Abstract
Purpose
To determine baseline factors and surgical procedures associated with clinically meaningful improvement or deterioration of lower urinary tract symptoms (LUTS) after robot-assisted radical prostatectomy (RARP).
Methods
We retrospectively reviewed our RARP database and analyzed the changes in the International Prostate Symptom Score (IPSS) at baseline and 1, 3, 6, and 12 months postoperatively. Multivariable ordinal logistic regression analysis was performed to determine variables that predicted clinically meaningful improvement (∆IPSS ≤ -5) or deterioration (∆IPSS ≥ 5) in LUTS after RARP.
Results
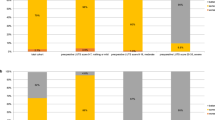
A total of 172 patients were eligible for analysis. Patients aged ≥ 70 reported a higher IPSS before and after RARP (all p < 0.05). Patients with a prostate volume of > 30 mL or body mass index of < 24 kg/m2 had worse preoperative LUTS; however, the difference disappeared after RARP. While patients with or without nerve-sparing (NS) had a similar preoperative LUTS burden, the NS group reported significantly lower IPSS than the non-NS group at all postoperative time points (p < 0.05). Twelve months after RARP, LUTS improved in 27% and worsened in 6% of patients in the NS group, compared with 20% and 24% of those in the non-NS group, respectively (p = 0.018). Preoperative IPSS (OR, 0.84; 95% CI, 0.79–0.89) and NS (OR, 0.39; 95% CI, 0.18–0.83) were independently associated with clinically meaningful changes of LUTS at 12 months after RARP.
Conclusion
Other than baseline LUTS severity, NS was the only independent factor associated with clinically meaningful changes in LUTS after RARP.



Similar content being viewed by others
References
Sung H, Ferlay J, Siegel RL et al (2021) Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249. https://doi.org/10.3322/caac.21660
Prabhu V, Taksler GB, Sivarajan G et al (2014) Radical prostatectomy improves and prevents age dependent progression of lower urinary tract symptoms. J Urol 191:412–417. https://doi.org/10.1016/j.juro.2013.08.010
Gordon A, Skarecky D, Osann K et al (2016) Quantification of long-term stability and specific relief of lower urinary tract symptoms (luts) after robot-assisted radical prostatectomy. Urology 93:97–103. https://doi.org/10.1016/j.urology.2016.03.028
Leyh-Bannurah S-R, Wagner C, Schuette A et al (2021) Improvement of quality of life and symptom burden after robot-assisted radical prostatectomy in patients with moderate to severe LUTS. Sci Rep 11:16757. https://doi.org/10.1038/s41598-021-95525-2
Schwartz EJ, Lepor H (1999) Radical retropubic prostatectomy reduces symptom scores and improves quality of life in men with moderate and severe lower urinary tract symptoms. J Urol 161:1185–1188
Gordon A, Skarecky DW, Ahlering T (2014) Long-term outcomes in severe lower urinary tract symptoms in men undergoing robotic-assisted radical prostatectomy. Urology 84:826–831. https://doi.org/10.1016/j.urology.2014.05.052
Ahn T, Roberts MJ, Strahan A et al (2019) Improved lower urinary tract symptoms after robot-assisted radical prostatectomy: implications for survivorship, treatment selection and patient counselling. BJU Int 123(Suppl 5):47–53. https://doi.org/10.1111/bju.14717
Matsushita K, Kent MT, Vickers AJ et al (2015) Preoperative predictive model of recovery of urinary continence after radical prostatectomy. BJU Int 116:577–583. https://doi.org/10.1111/bju.13087
Mungovan SF, Carlsson SV, Gass GC et al (2021) Preoperative exercise interventions to optimize continence outcomes following radical prostatectomy. Nat Rev Urol 18:259–281. https://doi.org/10.1038/s41585-021-00445-5
Seikkula H, Janssen P, Tutolo M et al (2017) Comparison of functional outcome after extended versus super-extended pelvic lymph node dissection during radical prostatectomy in high-risk localized prostate cancer. Front Oncol 7:280. https://doi.org/10.3389/fonc.2017.00280
Lee K, Shiota M, Takamatsu D et al (2022) Correlation between extended pelvic lymph node dissection and urinary incontinence at early phase after robot-assisted radical prostatectomy. Int J Urol. https://doi.org/10.1111/iju.15119
Eden CG, King D, Kooiman GG et al (2004) Transperitoneal or extraperitoneal laparoscopic radical prostatectomy: does the approach matter? J Urol 172:2218–2223. https://doi.org/10.1097/01.ju.0000144640.26182.41
