Abstract
Introduction
Prostate cancer is a multifactorial disease whose aetiology is still not fully understood. Metabolomics, by measuring several hundred metabolites simultaneously, could enhance knowledge on the metabolic changes involved and the potential impact of external factors.
Objectives
The aim of the present study was to investigate whether pre-diagnostic plasma metabolomic profiles were associated with the risk of developing a prostate cancer within the following decade.
Methods
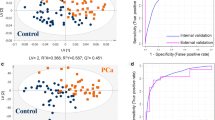
A prospective nested case-control study was set up among the 5141 men participant of the SU.VI.MAX cohort, including 171 prostate cancer cases, diagnosed between 1994 and 2007, and 171 matched controls. Nuclear magnetic resonance (NMR) metabolomic profiles were established from baseline plasma samples using NOESY1D and CPMG sequences. Multivariable conditional logistic regression models were computed for each individual NMR signal and for metabolomic patterns derived using principal component analysis.
Results
Men with higher fasting plasma levels of valine (odds ratio (OR) = 1.37 [1.07–1.76], p = .01), glutamine (OR = 1.30 [1.00–1.70], p = .047), creatine (OR = 1.37 [1.04–1.80], p = .02), albumin lysyl (OR = 1.48 [1.12–1.95], p = .006 and OR = 1.51 [1.13–2.02], p = .005), tyrosine (OR = 1.40 [1.06–1.85], p = .02), phenylalanine (OR = 1.39 [1.08–1.79], p = .01), histidine (OR = 1.46 [1.12–1.88], p = .004), 3-methylhistidine (OR = 1.37 [1.05–1.80], p = .02) and lower plasma level of urea (OR = .70 [.54–.92], p = .009) had a higher risk of developing a prostate cancer during the 13 years of follow-up.
Conclusions
This exploratory study highlighted associations between baseline plasma metabolomic profiles and long-term risk of developing prostate cancer. If replicated in independent cohort studies, such signatures may improve the identification of men at risk for prostate cancer well before diagnosis and the understanding of this disease.

Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- SU.VI.MAX:
-
Supplémentation en Vitamines et Minéraux Antioxydants
- BMI:
-
Body mass index
- NMR:
-
Nuclear magnetic resonance
- OR:
-
Odds ratio
- SD:
-
Standard deviation
- CI:
-
Confidence interval
- FDR:
-
False discovery rate
- PSA:
-
Prostate-specific antigen
- PCA:
-
Principal component analysis
- HDL:
-
High density lipoproteins
- LDL:
-
Low density lipoproteins
- BCAA:
-
Branched chain amino acids
- AAA:
-
Aromatic amino acids
References
Assi, N. (2015). A statistical framework to model the meeting-in-the-middle principle using metabolomic data: application to hepatocellular carcinoma in the EPIC study. Mutagenesis, 30(6), 743–753. https://doi.org/10.1093/mutage/gev045.
Assi, N., Thomas, D. C., Leitzman, M., Stepien, M., Chajes, V., Philip, T., et al. (2018). Are metabolic signatures mediating the relationship between lifestyle factors and hepatocellular carcinoma risk? Results from a nested case-control study in EPIC. Cancer Epidemiology, Biomarkers & Prevention, 27(5), 531–540. https://doi.org/10.1158/1055-9965.EPI-17-0649.
Athersuch, T. J., & Keun, H. C. (2015). Metabolic profiling in human exposome studies. Mutagenesis, 30(6), 755–762. https://doi.org/10.1093/mutage/gev060.
Benjamini, Y., & Hochberg, Y. (1995). Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society: Series B, 57(1), 289–300.
Bray, F., Ferlay, J., Soerjomataram, I., Siegel, R. L., Torre, L. A., & Jemal, A. (2018). Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians. https://doi.org/10.3322/caac.21492.
Bro, R., Kamstrup-Nielsen, M. H., Engelsen, S. B., Savorani, F., Rasmussen, M. A., Hansen, L., et al. (2015). Forecasting individual breast cancer risk using plasma metabolomics and biocontours. Metabolomics, 11(5), 1376–1380.
