Abstract
Purpose
Patients with lower urinary tract malformations (LUTM) were suspended from kidney transplantation (KT) programs in the past due to various concerns. Consequently, only a limited number of studies have explored this topic at hand. In this study, our objective was to perform a systematic review (SR) to evaluate the current evidence regarding KT outcomes as well as patient survival (PS), postoperative complications and urinary tract infections (UTI) in individuals with childhood LUTM.
Methods
The search encompassed databases of Web of Science, Medline (via PubMed), and Embase (via Scopus) to identify all studies reporting outcomes on KT for patients with LUTM. The research included articles published in English from January 1995 till September 2023.
Results
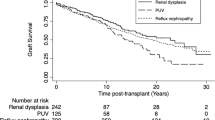
Of the 2634 yielded articles, 15 met the inclusion criteria, enrolling a total of 284,866 KT patients. There was significantly better 5-year graft survival (GS) in recipients with LUTM compared to the control group (RR, 1.04; 95% CI 1.02–1.06); while GS at 1-year and 10-year, and PS at 1-year, 5-year and 10-year were similar between groups. On the other hand, the postoperative UTI rate was significantly higher in the LUTM group (RR: 4.46; 95% CI 1.89–10.51). However, data on serum creatinine and estimated glomerular filtration rate on follow-up were insufficient.
Conclusion
GS and PS rates appear to be similar in patients with childhood LUTM and those with normal lower urinary tract functions. Despite a higher postoperative UTI rate within this patient group, it appears that this has no effect on GS rates.


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Stonebrook E, Hoff M, Spencer JD (2019) Congenital anomalies of the kidney and urinary tract: a clinical review. Curr Treat Options Pediatr 5(3):223–235. https://doi.org/10.1007/s40746-019-00166-3
Harada R, Hamasaki Y, Okuda Y, Hamada R, Ishikura K (2022) Epidemiology of pediatric chronic kidney disease/kidney failure: learning from registries and cohort studies. Pediatr Nephrol 37(6):1215–1229. https://doi.org/10.1007/s00467-021-05145-1
Czyzewski L, Sanko-Resmer J, Wyzgal J, Kurowski A (2014) Assessment of health-related quality of life of patients after kidney transplantation in comparison with hemodialysis and peritoneal dialysis. Ann Transplant 19:576–585
Guha C, van Zwieten A, Khalid R, Kim S, Walker A, Francis A, Didsbury M, Teixeira-Pinto A, Barton B, Prestidge C, Lancsar E, Mackie F, Kwon J, Howard K, Mallitt KA, Howell M, Jaure A, Hayes A, Raghunandan R, Petrou S, Lah S, McTaggart S, Craig JC, Wong G (2023) Longitudinal assessment of the health-related quality of life of children and adolescents with chronic kidney disease. Kidney Int 103(2):357–364. https://doi.org/10.1016/j.kint.2022.09.026
Purnell TS, Auguste P, Crews DC, Lamprea-Montealegre J, Olufade T, Greer R, Ephraim P, Sheu J, Kostecki D, Powe NR, Rabb H, Jaar B, Boulware LE (2013) Comparison of life participation activities among adults treated by hemodialysis, peritoneal dialysis, and kidney transplantation: a systematic review. Am J Kidney Dis 62(5):953–973. https://doi.org/10.1053/j.ajkd.2013.03.022
Riley P, Marks SD, Desai DY, Mushtaq I, Koffman G, Mamode N (2010) Challenges facing renal transplantation in pediatric patients with lower urinary tract dysfunction. Transplantation 89(11):1299–1307. https://doi.org/10.1097/tp.0b013e3181de5b8c
Marchal S, Kalfa N, Iborra F, Badet L, Karam G, Broudeur L, Branchereau J, Abdo N, Thuret R (2020) Long-term outcome of renal transplantation in patients with congenital lower urinary tract malformations: a multicenter study. Transplantation 104(1):165–171. https://doi.org/10.1097/TP.0000000000002746
Cornwell LB, Ingulli EG, Mason MD, Ewing E, Riddell JV (2021) Renal transplants due to congenital anomalies of the kidney and urinary tract (CAKUT) have better graft survival than non-CAKUT controls: analysis of over 10,000 patients. Urology 154:255–262. https://doi.org/10.1016/j.urology.2021.01.005
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097
First MR (1992) Renal transplantation for the nephrologist: new immunosuppressive drugs. Am J Kidney Dis 19(1):3–9. https://doi.org/10.1016/s0272-6386(12)70195-6
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibanes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196. https://doi.org/10.1097/SLA.0b013e3181b13ca2
