Abstract
Purpose
Adenocarcinoma of the pancreas remains one of the most lethal human cancers. The high mortality rates associated with this form of cancer are subsequent to late-stage clinical presentation and diagnosis, when surgery is rarely possible and of modest chemotherapeutic impact. Survival rates following diagnosis with advanced pancreatic cancer are very low; typical mortality rates of 50 % are expected within 3 months of diagnosis. However, adjuvant chemotherapy improves the prognosis of patients even after palliative surgery, and successful newer neoadjuvant chemotherapeutical modalities have recently been reported. For patients whose tumours appear unresectable, chemotherapy remains the only option. During the past two decades, the nucleoside analogue gemcitabine has become the first-line chemotherapy for pancreatic adenocarcinoma. In this study, we aim to increase the delivery of gemcitabine to pancreatic tumours by exploring the effect of sonoporation for localised drug delivery of gemcitabine in an orthotopic xenograft mouse model of pancreatic cancer.
Experimental Design
An orthotopic xenograft mouse model of luciferase expressing MIA PaCa-2 cells was developed, exhibiting disease development similar to human pancreatic adenocarcinoma. Subsequently, two groups of mice were treated with gemcitabine alone and gemcitabine combined with sonoporation; saline-treated mice were used as a control group. A custom-made focused ultrasound transducer using clinically safe acoustic conditions in combination with SonoVue® ultrasound contrast agent was used to induce sonoporation in the localised region of the primary tumour only. Whole-body disease development was measured using bioluminescence imaging, and primary tumour development was measured using 3D ultrasound.
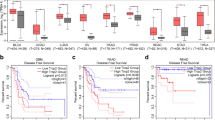
Results
Following just two treatments combining sonoporation and gemcitabine, primary tumour volumes were significantly lower than control groups. Additional therapy dramatically inhibited primary tumour growth throughout the course of the disease, with median survival increases of up to 10 % demonstrated in comparison to the control groups.
Conclusion
Combined sonoporation and gemcitabine therapy significantly impedes primary tumour development in an orthotopic xenograft model of human pancreatic cancer, suggesting additional clinical benefits for patients treated with gemcitabine in combination with sonoporation.






Similar content being viewed by others
References
American Cancer Society Cancer Facts and Figures (2013) http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-036845.pdf
Greenlee RT, Murray T, Bolden S, Wingo PA (2000) Cancer statistics, 2000. CA Cancer J Clin 50:7–33
Chen EL, Prinz RA (2007) Long-term survival after pancreatic cancer treatment. Am J Surg 194:S127–S130
Hartlapp I, Muller J, Kenn W et al (2013) Complete pathological remission of locally advanced, unresectable pancreatic cancer (LAPC) after intensified neoadjuvant chemotherapy. Onkologie 36:123–125
Neoptolemos JP, Stocken DD, Friess H et al (2004) A randomized trial of chemoradiotherapy and chemotherapy after resection of pancreatic cancer. N Engl J Med 350:1200–1210
Neoptolemos JP, Dunn JA, Stocken DD et al (2001) Adjuvant chemoradiotherapy and chemotherapy in resectable pancreatic cancer: a randomised controlled trial. Lancet 358:1576–1585
el-Kamar FG, Grossbard ML, Kozuch PS (2003) Metastatic pancreatic cancer: emerging strategies in chemotherapy and palliative care. Oncologist 8:18–34
Marechal R, Bachet JB, Mackey JR et al (2012) Levels of gemcitabine transport and metabolism proteins predict survival times of patients treated with gemcitabine for pancreatic adenocarcinoma. Gastroenterology 143(664–674):e661–666