Brockmoller, S. F., Bucher, E., Muller, B. M., Budczies, J., Hilvo, M., Griffin, J. L., et al. (2012). Integration of metabolomics and expression of glycerol-3-phosphate acyltransferase (GPAM) in breast cancer-link to patient survival, hormone receptor status, and metabolic profiling. Journal of Proteome Research, 11, 850–860.
Budczies, J., Brockmoller, S. F., Muller, B. M., Barupal, D. K., Richter-Ehrenstein, C., Kleine-Tebbe, A., et al. (2013). Comparative metabolomics of estrogen receptor positive and estrogen receptor negative breast cancer: Alterations in glutamine and beta-alanine metabolism. Journal of Proteomics, 94C, 279–288.
Carayol, M., Licaj, I., Achaintre, D., Sacerdote, C., Vineis, P., Key, T. J., et al. (2015). Reliability of serum metabolites over a two-year period: A targeted metabolomic approach in fasting and non-fasting samples from EPIC. PLoS ONE, 10, e0135437.
Carr, H. Y., & Purcell, E. M. (1954). Effects of diffusion on free precession in nuclear magnetic resonance experiments. Physical Review, 94, 630–638.
Cattell, R. B. (1966). The scree test for the number of factors. Multivariate Behavioral Research, 1, 245–276.
Claudino, W. M., Quattrone, A., Biganzoli, L., Pestrin, M., Bertini, I., & Di, L. A. (2007). Metabolomics: Available results, current research projects in breast cancer, and future applications. Journal of Clinical Oncology, 25, 2840–2846.
Costello, L. C., & Franklin, R. B. (2000). The intermediary metabolism of the prostate: A key to understanding the pathogenesis and progression of prostate malignancy. Oncology (Williston Park, N.Y.), 59(4), 269–282. https://doi.org/10.1159/000012183.
Defossez, G., Le Guyader–Peyrou, S., Uhry, Z., Grosclaude, P., Colonna, M., & Dantony, E. (2019). Estimations nationales de l’incidence et de la mortalité par cancer en France métropolitaine entre 1990 et 2018. In Synthèse (p. 20). Santé publique France.
Delaglio, F., Grzesiek, S., Vuister, G. W., Zhu, G., Pfeifer, J., & Bax, A. (1995). NMRPipe: A multidimensional spectral processing system based on UNIX pipes. Journal of Biomolecular NMR, 6, 277–293.
Eidelman, E., Twum-Ampofo, J., Ansari, J., & Siddiqui, M. M. (2017). The metabolic phenotype of prostate cancer. Frontiers in Oncology, 7, 131. https://doi.org/10.3389/fonc.2017.00131.
Fages, A., Duarte-Salles, T., Stepien, M., Ferrari, P., Fedirko, V., Pontoizeau, C., et al. (2015). Metabolomic profiles of hepatocellular carcinoma in a European prospective cohort. BMC Medicine, 13, 242. https://doi.org/10.1186/s12916-015-0462-9.
Floegel, A., Drogan, D., Wang-Sattler, R., Prehn, C., Illig, T., Adamski, J., et al. (2011). Reliability of serum metabolite concentrations over a 4-month period using a targeted metabolomic approach. PLoS ONE, 6, e21103.
Giraudeau, P., Silvestre, V., & Akoka, S. (2015). Optimizing water suppression for quantitative NMR-based metabolomics: a tutorial review. Metabolomics, 11(5), 1041–1055.
Guenin, S., Schwartz, L., Morvan, D., Steyaert, J. M., Poignet, A., Madelmont, J. C., & Demidem, A. (2008). PP2A activity is controlled by methylation and regulates oncoprotein expression in melanoma cells: A mechanism which participates in growth inhibition induced by chloroethylnitrosourea treatment. International Journal of Oncology, 32, 49–57.
