Abstract
Purpose
To assess the physiological meanings of the detrended fluctuation analysis (DFA) slope α and its relationship to spectral measures in heart rate variability, this study investigated changes of α and its corresponding spectral measures over various night-sleep stages.
Methods
The overall DFA α and natural-logarithm-transformed power values of the spectral parameters ln[high-frequency (HF)], ln[low-frequency (LF)], and ln[very-low-frequency (VLF)], and their relationship from one 5-min proper electrocardiography segment in each of pre-sleep-wakefulness (AWK), non-rapid eye movement stage 2 (N2), slow-wave (N3), the first and the latest rapid-eye movement sleep (REM1, and REM2), were computed in 93 otherwise healthy males (44.1 ± 7.7 years.) with wide-ranged apnea-hypopnea, periodic-limb movement and arousal indices (19.0 ± 20.9, 4.7 ± 9.9, and 10.7 ± 18.2 h, respectively).
Results
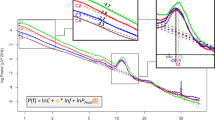
While ln(HF) dipped from AWK, N2, and N3 to REM1 then rebounded to the origin level at REM2, ln(VLF) dipped from AWK to N2, N3 trough, and then surged to levels surpassing AWKs and N2s at REM1 and REM2. ln(LF/HF), ln(VLF/HF), and α dipped from AWK and N2 to N3 trough, surged to levels surpassing AWKs, and N2s at REM1 then became attenuated at REM2. By general linear modeling, the relationship between α and the corresponding spectral values can be seen over various stages as α = b 0 + 0.147 × ln(VLF/HF) (R 2 = 0.766), regardless of age and sleep-sympathoexcitatory episodes.
Conclusion
The REM sleep attenuations appeared in ln(HF) and its derivatives, such as ln(LF/HF), ln(VLF/HF), and the overall DFA slope α values. The quantitative function of ln(VLF/HF) describes the α values constantly for overnight sleep stages, and it is not affected by age, LF, PLM, and AHI. Our findings therefore suggest that in sleep studies with spectral HRV measures, ln(VLF/HF) as a surrogate of the overall DFA slope α should be calculated at the same time.



Similar content being viewed by others
References
Zipes DP, Wellens HJ (1998) Sudden cardiac death. Circulation 98:2334–2351
Malik M (1996) Heart rate variability: standards of measurement, physiological interpretation and clinical use task force of the european society of cardiology and the north american society of pacing and electrophysiology. Circulation 93:1043–1065
Taylor JA, Carr DL, Myers CW, Eckberg DL (1998) Mechanisms underlying very-low-frequency RR-interval oscillations in humans. Circulation 98:547–555
Berlad II, Shlitner A, Ben-Haim S, Lavie P (1993) Power spectrum analysis and heart rate variability in stage 4 and REM sleep: evidence for state-specific changes in autonomic dominance. J Sleep Res 2:88–90
Bonsignore MR, Romano S, Marrone O, Chiodi M, Bonsignore G (1997) Different heart rate patterns in obstructive apneas during NREM sleep. Sleep 20:1167–1174
Sforza E, Pichot V, Barthelemy JC, Haba-Rubio J, Roche F (2005) Cardiovascular variability during periodic leg movements: a spectral analysis approach. Clin Neurophysiol 116:1096–1104
Huikuri HV, Perkiomaki JS, Maestri R, Pinna GD (2009) Clinical impact of evaluation of cardiovascular control by novel methods of heart rate dynamics. Philos Trans A Math Phys Eng Sci 367:1223–1238
Francis DP, Willson K, Georgiadou P, Wensel R, Davies LC, Coats A, et al. (2002) Physiological basis of fractal complexity properties of heart rate variability in man. J Physiol 542:619–629
Beckers F, Verheyden B, Aubert AE (2006) Aging and nonlinear heart rate control in a healthy population. Am J Physiol Heart Circ Physiol 290:H2560–H2570
Hu K, Ivanov P, Hilton MF, Chen Z, Ayers RT, Stanley HE, et al. (2004) Endogenous circadian rhythm in an index of cardiac vulnerability independent of changes in behavior. Proc Natl Acad Sci U S A 101:18223–18227
Hu K, Scheer FA, Buijs RM, Shea SA (2008) The circadian pacemaker generates similar circadian rhythms in the fractal structure of heart rate in humans and rats. Cardiovasc Res 80:62–68
Takabatake N, Nakamura H, Minamihaba O, Inage M, Inoue S, Kagaya S, et al. (2001) A novel pathophysiologic phenomenon in cachexic patients with chronic obstructive pulmonary disease: the relationship between the circadian rhythm of circulating leptin and the very low-frequency component of heart rate variability. Am J Respir Critical Care Med 163:1314–1319
Burgess HJ, Trinder J, Kim Y, Luke D (1997) Sleep and circadian influences on cardiac autonomic nervous system activity. Am J Physiol 273:H1761–H1768
Hilton MF, Umali MU, Czeisler CA, Wyatt JK, Shea SA (2000) Endogenous circadian control of the human autonomic nervous system. Comput Cardiol 27:197–200
