Abstract
Objectives
To evaluate the relationship between internal derangement and morphological features of the temporomandibular joint by comparing joint morphology between patients with ID and control patients.
Methods
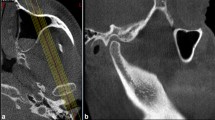
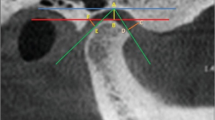
The current study prospectively is evaluated the cone-beam computed images of 106 ID patients and 122 patients with asymptomatic joints; recorded angular and linear measurements. The relationships between these measurements and ID are investigated; the differences between the two groups using paired t tests.
Results
There were significant differences in the values of articular slope and the condyle height/glenoid fossa depth (CH/GFD) ratio between patients in the ID and control groups (p < 0.05). There was also a relationship between these parameters and the gender of patients with ID. The condylar position was posterior in the ID group.
Conclusion
Posteriorly and superiorly located condyles with an increased CH/GFD ratio, condyles located eccentrically, and a steeper posterior slope may be risk factors for ID.


Similar content being viewed by others
Change history
04 May 2023
A Correction to this paper has been published: https://doi.org/10.1007/s11282-023-00684-9
References
Schiffman E, et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the international RDC/TMD consortium network and orofacial pain special interest group. J Oral Facial Pain Headache. 2014;28(1):6.
Salo L, et al. Internal derangement of the temporomandibular joint: a histochemical study. J Oral Maxillofac Surg. 1991;49(2):171–6.
Tuz H, et al. Comparison of local and general anaesthesia for arthrocentesis of the temporomandibular joint. Br J Oral Maxillofac Surg. 2016;54(8):946–9.
de Senna BR, et al. Condyle-disk-fossa position and relationship to clinical signs and symptoms of temporomandibular disorders in women. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 2009;108(3):e117–24.
Arnett G, Milam S, Gottesman L. Morphologic changes of the temporomandibular joint associated with orthognathic surgery. Philadelphia: WB Saunders; 2000.
Pullinger AG, et al. Multifactorial comparison of disk displacement with and without reduction to normals according to temporomandibular joint hard tissue anatomic relationships. J Prosthet Dent. 2002;87(3):298–310.
Imanimoghaddam M, et al. Evaluation of condylar positions in patients with temporomandibular disorders: a cone-beam computed tomographic study. Imaging Sci Dent. 2016;46(2):127–31.
Bonilla-Aragon H, et al. Condyle position as a predictor of temporomandibular joint internal derangement. J Prosthet Dent. 1999;82(2):205–8.
Sato S, et al. Morphology of the mandibular fossa and the articular eminence in temporomandibular joints with anterior disk displacement. Int J Oral Maxillofac Surg. 1996;25(3):236–8.
Fraga MR, et al. Anteroposterior condylar position: a comparative study between subjects with normal occlusion and patients with Class I, Class II Division 1, and Class III malocclusions. Med Sci Monit Int Med J Exp Clin Res. 2013;19:903.
Kikuchi K, et al. Association between condylar position, joint morphology and craniofacial morphology in orthodontic patients without temporomandibular joint disorders. J Oral Rehabil. 2003;30(11):1070–5.
Crusoé-Rebello IMR, et al. Evaluation of the relation between the horizontal condylar angle and the internal derangement of the TMJ-a magnetic resonance imaging study. Pesqui Odontol Bras. 2003;17:176–82.
Jasinevicius T, et al. Relationship of degenerative changes of the temporomandibular joint (TMJ) with the angle of eminentia. J Oral Rehabil. 2006;33(9):638–45.
Pullinger AG, et al. A tomographic study of mandibular condyle position in an asymptomatic population. J Prosthet Dent. 1985;53(5):706–13.
Sümbüllü M, et al. Radiological examination of the articular eminence morphology using cone beam CT. Dentomaxillofacial Radiol. 2012;41(3):234–40.
Yasa Y, Akgül HM. Comparative cone-beam computed tomography evaluation of the osseous morphology of the temporomandibular joint in temporomandibular dysfunction patients and asymptomatic individuals. Oral Radiol. 2018;34(1):31–9.
Park J, et al. Correlation between clinical diagnosis based on RDC/TMD and MRI findings of TMJ internal derangement. Int J Oral Maxillofac Surg. 2012;41(1):103–8.
Amorim MY, et al. Inclination of the condylar long axis is not related to temporomandibular disc displacement. J Investig Clin Dent. 2019;10(1): e12375.
Al-Rawi NH, Uthman AT, Sodeify SM. Spatial analysis of mandibular condyles in patients with temporomandibular disorders and normal controls using cone beam computed tomography. Eur J Dent. 2017;11(01):099–105.
Honda K, et al. Thickening of the glenoid fossa in osteoarthritis of the temporomandibular joint. Dentomaxillofacial Radiol. 2001;30(1):10–3.
İlgüy D, et al. Articular eminence inclination, height, and condyle morphology on cone beam computed tomography. Sci World J. 2014;2014:1.
Major PW, et al. Tomographic assessment of temporomandibular joint osseous articular surface contour and spatial relationships associated with disc displacement and disc length. Am J Orthod Dentofac Orthop. 2002;121(2):152–61.
Markovic MA, Rosenberg HM. Tomographic evaluation of 100 patients with temporomandibular joint symptoms. Oral Surg Oral Med Oral Pathol. 1976;42(6):838–46.
Paknahad M, et al. Cone-beam computed tomographic assessment of mandibular condylar position in patients with temporomandibular joint dysfunction and in healthy subjects. Int J Dent. 2015;2015:1.
Sülün T, et al. Morphology of the mandibular fossa and inclination of the articular eminence in patients with internal derangement and in symptom-free volunteers. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 2001;92(1):98–107.
Weinberg LA. An evaluation of occlusal factors in TMJ dysfunction-pain syndrome. J Prosthet Dent. 1979;41(2):198–208.
Fonseca RJ. Oral and maxillofacial surgery-E-book, vol. 3, 2nd ed. Elsevier Health Sciences; 2009. p. 789–1004.
Ren Y-F, Isberg A, Westesson P-L. Steepness of the articular eminence in the temporomandibular joint: tomographic comparison between asymptomatic volunteers with normal disk position and patients with disk displacement. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 1995;80(3):258–66.
Paknahad M, et al. Is mandibular fossa morphology and articular eminence inclination associated with temporomandibular dysfunction? J Dent. 2016;17(2):134.
Wadhwa S, Kapila S. TMJ disorders: future innovations in diagnostics and therapeutics. J Dent Educ. 2008;72(8):930–47.
Razi T, Razi S. Association between the morphology and thickness of bony components of the temporomandibular joint and gender, age and remaining teeth on cone-beam CT images. Dental Med Probl. 2018;55(3):299–304.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. Additional informed consent was obtained from all patients for which identifying information included in this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest related to this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised due to the table 2 was published incorrectly and the table has been corrected.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Meral, S.E., Karaaslan, S., Tüz, H.H. et al. Evaluation of the temporomandibular joint morphology and condylar position with cone-beam computerized tomography in patients with internal derangement. Oral Radiol 39, 173–179 (2023). https://doi.org/10.1007/s11282-022-00618-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11282-022-00618-x