Abstract
Objectives
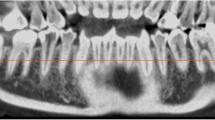
This study aims to reveal whether and which position of lower third molar (M3), assessed on a 2D image, indicates or potentially exclude the need for the CBCT exploration of the retromolar canal (RMC). We hypothesized that some positions of M3 are associated with overall higher incidence of the RMC, and particularly clinically relevant ones, thus justifying additional CBCT diagnostics.
Methods
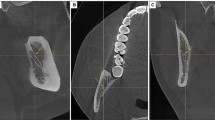
CBCT exam of 186 hemi-mandibles with present M3 were selected for the study. Explorations were made during the 2-year period from January 1th 2018 to December 31th 2019 with Scanora 3Dx Sorodex (Tussula, Finland). The following variables were assessed: the presence and width of the RMC, eruption status, and angulation of the M3. The RMC presence in relation to the M3 eruption status and angulation was analyzed using appropriate statistical tests.
Results
RMC was present in 89 (47.8%) out of 186 hemi-mandibles. Mean canal width was 1.51 mm. 22.5% of detected canals had the diameter exceeding 2 mm. Third molar’s eruption status showed no statistical correlation with the occurrence of RMC. We observed significantly higher occurrence of RMC in the hemi-mandibles containing distally angulated M3 in comparison to other orientations (p = 0.025).
Conclusion
Based upon our findings, we recommend preoperative CBCT in cases where distal angulation of M3 is observed on 2D images, for the purpose of RMC exploration. Lower resolution CBCT mode and limited field of view (XS or S) are sufficient for the visualization of potentially clinically relevant RMCs, with as much reducing the patient dose.


Similar content being viewed by others
References
Schejtman R, Devoto FC, Arias NH. The origin and distribution of the elements of the human mandibular retromolar canal. Arch Oral Biol. 1967;12:1261–7.
Bilecenoglu B, Tuncer N. Clinical and anatomical study of retromolar foramen and canal. J Oral Maxillofac Surg. 2006;64:1493–7.
Alves N, Deana NF. Anatomical and radiographical study of the retromolar canal and retromolar foramen in macerated mandibles. Int J Clin Exp Med. 2015;15:4292–6.
Moreno Rabie C, Vranckx M, Rusque MI, Deambrosi C, Ockerman A, Politis C, Jacobs R. Anatomical relation of third molars and the retromolar canal. Br J Oral Maxillofac Surg. 2019;57:765–70.
Gamieldien MY, Van Schoor A. Retromolar foramen: an anatomical study with clinical considerations. Br J Oral Maxillofac Surg. 2016;54:784–7.
Kikuta S, Iwanaga J, Nakamura K, Hino K, Nakamura M, Kusukawa J. The retromolar canals and foramina: radiographic observation and application to oral surgery. Surg Radiol Anat. 2018;40:647–52.
Hou Y, Feng G, Lin W, Wang R, Yuan H. Observation of retromolar canals on cone beam computed tomography. Oral Radiol. 2020;36:365–70.
Patil S, Matsuda Y, Nakajima K, Araki K, Okano T. Retromolar canals as observed on cone-beam computed tomography: their incidence, course, and characteristics. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115:692–9.
Truong MK, He P, Adeeb N, Oskouian RJ, Tubbs RS, Iwanaga J. Clinical anatomy and significance of the retromolar foramina and their canals: a literature review. Cureus. 2017;9: e1781.
Capote TS, Gonçalves MA, Campos JA. Retromolar canal associated with age, side, sex, bifid mandibular canal, and accessory mental foramen in panoramic radiographs of Brazilians. Anat Res Int. 2015;2015:434083.
Sisman Y, Sekerci AE, Payveren-Arikan M, Sahman H. Diagnostic accuracy of cone-beam CT compared with panoramic images in predicting retromolar canal during extraction of impacted mandibular third molars. Med Oral Patol Oral Cir Bucal. 2015;20:74–81.
De Oliveira-Santos C, Souza PH, de Azambuja B-C, Stinkens L, Moyaert K, Rubira-Bullen IR, Jacobs R. Assessment of variations of the mandibular canal through cone beam computed tomography. Clin Oral Investig. 2012;16:387–93.
Iida S, Hassfeld S, Reuther T, Nomura K, Mühling J. Relationship between the risk of mandibular angle fractures and the status of incompletely erupted mandibular third molars. J Craniomaxillofac Surg. 2005;33:158–63.