Sterne JA, Hernan MA, Reeves BC, Savovic J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan AW, Churchill R, Deeks JJ, Hrobjartsson A, Kirkham J, Juni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schunemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF, Higgins JP (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. https://doi.org/10.1136/bmj.i4919
Artiles A, Dominguez A, Subiela JD, Boissier R, Campi R, Prudhomme T, Pecoraro A, Breda A, Burgos FJ, Territo A, Hevia V, Group E-YKTW (2023) Kidney transplant outcomes in elderly population: a systematic review and meta-analysis. Eur Urol Open Sci 51:13–25. https://doi.org/10.1016/j.euros.2023.02.011
Mesnard B, Territo A, Campi R, Hevia V, Andras I, Piana A, Pecoraro A, Boissier R, Prudhomme T, Transplantation EA-YAUgoK (2023) Kidney transplantation from elderly donors (> 70 years): a systematic review. World J Urol 41(3):695–707. https://doi.org/10.1007/s00345-023-04311-4
Prudhomme T, Mesnard B, Abbo O, Banuelos B, Territo A, Transplantation EAUYAUgoK, the EAUYAUgoPU (2023) Postoperative surgical complications after pediatric kidney transplantation in low weight recipients (<15 kg) a systematic review. Curr Opin Organ Transplant 28(4):297–308
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135. https://doi.org/10.1186/1471-2288-14-135
Haberal HB, Zakri R, Olsburgh J (2022) Medium and long-term clinical outcomes of kidney transplantation in patients with prune belly syndrome: a single-centre experience. Urology 169:245–249. https://doi.org/10.1016/j.urology.2022.08.023
Rickard M, Chua ME, Zu’bi F, Dos Santos J, Koyle MA, Lorenzo AJ, Farhat WA (2020) Comparative outcome analysis of pediatric kidney transplant in posterior urethral valves children with or without pretransplant Mitrofanoff procedure. Pediatr Transplant 24(8):e13798. https://doi.org/10.1111/petr.13798
Al-Khudairi N, Riley P, Desai DY, Reid C, Marks SD, Mamode N (2013) Interventions for impaired bladders in paediatric renal transplant recipients with lower urinary tract dysfunction. Transpl Int 26(4):428–434. https://doi.org/10.1111/tri.12063
Kaya Aksoy G, Koyun M, Dinckan A, Aliosmanoglu I, Gemici A, Gultekin E, Comak E, Akman S (2021) Graft survival in patients with lower urinary tract dysfunction. Exp Clin Transplant 19(2):125–130. https://doi.org/10.6002/ect.2018.0029
Christman MS, Canning DA, Schast AP, Baluarte HJ, Kaplan BS (2013) Renal transplantation into a diverted urinary system-is it safe in children? J Urol 190(2):678–682. https://doi.org/10.1016/j.juro.2013.02.019
Figueiredo R, Meireles D, Costa T, Mota C, Caldas Afonso A (2021) Renal transplant in pediatric patients with congenital abnormalities of the lower urinary tract. Exp Clin Transplant 19(4):310–315. https://doi.org/10.6002/ect.2020.0325
Aki FT, Aydin AM, Dogan HS, Donmez MI, Erkan I, Duzova A, Topaloglu R, Tekgul S (2015) Does lower urinary tract status affect renal transplantation outcomes in children? Transplant Proc 47(4):1114–1116. https://doi.org/10.1016/j.transproceed.2014.10.069
Luke PP, Herz DB, Bellinger MF, Chakrabarti P, Vivas CA, Scantlebury VP, Hakala TR, Jevnikar AM, Jain A, Shapiro R, Jordan ML (2003) Long-term results of pediatric renal transplantation into a dysfunctional lower urinary tract. Transplantation 76(11):1578–1582. https://doi.org/10.1097/01.TP.0000090866.00241.0C
Saad IR, Habib E, ElSheemy MS, Abdel-Hakim M, Sheba M, Mosleh A, Salah DM, Bazaraa H, Fadel FI, Morsi HA, Badawy H (2016) Outcomes of living donor renal transplantation in children with lower urinary tract dysfunction: a comparative retrospective study. BJU Int 118(2):320–326. https://doi.org/10.1111/bju.13347
Hebenstreit D, Csaicsich D, Hebenstreit K, Muller-Sacherer T, Berlakovich G, Springer A (2018) Long-term outcome of pediatric renal transplantation in boys with posterior urethral valves. J Pediatr Surg 53(11):2256–2260. https://doi.org/10.1016/j.jpedsurg.2018.07.003
Kara E, Sakaci T, Ahbap E, Sahutoglu T, Koc Y, Basturk T, Sevinc M, Akgol C, Kayalar AO, Ucar ZA, Unsal A, Seyahi N (2016) Posttransplant urinary tract infection rates and graft outcome in kidney transplantation for end-stage renal disease due to reflux nephropathy versus chronic glomerulonephritis. Transplant Proc 48(6):2065–2071. https://doi.org/10.1016/j.transproceed.2016.05.009
Lopez Pereira P, Ortiz R, Espinosa L, Martinez Urrutia MJ, Lobato R, Alonso A, Jaureguizar E (2014) Does bladder augmentation negatively affect renal transplant outcome in posterior urethral valve patients? J Pediatr Urol 10(5):892–897. https://doi.org/10.1016/j.jpurol.2014.01.011