Hercberg, S., Galan, P., Preziosi, P., Bertrais, S., Mennen, L., Malvy, D., et al. (2004). The SU.VI.MAX study: A randomized, placebo-controlled trial of the health effects of antioxidant vitamins and minerals. Archives of Internal Medicine, 164, 2335–2342.
Hercberg, S., Preziosi, P., Briancon, S., Galan, P., Triol, I., Malvy, D., et al. (1998). A primary prevention trial using nutritional doses of antioxidant vitamins and minerals in cardiovascular diseases and cancers in a general population: the SU.VI.MAX study–design, methods, and participant characteristics. SUpplementation en VItamines et Mineraux AntioXydants. Controlled Clinical Trials, 19, 336–351.
Howell, A. (2010). Can metabolomics in addition to genomics add to prognostic and predictive information in breast cancer? BMC Medicine, 8, 73.
Huang, J., Mondul, A. M., Weinstein, S. J., Koutros, S., Derkach, A., Karoly, E., et al. (2016). Serum metabolomic profiling of prostate cancer risk in the prostate, lung, colorectal, and ovarian cancer screening trial. British Journal of Cancer, 115, 1087–1095.
Jobard, E., Pontoizeau, C., Blaise, B. J., Bachelot, T., Elena-Herrmann, B., & Tredan, O. (2014). A serum nuclear magnetic resonance-based metabolomic signature of advanced metastatic human breast cancer. Cancer Letters, 343, 33–41.
Koutros, S., Meyer, T. E., Fox, S. D., Issaq, H. J., Veenstra, T. D., Huang, W.-Y., et al. (2013). Prospective evaluation of serum sarcosine and risk of prostate cancer in the Prostate, Lung, Colorectal and Ovarian Cancer Screening Trial. Carcinogenesis, 34(10), 2281–2285. https://doi.org/10.1093/carcin/bgt176.
Kuhn, T., Floegel, A., Sookthai, D., Johnson, T., Rolle-Kampczyk, U., Otto, W., et al. (2016). Higher plasma levels of lysophosphatidylcholine 18:0 are related to a lower risk of common cancers in a prospective metabolomics study. BMC Medicine, 14, 13.
Kühn, T., Sookthai, D., Graf, M. E., Schübel, R., Freisling, H., Johnson, T., et al. (2017). Albumin, bilirubin, uric acid and cancer risk: Results from a prospective population-based study. British Journal of Cancer, 117(10), 1572–1579. https://doi.org/10.1038/bjc.2017.313.
Lécuyer, L., Dalle, C., Lyan, B., Demidem, A., Rossary, A., Vasson, M.-P., et al. (2019). Plasma metabolomic signatures associated with long-term breast cancer risk in the SU.VI.MAX prospective cohort. Cancer Epidemiology, Biomarkers & Prevention: A Publication of the American Association for Cancer Research, Cosponsored by the American Society of Preventive Oncology. https://doi.org/10.1158/1055-9965.EPI-19-0154.
Lécuyer, L., Bala, V., Deschasaux, A., Bouchemal, M., Triba, N. Nawfal, Vasson, M., M.-P., et al (2018). NMR metabolomic signatures reveal predictive plasma metabolites associated with long-term risk of developing breast cancer. International Journal of Epidemiology, 47(2), 484–494. https://doi.org/10.1093/ije/dyx271.
Leverve, X., Carpentier, F., Barnoud, D., Fontaine, E., & Guignier, M. (1992). Intérêt et limites de la 3-méthylhistidine pour la mesure du catabolisme musculaire. Nutrition Clinique et Métabolisme, 6(4), 219–225. https://doi.org/10.1016/S0985-0562(05)80371-1.
Liesenfeld, D. B., Habermann, N., Owen, R. W., Scalbert, A., & Ulrich, C. M. (2013). Review of mass spectrometry-based metabolomics in cancer research. Cancer Epidemiology, Biomarkers & Prevention, 22, 2182–2201.
