Abstract
Objective
To clarify CT diagnostic performance in extranodal extension of cervical lymph node metastases using deep learning classification.
Methods
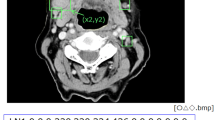
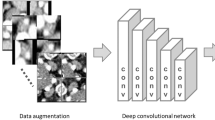
Seven-hundred and three CT images (178 with and 525 without extranodal extension) in 51 patients with cervical lymph node metastases from oral squamous cell carcinoma were enrolled in this study. CT images were cropped to an arbitrary size to include lymph nodes and surrounding tissues. All images were automatically divided into two datasets, assigning 80% as the training dataset and 20% as the testing dataset. The automated selection was repeated five times. Each training dataset was imported to a deep learning training system “DIGITS”. Five learning models were created after 300 epochs of the learning process using a neural network “AlexNet”. Each testing dataset was applied to each created learning model and resulting five performances were averaged as estimated diagnostic performances. A radiologist measured the minor axis and three radiologists evaluated central necrosis and irregular borders of each lymph node, and the diagnostic performances were obtained.
Results
The deep learning accuracy of extranodal extension was 84.0%. The radiologists’ accuracies based on minor axis ≥ 11 mm, central necrosis, and irregular borders were 55.7%, 51.1% and 62.6%, respectively.
Conclusions
The deep learning diagnostic performance in extranodal extension was significantly higher than that of radiologists. This method is expected to improve diagnostic accuracy by further study with increasing the number of patients.





Similar content being viewed by others
References
Kann BH, Aneja S, Loganadane GV, Kelly JR, Smith SM, Decker RH, et al. Pretreatment identification of head and neck cancer nodal metastasis and extranodal extension using deep learning neural networks. Sci Rep. 2018;8:14036.
O'Sullivan B. Head and neck tumours. In: Brierley J, Gospodarowicz MK, Wittekind C, editors. UICC TNM classification of malignant tumours. 8th ed. Chichester: Wiley; 2017. p. 17–54.
Amin M, Edge S, Greene F, Schilsky RL, Gaspar LE, Washington MK, et al. AJCC cancer staging manual. 8th ed. New York: Springer; 2017. p. P55–65.
Aiken AH, Poliashenko S, Beitler JJ, Chen AY, Baugnon KL, Corey AS, et al. Accuracy of preoperative imaging in detecting nodal extracapsular spread in oral cavity squamous cell carcinoma. AJNR Am J Neuroradiol. 2015;36:1776–811.
Zoumalan RA, Kleinberger AJ, Morris LG, Ranade A, Yee H, DeLacure MD, et al. Lymph node central necrosis on computed tomography as predictor of extracapsular spread in metastatic head and neck squamous cell carcinoma: pilot study. J Laryngol Otol. 2010;124:1284–8.
Maxwell JH, Rath TJ, Byrd JK, Albergotti WG, Wang H, Duvvuri U, et al. Accuracy of computed tomography to predict extracapsular spread in p16-positive squamous cell carcinoma. Laryngoscope. 2015;125:1613–8.
Chai RL, Rath TJ, Johnson JT, Ferris RL, Kubicek GJ, Duvvuri U, et al. Accuracy of computed tomography in the prediction of extracapsular spread of lymph node metastases in squamous cell carcinoma of the head and neck. JAMA Otolaryngol Head Neck Surg. 2013;139:1187–94.
Aerts HJ, Velazquez ER, Leijenaar RT, Parmar C, Grossmann P, Carvalho S, et al. Decoding tumour phenotype by noninvasive imaging using a quantitative radiomics approach. Nat Commun. 2014;5:4006.
Wong AJ, Kanwar A, Mohamed AS, Fuller CD. Radiomics in head and neck cancer: from exploration to application. Transl Cancer Res. 2016;5:371–82.
LeCun Y, Bengio Y, Hinton G. Deep learning. Nature. 2015;521:436–44.
Cireşan D, Meier U, Masci J, Schmidhuber J. Multi-column deep neural network for traffic sign classification. Neural Netw. 2012;32:333–8.
Chang K, Bai HX, Zhou H, Su C, Bi WL, Agbodza E, et al. Residual convolutional neural network for the determination of IDH status in low- and high-grade gliomas from MR imaging. Clin Cancer Res. 2018;24:1073–81.
