Abstract
Purpose
The purposes of the present study are to determine the prevalence and demographic features of rapid eye movement (REM)-related sleep-disordered breathing (SDB) in Korean adults with newly diagnosed obstructive sleep apnea (OSA) and determine if REM-related SDB is associated with depressive symptoms and health-related quality of life (HRQoL) in OSA patients.
Methods
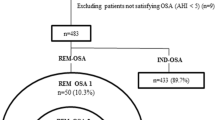
In this cross-sectional study, we evaluated 1281 OSA adults who were consecutively recruited. REM-related SDB was defined as an overall apnea-hypopnea index (AHI) ≥5, an AHINREM <15, and AHIREM to AHINREM ratio of >2. The Epworth Sleepiness Scale (ESS), Beck Depression Inventory (BDI), and Medical Outcomes Study Short-Form Health survey (SF-36) were used to evaluate all patients. Multiple regression analyses were performed to determine the associations between REM-related SDB and clinical outcomes.
Results
The prevalence of REM-related SDB was 18 % in this study. REM-related SDB was more commonly observed in patients with mild or moderate OSA (p < 0.001) and women (p < 0.001). The linear regression analysis showed that the presence of REM-related SDB was significantly associated with higher BDI scores, but only in men. AHIREM was positively associated with the BDI scores, but only in men with REM-related SDB. There were no differences in ESS and SF-36 scores between patients with and without REM-related SDB.
Conclusions
Patients with REM-related SDB account for 18 % of Korean OSA adults. REM-related SDB was associated with depressive symptoms, but only in men. AHIREM is positively related to the degree of depressive symptoms in men with REM-related SDB.
Similar content being viewed by others
References
Kass JE, Akers SM, Bartter TC, Pratter MR (1996) Rapid-eye movement-specific sleep-disordered breathing: a possible cause of excessive daytime sleepiness. Am J Respir Crit Care Med 154:167–169
Koo B, Dostal J, Ioachimescu O, Budur K (2008) The effects of gender and age on REM-related sleep-disordered breathing. Sleep Breath 12:257–264
Katz E, White D (2004) Genioglossus activity during sleep in normal control subjects and children with obstructive sleep apnea. Am J Respir Crit Care Med 170:553–560
Smith CA, Henderson KS, Xi L, Chow CM, Eastwood PR, Dempsey JA (1997) Neural-mechanical coupling of breathing in REM sleep. J Appl Phys 83:1923–1932
Series F, Cormier Y, La Forge J (1990) Influence of apnea type and sleep stage on nocturnal postapneic desaturation. Am Rev Respir Dis 141:1522–1526
Conwell W, Patel B, Doeing D, Pamidi S, Knutson KL, Ghods F, Mokhlesi B (2012) Prevalence, clinical features, and CPAP adherence in REM-related sleep-disordered breathing: a cross-sectional analysis of a large clinical population. Sleep Breath 16:519–526
Haba-Rubio J, Janssens JP, Rochat T, Sforza E (2005) Rapid eye movement-related disordered breathing: clinical and polysomnographic features. Chest 128:3350–3357
O’Connor C, Thornley KS, Hanly PJ (2000) Gender differences in the polysomnographic features of obstructive sleep apnea. Am J Respir Crit Care Med 161:1465–1472
Koo BB, Patel SR, Strohl K, Hoffstein V (2008) Rapid eye movement related sleep-disordered breathing: influence of age and gender. Chest 134:1156–1161
Chervin RD, Aldrich MS (1998) The relation between multiple sleep latency test findings and the frequency of apneic events in REM and non-REM sleep. Chest 113:980–984
Punjabi NM, Bandeen-Roche K, Marx JJ, Neubauer DN, Smith PL, Schwartz AR (2002) The association between daytime sleepiness and sleep-disordered breathing in NREM and REM sleep. Sleep 25:307–314
Chami HA, Baldwin CM, Silverman A, Zhang Y, Rapoport D, Punjabi N, Gottlieb DJ (2010) Sleepiness, quality of life, and sleep maintenance in REM versus non-REM sleep-disordered breathing. Am J Respir Crit Care Med 181:997–1002
Ohayon MM (2003) The effects of breathing-related sleep disorders on mood disturbances in the general population. J Clin Psychiatry 64:1195–1200
Sharafkhaneh A, Giray N, Richardson P, Young T, Hirshkowitz M (2005) Association of psychiatric disorders and sleep apnea in a large cohort. Sleep 28:1405–1411
Lee YH, Song JY (1991) A study of the reliability and the validity of the BDI, SDS, and MMPI-D scales. J Korean Neuropsychiatr Assoc 10:93–113
American Academy of Sleep Medicine (2007) The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. Westchester, IL
Cho YW, Lee JH, Son HK, Lee SH, Shin C, Johns MW (2011) The reliability and validity of the Korean version of the Epworth Sleepiness Scale. Sleep Breath 15:377–384
Han CW, Lee EJ, Iwaya T, Kataoka H, Kohzuki M (2004) Development of the Korean version of Short-Form 36-Item Health Survey: health related QOL of healthy elderly people and elderly patients in Korea. Tohoku J Exp Med 203:189–194
Sakao S, Sakurai T, Yahaba M, Sakurai Y, Terada J, Tanabe N, Tatsumi K (2015) Features of REM-related sleep disordered breathing in the Japanese population. Intern Med 54:1481–1487
Li KK, Kushida C, Powell NB, Riley RW, Guilleminault C (2000) Obstructive sleep apnea syndrome: a comparison between Far-East Asian and white men. Laryngoscope 110:1689–1693
Glovinsky P, Glovinsky PB, Spielman AJ, Carroll P, Weinstein L, Ellman SJ (1990) Sleepiness and REM sleep recurrence: the effects of stage 2 and REM sleep awakenings. Psychophysiology 27:552–559
Nykamp K, Rosenthal L, Folkerts M, Roehrs T, Guido P, Roth T (1998) The effect of REM sleep deprivation on the level of sleepiness/alertness. Sleep 21:609–614
Armitage R (2007) Sleep and circadian rhythms in mood disorders. Acta Psychiatr Scand 115(Suppl 433):S104–S115
Gottesmann C, Gottesman I (2007) The neurobiological characteristics of rapid eye movement (REM) sleep are candidate endophenotypes of depression, schizophrenia, mental retardation and dementia. Prog Neurobiol 81:237–250
Palagini L, Baglioni C, Ciapparelli A, Gemignani A, Riemann D (2013) REM sleep dysregulation in depression: state of the art. Sleep Med Rev 17:377–390
Kessler RC, McGonagle KA, Swartz M, Blazer DG, Nelson CB (1993) Sex and depression in the National Comorbidity Survey. I: lifetime prevalence, chronicity and recurrence. J Affect Disord 29:85–96
Shochat T, Umphress J, Israel AG, Ancoli-Israel S (1999) Insomnia in primary care patients. Sleep 22(Suppl 2):S359–S365
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
No funding was received for this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements) or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Lee, SA., Paek, JH. & Han, SH. REM-related sleep-disordered breathing is associated with depressive symptoms in men but not in women. Sleep Breath 20, 995–1002 (2016). https://doi.org/10.1007/s11325-016-1323-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-016-1323-2