Lucarelli, G., Loizzo, D., Ferro, M., Rutigliano, M., Vartolomei, M. D., Cantiello, F., et al. (2019). Metabolomic profiling for the identification of novel diagnostic markers and therapeutic targets in prostate cancer: An update. Expert Review of Molecular Diagnostics, 19(5), 377–387. https://doi.org/10.1080/14737159.2019.1604223.
Lucarelli, G., Rutigliano, M., Galleggiante, V., Giglio, A., Palazzo, S., Ferro, M., et al. (2015). Metabolomic profiling for the identification of novel diagnostic markers in prostate cancer. Expert Review of Molecular Diagnostics, 15(9), 1211–1224. https://doi.org/10.1586/14737159.2015.1069711.
Magnusson, M., Lewis, G. D., Ericson, U., Orho-Melander, M., Hedblad, B., Engstrom, G., et al. (2013). A diabetes-predictive amino acid score and future cardiovascular disease. European Heart Journal, 34, 1982–1989.
Maxeiner, A., Adkins, C. B., Zhang, Y., Taupitz, M., Halpern, E. F., McDougal, W. S., et al. (2010). Retrospective analysis of prostate cancer recurrence potential with tissue metabolomic profiles. Prostate, 70, 710–717.
Merlot, A. M., Kalinowski, D. S., & Richardson, D. R. (2014). Unraveling the mysteries of serum albumin-more than just a serum protein. Frontiers in Physiology, 5, 299. https://doi.org/10.3389/fphys.2014.00299.
Mondul, A. M., Moore, S. C., Weinstein, S. J., Karoly, E. D., Sampson, J. N., & Albanes, D. (2015). Metabolomic analysis of prostate cancer risk in a prospective cohort: The alpha-tocolpherol, beta-carotene cancer prevention (ATBC) study. International Journal of Cancer, 137, 2124–2132.
Mondul, A. M., Moore, S. C., Weinstein, S. J., Mannisto, S., Sampson, J. N., & Albanes, D. (2014). 1-stearoylglycerol is associated with risk of prostate cancer: Results from serum metabolomic profiling. Metabolomics, 10, 1036–1041.
Newgard, C. B., An, J., Bain, J. R., Muehlbauer, M. J., Stevens, R. D., Lien, L. F., et al. (2009). A branched-chain amino acid-related metabolic signature that differentiates obese and lean humans and contributes to insulin resistance. Cell Metabolism, 9, 311–326.
O’Connell, T. M. (2013). The complex role of branched chain amino acids in diabetes and cancer. Metabolites, 3, 931–945.
Ren, J.-G., Seth, P., Ye, H., Guo, K., Hanai, J.-I., Husain, Z., & Sukhatme, V. P. (2017). Citrate Suppresses tumor growth in multiple models through inhibition of glycolysis, the tricarboxylic acid cycle and the IGF-1R pathway. Scientific Reports, 7(1), 4537. https://doi.org/10.1038/s41598-017-04626-4.
Scalbert, A., Brennan, L., Manach, C., Andres-Lacueva, C., Dragsted, L. O., Draper, J., et al. (2014). The food metabolome: A window over dietary exposure. The American Journal of Clinical Nutrition, 99(6), 1286–1308.
Schmidt, J. A., Fensom, G. K., Rinaldi, S., Scalbert, A., Appleby, P. N., Achaintre, D., et al. (2017). Pre-diagnostic metabolite concentrations and prostate cancer risk in 1077 cases and 1077 matched controls in the European Prospective Investigation into Cancer and Nutrition. BMC Medicine, 15(1), 122. https://doi.org/10.1186/s12916-017-0885-6.
Sousa, S. A., Magalhaes, A., & Ferreira, M. M. (2013). Optimized bucketing for NMR spectra: Three case studies. Chemometrics and Intelligent Laboratory Systems, 122, 93–102.
Sreekumar, A., Poisson, L. M., Rajendiran, T. M., Khan, A. P., Cao, Q., Yu, J., et al. (2009). Metabolomic profiles delineate potential role for sarcosine in prostate cancer progression. Nature, 457, 910–914.