Traxel E, DeFoor W, Minevich E, Reddy P, Alam S, Reeves D, Sheldon C (2011) Low incidence of urinary tract infections following renal transplantation in children with bladder augmentation. J Urol 186(2):667–671. https://doi.org/10.1016/j.juro.2011.03.155
Territo A, Bajeot AS, Mesnard B, Campi R, Pecoraro A, Hevia V, Piana A, Doumerc N, Breda A, Boissier R, Prudhomme T (2023) Open versus robotic-assisted kidney transplantation: a systematic review by the European Association of Urology (EAU)—Young Academic Urologists (YAU) Kidney Transplant Working Group. Actas Urol Esp (Engl Ed) 47(8):474–487. https://doi.org/10.1016/j.acuroe.2023.03.003
Salomon L, Fontaine E, Gagnadoux MF, Broyer M, Beurton D (1997) Posterior urethral valves: long-term renal function consequences after transplantation. J Urol 157(3):992–995. https://doi.org/10.1016/s0022-5347(01)65128-0
Oomen L, de Wall LL, Cornelissen EAM, Feitz WFJ, Bootsma-Robroeks C (2021) Prognostic factors on graft function in pediatric kidney recipients. Transplant Proc 53(3):889–896. https://doi.org/10.1016/j.transproceed.2020.10.017
Amesty MV, Garcia-Vaz C, Espinosa L, Martinez-Urrutia MJ, Lopez-Pereira P (2021) Long-term renal transplant outcome in patients with posterior urethral valves. prognostic factors related to bladder dysfunction management. Front Pediatr 9:646923. https://doi.org/10.3389/fped.2021.646923
Colgan R, Jaffe GA, Nicolle LE (2020) Asymptomatic bacteriuria. Am Fam Physician 102(2):99–104
Banuelos Marco B, Donmez MI, Geppert T, Prudhomme T, Campi R, Mesnard B, Hevia V, Boissier R, Pecoraro A, Territo A, Eau - Yau Kidney Transplant PWG, (2023) Renal transplantation in pediatric recipients: considerations and preoperative assessment strategies. Actas Urol Esp (Engl Ed) 47(6):351–359. https://doi.org/10.1016/j.acuroe.2023.03.002
Sager C, Burek C, Duran V, Corbetta JP, Weller S, Paz E, Lopez JC (2011) Outcome of renal transplant in patients with abnormal urinary tract. Pediatr Surg Int 27(4):423–430. https://doi.org/10.1007/s00383-010-2704-4
Jesus LE, Pippi Salle JL (2015) Pre-transplant management of valve bladder: a critical literature review. J Pediatr Urol 11(1):5–11. https://doi.org/10.1016/j.jpurol.2014.12.001
Basiri A, Otookesh H, Hosseini R, Simforoosh N, Moghaddam SM (2009) Kidney transplantation before or after augmentation cystoplasty in children with high-pressure neurogenic bladder. BJU Int 103(1):86–88. https://doi.org/10.1111/j.1464-410X.2008.08081.x
Salman B, Hassan A, Selim M, Abdelbaky T, Sultan S, Halawa A (2018) Renal transplant in abnormal bladder: treatment options and their effects on graft outcome. Exp Clin Transplant 16(6):660–664. https://doi.org/10.6002/ect.2016.0360
Nahas WC, Antonopoulos IM, Piovesan AC, Pereira LM, Kanashiro H, David-Neto E, Ianhez LE, Srougi M (2008) Comparison of renal transplantation outcomes in children with and without bladder dysfunction. a customized approach equals the difference. J Urol 179(2):712–716. https://doi.org/10.1016/j.juro.2007.09.094
Neild GH, Dakmish A, Wood S, Nauth-Misir R, Woodhouse CR (2004) Renal transplantation in adults with abnormal bladders. Transplantation 77(7):1123–1127. https://doi.org/10.1097/01.tp.0000116712.56265.78
McKay AM, Kim S, Kennedy SE (2019) Long-term outcome of kidney transplantation in patients with congenital anomalies of the kidney and urinary tract. Pediatr Nephrol 34(11):2409–2415. https://doi.org/10.1007/s00467-019-04300-z
Adams J, Mehls O, Wiesel M (2004) Pediatric renal transplantation and the dysfunctional bladder. Transpl Int 17(10):596–602. https://doi.org/10.1007/s00147-004-0784-6
Acknowledgements
None declared.
Funding
None declared.
Author information
Authors and Affiliations
Consortia
Contributions
Study concept and design: H.B.H., M.I.D., A.P., A.P., T.P., B.B.M., A.B., and A.T.; analysis and interpretation of data: H.B.H., M.I.D., and A.T.; drafting of the manuscript: H.B.H., M.I.D., A.P., A.P., T.P., B.B.M., A.L., R.C., R.B., A.B., and A.T.; statistical analysis: H.B.H. and M.I.D.; supervision: R.C., R.B., and A.B. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Haberal, H.B., Donmez, M.I., Piana, A. et al. A systematic review of kidney transplantation outcomes in patients with end-stage renal disease due to childhood lower urinary tract malformations. Int Urol Nephrol (2024). https://doi.org/10.1007/s11255-024-04079-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11255-024-04079-5