Camp-Sorell D (2010) Chemotherapy toxicities and management. In: Yarbro CH, Wujcik D, Gobel BH (eds) Cancer nursing: principles and practice. Jones & Bartlett, Sudbury
Erchinger FG, Dimcevski G, Engjom T, Gilja OH (2011) Transabdominal ultrasonography of the pancreas: basic and new aspects. Imaging Med 3:412–422
Simpson DH, Burns PN, Averkiou MA (2001) Techniques for perfusion imaging with microbubble contrast agents. IEEE Trans Ultrason Ferroelectr Freq Control 48:1483–1494
Stride E, Saffari N (2003) Microbubble ultrasound contrast agents: a review. Proc Inst Mech Eng H J Eng Med 217:429–447
Postema MAB (2004) Medical bubbles. Michiel Postema, Bergschenhoek
Qiu Y, Zhang C, Tu J, Zhang D (2012) Microbubble-induced sonoporation involved in ultrasound-mediated DNA transfection in vitro at low acoustic pressures. J Biomech 45:1339–1345
Suzuki R, Oda Y, Utoguchi N, Maruyama K (2011) Progress in the development of ultrasound-mediated gene delivery systems utilizing nano- and microbubbles. J Control Release 149:36–41
Nejad SM, Hosseini SH, Akiyama H, Tachibana K (2011) Optical observations of cell sonoporation with low intensity ultrasound. Biochem Biophys Res Co 413:218–223
Kooiman K, Harteveld M, van der Steen AFW, de Jong N (2011) Sonoporation of endothelial cells by vibrating targeted microbubbles. J Control Release 154:35–41
Wu J, Pepe J, Rincon M (2006) Sonoporation, anti-cancer drug and antibody delivery using ultrasound. Ultrasonics 44:E21–E25
Delalande A, Kotopoulis S, Rovers T, Pichon C, Postema M (2011) Sonoporation at a low mechanical index. Bub Sci Eng Tech 3:3–11
van Wamel A, Bouakaz A, Bernard B, ten Cate F, de Jong N (2005) Controlled drug delivery with ultrasound and gas microbubbles. J Control Release 101:389–391
Emmer M, Borsboom J, Van Wamel A, Versluis M, de Jong N (2005) Optical investigation of ultrasound induced encapsulated microbubble oscillations: threshold and hysteresis effects. Proc IEEE Ultrason Symp:981–984
van Wamel A, Kooiman K, Harteveld M et al (2006) Vibrating microbubbles poking individual cells: drug transfer into cells via sonoporation. J Control Release 112:149–155
Postema M, Kotopoulis S, Delalande A, Gilja OH (2012) Sonoporation: why microbubbles create pores. Ultraschall in Med 33:97–98
Delalande A, Bouakaz A, Renault G et al (2011) Ultrasound and microbubble-assisted gene delivery in Achilles tendons: long lasting gene expression and restoration of fibromodulin KO phenotype. J Control Release 156:223–230
Delalande A, Kotopoulis S, Postema M, Midoux P, Pichon C (2013) Sonoporation: mechanistic insights and ongoing challenges for gene transfer. Gene 525:191–199
Gerold B, Rachmilevitch I, Prentice P (2013) Bifurcation of ensemble oscillations and acoustic emissions from early stage cavitation clouds in focused ultrasound. New J Phys 15:033044
Gerold B, Kotopoulis S, McDougall C, McGloin D, Postema M, Prentice P (2011) Laser-nucleated acoustic cavitation in focused ultrasound. Rev Sci Instrum 82:044908
Piscaglia F, Nolsoe C, Dietrich CF et al (2012) The EFSUMB guidelines and recommendations on the clinical practice of contrast enhanced ultrasound (CEUS): update 2011 on non-hepatic applications. Ultraschall Med 33:33–59
Ng KH (2002) International guidelines and regulations for the safe use of diagnostic ultrasound in medicine. J Med Ultrasound 10:5–9
British Medical Ultrasound Society (2000) Guidelines for the safe use of diagnostic ultrasound equipment. British Medical Ultrasound Society
Fan Z, Kumon RE, Park J, Deng CX (2010) Intracellular delivery and calcium transients generated in sonoporation facilitated by microbubbles. J Control Release 142:31–39
Tlaxca JL, Anderson CR, Klibanov AL et al (2010) Analysis of in vitro transfection by sonoporation using cationic and neutral microbubbles. Ultrasound Med Biol 36:1907–1918