Barry MJ, O’Leary MP (1995) Advances in benign prostatic hyperplasia. The developmental and clinical utility of symptom scores. Urol Clin North Am 22:299–307
Patel VR, Coelho RF, Palmer KJ, Rocco B (2009) Periurethral suspension stitch during robot-assisted laparoscopic radical prostatectomy: description of the technique and continence outcomes. Eur Urol 56:472–478. https://doi.org/10.1016/j.eururo.2009.06.007
Rocco B, Gregori A, Stener S et al (2007) Posterior reconstruction of the rhabdosphincter allows a rapid recovery of continence after transperitoneal videolaparoscopic radical prostatectomy. Eur Urol 51:996–1003. https://doi.org/10.1016/j.eururo.2006.10.014
Briganti A, Larcher A, Abdollah F et al (2012) Updated nomogram predicting lymph node invasion in patients with prostate cancer undergoing extended pelvic lymph node dissection: the essential importance of percentage of positive cores. Eur Urol 61:480–487. https://doi.org/10.1016/j.eururo.2011.10.044
Kim JH, Ha Y-S, Jeong SJ et al (2013) Impact of robot-assisted radical prostatectomy on lower urinary tract symptoms and predictive factors for symptom changes: a longitudinal study. Urology 81:787–793. https://doi.org/10.1016/j.urology.2012.12.038
Oszczudłowski M, Bilski K, Kozikowski M, Dobruch J (2022) De novo detrusor underactivity and other urodynamic findings after radical prostatectomy: a systematic review. Medicina 58:381. https://doi.org/10.3390/medicina58030381
Nguyen LN, Head L, Witiuk K et al (2017) The risks and benefits of cavernous neurovascular bundle sparing during radical prostatectomy: a systematic review and meta-analysis. J Urol 198:760–769. https://doi.org/10.1016/j.juro.2017.02.3344
Bayoud Y, de la Taille A, Ouzzane A et al (2015) International prostate symptom score is a predictive factor of lower urinary tract symptoms after radical prostatectomy. Int J Urol 22:283–287. https://doi.org/10.1111/iju.12681
Hikita K, Honda M, Shimizu R et al (2022) Longitudinal, 5-year long-term outcomes for urinary continence and quality of life after robot-assisted radical prostatectomy in Japanese patients. Low Urin Tract Symptoms 14:178–185. https://doi.org/10.1111/luts.12421
van der Poel HG, Tillier C, de Blok W, van Muilekom E (2012) Extended nodal dissection reduces sexual function recovery after robot-assisted laparoscopic prostatectomy. J Endourol 26:1192–1198. https://doi.org/10.1089/end.2012.0011
Sagalovich D, Calaway A, Srivastava A et al (2013) Assessment of required nodal yield in a high risk cohort undergoing extended pelvic lymphadenectomy in robotic-assisted radical prostatectomy and its impact on functional outcomes. BJU Int 111:85–94. https://doi.org/10.1111/j.1464-410X.2012.11351.x
Kallidonis P, Rai BP, Qazi H et al (2017) Critical appraisal of literature comparing minimally invasive extraperitoneal and transperitoneal radical prostatectomy: a systematic review and meta-analysis. Arab J Urol 15:267–279. https://doi.org/10.1016/j.aju.2017.07.003
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
Takeshi Soda contributed to the study conception and design, data acquisition, and data analysis. Takeshi Soda wrote the first draft of the manuscript. Hikari Otsuka and Shuhei Koike contributed to data acquisition and critical review of the manuscript. Takuya Okada contributed to data acquisition, critical review of the manuscript, and supervision. All authors commented on previous versions of the manuscript and read and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Institutional Review Board of the Medical Research Institute Kitano Hospital, approval number [P230100100].
Informed consent
Written informed consent was waived by the Institutional Review Board of the Medical Research Institute Kitano Hospital in view of the retrospective nature of the study and all the procedures being performed were part of the routine care.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Soda, T., Otsuka, H., Koike, S. et al. Baseline factors and surgical procedures affecting changes in lower urinary tract symptoms after robot-assisted radical prostatectomy: the impact of nerve-sparing. Int Urol Nephrol 56, 989–997 (2024). https://doi.org/10.1007/s11255-023-03859-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03859-9