Schumann AY, Bartsch RP, Penzel T, Ivanov P, Kantelhardt JW (2010) Aging effects on cardiac and respiratory dynamics in healthy subjects across sleep stages. Sleep 33:943–955
Kuo TB, Yang CC (2004) Scatterplot analysis of EEG slow-wave magnitude and heart rate variability: an integrative exploration of cerebral cortical and autonomic functions. Sleep 27:648–656
Tan CO, Cohen MA, Eckberg DL, Taylor JA (2009) Fractal properties of human heart period variability: physiological and methodological implications. J Physiol 587:3929–3941
Penzel T, Kantelhardt JW, Lo CC, Voigt K, Vogelmeier C (2003) Dynamics of heart rate and sleep stages in normals and patients with sleep apnea. Neuropsychopharmacol Off Publ Am College Neuropsychopharmacol 28(Suppl 1):S48–S53
Heitmann A, Huebner T, Schroeder R, Perz S, Voss A (2011) Multivariate short-term heart rate variability: a pre-diagnostic tool for screening heart disease. Med Biol Eng Comput 49:41–50
Deboer T, Vansteensel MJ, Detari L, Meijer JH (2003) Sleep states alter activity of suprachiasmatic nucleus neurons. Nat Neurosci 6:1086–1090
Ting H, Lo HS, Chang SY, Chung AH, Kuan PC, Yuan SC, et al. (2009) Post- to pre-overnight sleep systolic blood pressures are associated with sleep respiratory disturbance, pro-inflammatory state and metabolic situation in patients with sleep-disordered breathing. Sleep Med 10:720–725
Askew EW (2002) Work at high altitude and oxidative stress: antioxidant nutrients. Toxicology 180:107–119
Bunde A, Havlin S, Kantelhardt JW, Penzel T, Peter JH, Voigt K (2000) Correlated and uncorrelated regions in heart-rate fluctuations during sleep. Phys Rev Lett 85:3736–3739
Penzel T, Wessel N, Riedl M, Kantelhardt JW, Rostig S, Glos M, et al. (2007) Cardiovascular and respiratory dynamics during normal and pathological sleep. Chaos 17:015116
da Silva EL, Pereira R, Reis LN, Pereira VL Jr., Campos LA, Wessel N, et al. (2015) Heart rate detrended fluctuation indexes as estimate of obstructive sleep apnea severity. Medicine 94:e516
Kryger MH, Roth T, Dement WC, Borbély AA (2011) Sleep Homeostasis and Models of Sleep Regulation. In Principles and Practice of Sleep Medicine 5th edn. 431–44.
Hu K, Van Someren EJ, Shea SA, Scheer FA (2009) Reduction of scale invariance of activity fluctuations with aging and Alzheimer’s disease: involvement of the circadian pacemaker. Proc Natl Acad Sci U S A 106:2490–2494
van Eekelen AP, Houtveen JH, Kerkhof GA (2004) Circadian variation in base rate measures of cardiac autonomic activity. Eur J Appl Physiol 93:39–46
Fleisher LA, Frank SM, Sessler DI, Cheng C, Matsukawa T, Vannier CA (1996) Thermoregulation and heart rate variability. Clin Sci (Lond) 90:97–103
Krauchi K (2007) The human sleep-wake cycle reconsidered from a thermoregulatory point of view. Physiol Behav 90:236–245
Di Rienzo M, Parati G, Castiglioni P, Omboni S, Ferrari AU, Ramirez AJ, et al. (1991) Role of sinoaortic afferents in modulating BP and pulse-interval spectral characteristics in unanesthetized cats. Am J Physiol 261:H1811–H1818
Bigger JT Jr., Fleiss JL, Steinman RC, Rolnitzky LM, Kleiger RE, Rottman JN (1992) Frequency domain measures of heart period variability and mortality after myocardial infarction. Circulation 85:164–171
Bigger JT, Fleiss JL, Rolnitzky LM, Steinman RC (1993) The ability of several short-term measures of RR variability to predict mortality after myocardial infarction. Circulation 88:927–934
Penzel T, Kantelhardt JW, Grote L, Peter JH, Bunde A (2003) Comparison of detrended fluctuation analysis and spectral analysis for heart rate variability in sleep and sleep apnea. IEEE Trans on Biomed Eng 50:1143–1150
Acknowledgments
We thank Dr. Tim Williams for his support throughout the editing process.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
All procedures performed in studies involving human.
participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Funding
The National Science Council, Taiwan provided financial support in the form of 98–2314-B-040-001-MY3 funding.
Taiwan Department of Health Clinical Trial and Research Center of Excellence provided financial support in the form of DOH102-TD-B-111-004 funding.
Additional information
Ren-Jing Huang, Ching-Hsiang Lai and Shin-Da Lee this authors contributed equally
Rights and permissions
About this article
Cite this article
Huang, RJ., Lai, CH., Lee, SD. et al. Scaling exponent values as an ordinary function of the ratio of very low frequency to high frequency powers in heart rate variability over various sleep stages. Sleep Breath 20, 975–985 (2016). https://doi.org/10.1007/s11325-016-1320-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-016-1320-5