Stepien, M., Duarte-Salles, T., Fedirko, V., Floegel, A., Barupal, D. K., Rinaldi, S., et al. (2016). Alteration of amino acid and biogenic amine metabolism in hepatobiliary cancers: Findings from a prospective cohort study. International Journal of Cancer, 138, 348–360.
Vandenbroucke, J. P., & Pearce, N. (2012). Case-control studies: Basic concepts. International Journal of Epidemiology, 41(5), 1480–1489. https://doi.org/10.1093/ije/dys147.
WHO. (1993). ICD-10, International Classification of Diseases and related health problems, 10th revision. World Health Organization.
Wishart, D. S., Feunang, Y. D., Marcu, A., Guo, A. C., Liang, K., Vázquez-Fresno, R., et al. (2018). HMDB 4.0: The human metabolome database for 2018. Nucleic Acids Research, 46(D1), D608–D617. https://doi.org/10.1093/nar/gkx1089.
Wood, S. L., Westbrook, J. A., & Brown, J. E. (2014). Omic-profiling in breast cancer metastasis to bone: Implications for mechanisms, biomarkers and treatment. Cancer Treatment Reviews, 40, 139–152.
World Cancer Research Fund/American Institute for Cancer Research. (2014). Continuous Update Project Expert Report 2018. Diet, nutrition, physical activity and prostate cancer. World Cancer Research Fund/American Institute for Cancer Research.
World Cancer Research Fund/American Institute for Cancer Research. (2018). Continuous Update Project Expert Report 2018. The cancer process. http://www.dietandcancerreport.org.
Wu, S., Zhu, W., Thompson, P., & Hannun, Y. A. (2018). Evaluating intrinsic and non-intrinsic cancer risk factors. Nature Communications, 9(1), 3490. https://doi.org/10.1038/s41467-018-05467-z.
Wurtz, P., Soininen, P., Kangas, A. J., Ronnemaa, T., Lehtimaki, T., Kahonen, M., et al. (2013). Branched-chain and aromatic amino acids are predictors of insulin resistance in young adults. Diabetes Care, 36(3), 648–655. https://doi.org/10.2337/dc12-0895.
Acknowledgements
The authors thank all participants of the SU.VI.MAX study as well as Younes Esseddik, Thi Hong Van Duong, Régis Gatibelza, and Jagatjit Mohinder (computer scientists), Cédric Agaesse (dietitian), Fabien Szabo de Edelenyi, PhD, Julien Allègre, Nathalie Arnault, Laurent Bourhis (data-managers/biostatisticians), and Fatoumata Diallo, MD, Roland Andrianasolo, MD and Sandrine Kamdem (physicians), for their technical contribution. This work was conducted in the framework of the French network for Nutrition And Cancer Research (NACRe network), and received the NACRe Partnership Label.
Funding
This work was supported by the Fondation de France [Grant Number 2015 00060743 for the project], by the French National Cancer Institute [PhD Grant Number INCa_11323 for L. Lecuyer]; and the Federative Institute for Biomedical Research IFRB Paris 13. The funders had no role in the design, analysis, or writing of this article.
Author information
Authors and Affiliations
Contributions
The author’s responsibilities were as follow—LL and MT: designed the research; SH, PG, MT, EKG: conducted the research; NB, AVB: acquired NMR spectra; LL: performed statistical analysis; MT, MNT: supervised statistical analysis; LL and MT: wrote the paper; LL, AVB, AD, AR, NB, MNT, PG, SH, VP, LLM, BS, PLM, EKG, NDP, MD, PS, MT: contributed to the data interpretation and revised each draft for important intellectual content; and MT had primary responsibility for final content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to disclose.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent for publication
All authors have approved the manuscript before submission. Participants signed informed consent regarding publishing their data.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lécuyer, L., Victor Bala, A., Demidem, A. et al. NMR metabolomic profiles associated with long-term risk of prostate cancer. Metabolomics 17, 32 (2021). https://doi.org/10.1007/s11306-021-01780-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11306-021-01780-9