Antic S, Milicic B, Jelovac DB, Djuric M. Impact of the lower third molar and injury mechanism on the risk of mandibular angle and condylar fracture. Dent Traumatol. 2016;32:286–95.
Winter G. Principles of Exodontia as applied to the impacted third molars. St. Louis: American Medical Book Company; 1926.
Ludlow JB, Davies-Ludlow LE, White SC. Patient risk related to common dental radiographic examinations: the impact of 2007 International Commission on Radiological Protection recommendations regarding dose calculation. J Am Dent Assoc. 2008;139:1237–43.
Shin HS, Nam KC, Park H, Choi HU, Kim HY, Park CS. Effective doses from panoramic radiography and CBCT (cone beam CT) using dose area product (DAP) in dentistry. Dentomaxillofac Radiol. 2014;43:20130439.
Qiang W, Qiang F, Lin L. Estimation of effective dose of dental x-ray devices. Radiat Prot Dosimetry. 2019;183:417–21.
Ludlow JB, Timothy R, Walker C, Hunter R, Benavides E, Samuelson DB, Scheske MJ. Effective dose of dental CBCT-a meta analysis of published data and additional data for nine CBCT units. Dentomaxillofac Radiol. 2015;44:20140197.
Oenning AC, Jacobs R, Pauwels R, Stratis A, Hedesiu M, Salmon B, DIMITRA Research Group. Cone-beam CT in paediatric dentistry: DIMITRA project position statement. Pediatr Radiol. 2018;48:308–16.
Luangchana P, Pornprasertsuk-Damrongsri S, Kitisubkanchana J, Wongchuensoontorn C. The retromolar canal and its variations: Classification using cone beam computed tomography. Quintessence Int. 2018;49:61–7.
Nikkerdar N, Golshah A, Norouzi M, Falah-Kooshki S. Incidence and anatomical properties of retromolar canal in an Iranian population: a cone-beam computed tomography study. Int J Dent. 2020;9:9178973.
von Arx T, Hänni A, Sendi P, Buser D, Bornstein MM. Radiographic study of the mandibular retromolar canal: an anatomic structure with clinical importance. J Endod. 2011;37:1630–5.
Narayana K, Nayak UA, Ahmed WN, Bhat JG, Devaiah BA. The retromolar foramen and canal in south Indian dry mandibles. Eur J Anat. 2002;6:141–6.
Schneider T, Filo K, Kruse AL, Locher M, Grätz KW, Lübbers HT. Variations in the anatomical positioning of impacted mandibular wisdom teeth and their practical implications. Swiss Dent J. 2014;124:520–38.
Quek SL, Tay CK, Tay KH, Toh SL, Lim KC. Pattern of third molar impaction in a Singapore Chinese population: a retrospective radiographic survey. Int J Oral Maxillofac Surg. 2003;32:548–52.
Matzenn LH, Wenzel A. Efficacy of CBCT for assessment of impacted mandibular third molars: a review – based on a hierarchical model of evidence. Dentomaxillofac Radiol. 2015;44:20140189.
Kim TS, Caruso JM, Christensen H, Torabinejad M. A comparison of Cone-Beam Computed Tomography and direct measurement in the examination of the mandibular canal and adjacent structures. J Endodont. 2010;36:1191–4.
Maret D, Telmon N, Peters OA, Lepage B, Treil J, Inglese JM, Peyre A, Kahn JL, Sixou M. Effect of voxel size on the accuracy of 3D reconstructions with cone beam CT. Dentomaxillofac Radiol. 2012;41:649–55.
Palma LF, Buck AF, Kfouri FA, Blachman IT, Lombardi LA, Cavalli MA. Evaluation of retromolar canals on cone beam computerized tomography scans and digital panoramic radiographs. Oral Maxillofac Surg. 2017;21:307–12.
Ngeow WC, Chai WL. The clinical significance of the retromolar canal and foramen in dentistry. Clin Anat. 2021;34:512–21.
Funding
There is no funding sources.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Not required according to national ethical guidelines. This article does not contain any studies with human or animal subjects performed by any of the authors.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Antic, S., Markovic-Vasiljkovic, B., Radivojević, O. et al. Can lower third molar position indicate the need for preoperative cone beam computed tomography exploration of retromolar canal?. Oral Radiol 38, 618–624 (2022). https://doi.org/10.1007/s11282-022-00597-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11282-022-00597-z