Simonyan K, Zisserman A. Verd deep convolutional networks for large-scale image recognition. 2014. https://arxiv.org/abs/1409.1556
Silver D, Schrittwieser J, Simonyan K, Antonoglou I, Huang A, Guez A, et al. Mastering the game of Go without human knowledge. Nature. 2017;550:354–9.
Silver D, Huang A, Maddison CJ, Guez A, Sifre L, van den Driessche G, et al. Mastering the game of Go with deep neural networks and tree search. Nature. 2016;529:484–9.
Ariji Y, Fukuda M, Kise Y, Nozawa M, Yanashita Y, Fujita H, et al. Contrast-enhanced computed tomography image assessment of cervical lymph node metastasis in patients with oral cancer by using a deep learning system of artificial intelligence. Oral Surg Oral Med Oral Pathol Oral Radiol. 2019 (in press). https://doi.org/10.1016/j.oooo.2018.10.002.
Jose J, Coatesworth AP, Johnston C, MacLennan K. Cervical node metastases in squamous cell carcinoma of the upper aerodigestive tract: the significance of extracapsular spread and soft tissue deposits. Head Neck. 2003;25:451–6.
Brasilino de Carvalho M. Quantitative analysis of the extent of extracapsular invasion and its prognostic significance: a prospective study of 170 cases of carcinoma of the larynx and hypopharynx. Head Neck. 1998;20:16-21.
Bernier J, Cooper JS, Pajak TF, van Glabbeke M, Bourhis J, Forastiere A, et al. Defining risk levels in locally advanced head and neck cancers: a comparative analysis of concurrent postoperative radiation plus chemotherapy trials of the EORTC (#22931) and RTOG (# 9501). Head Neck. 2005;27:843–50.
Carlton JA, Maxwell AW, Bauer LB, McElroy SM, Layfield LJ, Ahsan H, et al. Computed tomography detection of extracapsular spread of squamous cell carcinoma of the head and neck in metastatic cervical lymph nodes. Neuroradiol J. 2017;30:222–9.
Prabhu RS, Magliocca KR, Hanasoge S, Aiken AH, Hudgins PA, Hall WA, et al. Accuracy of computed tomography for predicting pathologic nodal extracapsular extension in patients with head-and-neck cancer undergoing initial surgical resection. Int J Radiat Oncol Biol Phys. 2014;88:122–9.
Johnson JT, Barnes EL, Myers EN, Schramm VL Jr, Borochovitz D, Sigler BA. The extracapsular spread of tumors in cervical node metastasis. Arch Otolaryngol. 1981;107:725–9.
Don DM, Anzai Y, Lufkin RB, Fu YS, Calcaterra TC. Evaluation of cervical lymph node metastases in squamous cell carcinoma of the head and neck. Laryngoscope. 1995;105:669–74.
Yousem DM, Som PM, Hackney DB, Schwaibold F, Hendrix RA. Central nodal necrosis and extracapsular neoplastic spread in cervical lymph nodes: MR imaging versus CT. Radiology. 1992;182:753–9.
King AD, Tse GM, Yuen EH, To EW, Vlantis AC, Zee B, et al. Comparison of CT and MR imaging for the detection of extranodal neoplastic spread in metastatic neck nodes. Eur J Radiol. 2004;52:264–70.
Misselt PN, Glazebrook KN, Reynolds C, Degnim AC, Morton MJ. Predictive value of sonographic features of extranodal extension in axillary lymph nodes. J Ultrasound Med. 2010;29:1705–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Yoshiko Ariji, Yoshihiko Sugita, Toru Nagao, Atsushi Nakayama, Motoki Fukuda, Yoshitaka Kise, Michihito Nozawa, Masako Nishiyama, Akitoshi Katumata and Eiichiro Ariji declare that they have no conflict of interest.
Human rights statements and informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions.
Animal rights statement
This article does not contain any studies with animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ariji, Y., Sugita, Y., Nagao, T. et al. CT evaluation of extranodal extension of cervical lymph node metastases in patients with oral squamous cell carcinoma using deep learning classification. Oral Radiol 36, 148–155 (2020). https://doi.org/10.1007/s11282-019-00391-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11282-019-00391-4