Qiu Y, Luo Y, Zhang Y et al (2010) The correlation between acoustic cavitation and sonoporation involved in ultrasound-mediated DNA transfection with polyethylenimine (PEI) in vitro. J Control Release 145:40–48
Czarnota GJ, Karshafian R, Burns PN et al (2012) Tumor radiation response enhancement by acoustical stimulation of the vasculature. Proc Natl Acad Sci U S A 109:E2033–2041
Lukianova-Hleb EY, Samaniego AP, Wen J, Metelitsa LS, Chang CC, Lapotko DO (2011) Selective gene transfection of individual cells in vitro with plasmonic nanobubbles. J Control Release 152:286–293
Hoffman RM (1999) Orthotopic metastatic mouse models for anticancer drug discovery and evaluation: a bridge to the clinic. Invest New Drug 17:343–359
Bibby MC (2004) Orthotopic models of cancer for preclinical drug evaluation: advantages and disadvantages. Eur J Cancer 40:852–857
Greis C (2004) Technology overview: SonoVue (Bracco, Milan). Eur Radiol 14:P11–P15
Lu JY, Zou H, Greenleaf JF (1994) Biomedical ultrasound beam forming. Ultrasound Med Biol 20:403–428
Kotopoulis S, Dimcevski G, Gilja OH, Hoem D, Postema M (2013) Treatment of human pancreatic cancer using combined ultrasound, microbubbles, and gemcitabine: a clinical case study. Med Phys 40:072902–072909
Burris HA 3rd, Moore MJ, Andersen J et al (1997) Improvements in survival and clinical benefit with gemcitabine as first-line therapy for patients with advanced pancreas cancer: a randomized trial. J Clin Oncol 15:2403–2413
McCormack E, Mujic M, Osdal T, Bruserud O, Gjertsen BT (2013) Multiplexed mAbs: a new strategy in preclinical time-domain imaging of acute myeloid leukemia. Blood 121:e34–42
McCormack E, Silden E, West RM et al (2013) Nitroreductase, a near-infrared reporter platform for in vivo time-domain optical imaging of metastatic cancer. Cancer Res 73:1276–1286
Ozawa Y, Numata K, Tanaka K et al (2002) Contrast-enhanced sonography of small pancreatic mass lesions. J Ultrasound Med 21:983–991
Poortinga AT (2012) Micron-sized antibubbles with tunable stability. Colloids Surf A: Physiochem Eng Aspects
Zhang GN, Liang Y, Zhou LJ et al (2011) Combination of salinomycin and gemcitabine eliminates pancreatic cancer cells. Cancer Lett 313:137–144
Michaelis M, Doerr HW, Cinatl J (2007) Valproic acid as anti-cancer drug. Curr Pharm Design 13:3378–3393
Kunnumakkara AB, Guha S, Krishnan S, Diagaradjane P, Gelovani J, Aggarwal BB (2007) Curcumin potentiates antitumor activity of gemcitabine in an orthotopic model of pancreatic cancer through suppression of proliferation, angiogenesis, and inhibition of nuclear factor-kappaB-regulated gene products. Cancer Res 67:3853–3861
Acknowledgments
This work was supported by the Norwegian Cancer Society (grant numbers 421828 and 732200), the Western Health Board of Norway (grant numbers 911182 and 911789) and the Bergen Research Foundation. The study was supported by MedViz (http://medviz.uib.no/), an interdisciplinary research cluster from Haukeland University Hospital, University of Bergen and Christian Michelsen Research AS. We would like to thank Lars Helgeland (Section for Pathology, The Gade Institute, University of Bergen) for his advice on histology.
Conflict of Interest
The authors have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Anthony Delalande and Mihaela Popa contributed equally.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 183 kb)
Rights and permissions
About this article
Cite this article
Kotopoulis, S., Delalande, A., Popa, M. et al. Sonoporation-Enhanced Chemotherapy Significantly Reduces Primary Tumour Burden in an Orthotopic Pancreatic Cancer Xenograft. Mol Imaging Biol 16, 53–62 (2014). https://doi.org/10.1007/s11307-013-0672-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11307-013-0672-5