applied. Further, each patient diagnosed with RLS/WED underwent a detailed neurological examination (performed by a neurologist) and an EMG examination to rule out polyneuropathy.
Results
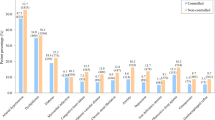
Out of 76 COPD cases included in our study, 26.3 % (n = 20) were diagnosed with RLS/WED (mean age 60.4 ± 7.5 years, 20 males). The cases with RLS/WED had significantly lower body mass index (BMI) than cases without RLS/WED (p = 0.009). There were no significant differences between cases with and without RLS/WED with respect to PFT, dyspnea scales, and arterial blood gas values. However, ESS was significantly different (p = 0.016). There were no significant differences in RLS/WED scores and mean hs-CRP levels between COPD stages (p = 0.424; p = 0.518, respectively), while ESS was significantly different (p = 0.016). ESS was significantly higher in stage B COPD than in stages A and D (p = 0.005, p = 0.008, respectively). Based on our model, we found that exacerbations and iron binding capacity (UIBC) were predictive factors for RLS/WED (p < 0.100)
Conclusion
RLS/WED is a common disease in cases with stable COPD. Despite our hypothesis suggesting that the prevalence of RLS/WED in COPD is related with systemic inflammation, we did not find a significant association between hs-CRP and COPD cases with RLS/WED. However, we did find that UIBC is a predictive factor for the development of RLS/WED. Nonetheless, further studies are needed to understand the relationships between UIBC, low BMI, and the development of RLS/WED in COPD.



Similar content being viewed by others
References
Vestbo J, Hurd SS, Rodriguez-Roisin R (2012) The 2011 revision of the global strategy for the diagnosis, management and prevention of COPD (GOLD)—why and what? Clin Respir J 6(4):208–214. doi:10.1111/crj.12002
Barnes PJ, Celli BR (2009) Systemic manifestations and comorbidities of COPD. Eur Respir J 33(5):1165–1185. doi:10.1183/09031936.00128008
Trenkwalder C, Paulus W, Walters AS (2005) The restless legs syndrome. Lancet Neurol 4(465-475):1165–1185. doi:10.1183/09031936.ERS
Earley CJ, Connor J, Garcia-Borreguero D, Jenner P, Winkelman J, Zee PC, Allen R (2014) Altered brain iron homeostasis and dopaminergic function in Restless Legs Syndrome (Willis-Ekbom disease). Sleep Med 15(11):1288–1301. doi:10.1016/j.sleep
Allen RP, Picchietti D, Hening WA, Trenkwalder C, Walters AS, Montplaisir J (2003) Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology. Sleep Med 4:101–119
Walters AS LeBrocq C, Dhar A, Hening W, Rosen R, Allen RP, Trenkwalder C, International Restless Legs Syndrome Study Group (2003) Validation of the International Restless Legs Syndrome Study Group rating scale for restless legs syndrome. Sleep Med 4(2):121–132
Allen RP, Walters AS, Montplaisir J, Hening W, Myers A, Bell TJ, Ferini-Strambi L (2005) Restless legs syndrome prevalence and impact: REST general population study. Arch Intern Med 13 165(11):1286–1292
Högl B, Kiechl S, Willeit J, Saletu M, Frauscher B, Seppi K, Müller J, Rungger G, Poewe W (2005) Restless legs syndrome: a community-based study of prevalence, severity and risk factors. Neurology 64(11):1920–1924
Hening W, Walters AS, Allen RP, Montplaisir J, Myers A, Ferini-Strambi L (2004) Impact, diagnosis and treatment of restless legs syndrome (RLS) in a primary care population: the REST (RLS Epidemiology, Symptoms, and Treatment) primary care study. Sleep Med 5(3):237–246
Garcia-Borreguero D (2006) Time to REST; epidemiology and burden. Eur J Neurol 13(suppl 3):15–20
Aras G, Kadakal F, Purisa S, Kanmaz D, Aynaci A, Isik E (2011) Are we aware of restless leg syndrome in COPD patient who are in an exaceration period? Frequency and probable factors are related to underlying mechanism. COPD 8(6):437–443
Hening WA (2007) Current guidelines and standards of practice for restless legs syndrome. Am J Med 120(1):522–527
Yüksel G, Varlıbaşı F, Karlıkaya G, Tireli H (2006) Huzursuz bacaklar sendromu; Klinik ve Demografik değerlendirme. Parkinson Hastalığı ve Hareket Bozuklukları Dergisi 9(2):94–103
Lo Coco D, Mattalino A, Lo Coco A, Randisi B (2009) İncreased frequency of restless leg syndrome in chronic obstructive pulmonary disease patients. Sleep Med 10(5):572–576
Kaplan Y, İnonu H, Yilmaz A, Ocal S (2008) Restless leg syndrome in patients with chronic obstructive pulmonary disease. Can J Neurol Sci 35(3):352–357
Benediktsdottir B, Janson C, Lindberg E, Arnardóttir ES, Olafsson I, Cook E, Thorarinsdottir EH, Gislason T (2010) Prevalence of restless legs syndrome among adults in Iceland and Sweden: lung function, comorbidity, ferritin, biomarkers and quality of life. Sleep Med 11(10):1043–1048
de Godoy I, Donahoe M, Calhoun WJ, Mancino J, Rogers RM (1996) Elevated TNF-alpha production by peripheral blood monocytes of weight-losing COPD patients. Am J Respir Crit Care Med 153(2):633–637
Means RT Jr, Dessypris EN, Krantz SB (1992) Inhibition of human erythroid colony-forming units by interleukin-1 is mediated by gamma interferon. J Cell Physiol 150:59–64
Allen DA, Breen C, Yaqoob MM, Macdougall IC (1999) Inhibition of CFU-E colony formation in uremic patients with inflammatory disease: role of IFN-gamma and TNF-alpham. J Investig Med 47:204–211
Cavalcante AG, de Bruin PF, de Bruin VM, Pereira ED, Cavalcante MM, Nunes DM, Viana CS (2012) Restless legs syndrome, sleep impairment, and fatigue in chronic obstructive pulmonary disease. Sleep Med 13(7):842–847. doi:10.1016/j.sleep.2012.03.017
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Study funding
This study was not any financially supported.
Conflict of interest
The investigation was performed at the sleep laboratory of the Department of Chest Diseases, Yedikule Chest Diseases, and Chest Surgery Training and Research Hospital. The work has been seen and approved by all co-authors. The authors have no proprietary, financial, professional, or other personal interest of any nature or kind in any product, service, and/or company that could be construed as influencing the position presented in, or the review of, the manuscript.
Ethical approval
Local Ethics Committee approval was taken for the study.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
The manuscript entitled “To What Extent and Why Are COPD and Willis-Ekbom Disease Associated?” which we submit for consideration to be published in Journal of Sleep and Breathing is not under consideration for publication or published elsewhere.
Comment
This is the first study looking into detail at the predictors of restless legs syndrome in stable COPD patients without comorbidities. They confirm a very high prevalence of restless legs although a rather young study population. Iron reserve, but not inflammation is contributing to its genesis, in the absence of traditional organic risk factors.
Johan Verbraecken
Antwerp, Belgium
Rights and permissions
About this article
Cite this article
Mandal, T., Aydın, Ş., Kanmaz, D. et al. To what extent and why are COPD and Willis-Ekbom disease associated?. Sleep Breath 20, 1021–1027 (2016). https://doi.org/10.1007/s11325-016-1359-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-016-1359-3