Abstract
Purpose
Asymptomatic pyuria and bacteriuria are more prevalent in diabetic patients and may be associated with urinary tract infection (UTI). The aim of this study is to investigate the association between asymptomatic pyuria/bacteriuria at the initiation of SGLT2 inhibitor and UTI risk in female patients with type 2 diabetes.
Methods
The study was designed as a practical, single-center, prospective, cohort study. The female outpatients with type 2 diabetes initiated SGLT2 inhibitor were included. Patients who were symptomatic or treated in the past 3 months for urinary or genital tract infection, had a high risk for UTI were excluded. Hospitalization/antibiotic use for indications other than UTI were exclusion criteria during follow-up. All patients were followed up for 3 months. Pyuria and bacteriuria were exposure and, UTI was the outcome. Cumulative incidence and relative risk of UTI were analyzed for pyuria and bacteriuria.
Results
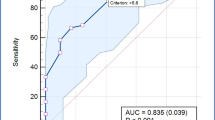
143 female patients were included among 1132 female type 2 diabetic patients. 13 patients were excluded during follow-up. 41.5% of the patients (n = 54) had pyuria and 28.5% (n = 37) had bacteriuria. The cumulative incidence of UTI was 20% in the whole cohort, 25,9% (n = 14/54) in the pyuria group and 18.9% (n = 7/37) in the bacteriuria group. The relative risk of UTI was 1.64 (95% CI: 0.82–3.26, p = 0.15) for pyuria, 0.92 (95% CI: 0.42–2.01, p = 0.84) for bacteriuria, and 1.2 (95% CI: 0.47–3.08, p = 0.69) for pyuria plus bacteriuria. Adjusted odd ratios revealed similar results.
Conclusions
Asymptomatic pyuria/bacteriuria at the initiation of SGLT2 inhibitors are not risk factors for UTI in women with type 2 diabetes.


Similar content being viewed by others
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request.
References
Heerspink HJL, Stefánsson BV, Correa-Rotter R, Chertow GM, Greene T, Hou FF, Mann JFE, McMurray JJV, Lindberg M, Rossing P, Sjöström CD, Toto RD, Langkilde AM, Wheeler DC (2020) Dapagliflozin in patients with chronic kidney disease. N Engl J Med 383(15):1436–1446. https://doi.org/10.1056/NEJMoa2024816
Wanner C, Inzucchi SE, Lachin JM, Fitchett D, von Eynatten M, Mattheus M, Johansen OE, Woerle HJ, Broedl UC, Zinman B (2016) Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med 375(4):323–334. https://doi.org/10.1056/NEJMoa1515920
Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, Silverman MG, Zelniker TA, Kuder JF, Murphy SA, Bhatt DL, Leiter LA, McGuire DK, Wilding JPH, Ruff CT, Gause-Nilsson IAM, Fredriksson M, Johansson PA, Langkilde AM, Sabatine MS (2019) Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med 380(4):347–357. https://doi.org/10.1056/NEJMoa1812389
Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, Mattheus M, Devins T, Johansen OE, Woerle HJ, Broedl UC, Inzucchi SE (2015) Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 373(22):2117–2128. https://doi.org/10.1056/NEJMoa1504720
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, Collins BS, Hilliard ME, Isaacs D, Johnson EL, Kahan S, Khunti K, Leon J, Lyons SK, Perry ML, Prahalad P, Pratley RE, Seley JJ, Stanton RC, Gabbay RA (2023) 9 Pharmacologic approaches to glycemic treatment: standards of care in diabetes-2023. Diabetes Care 46(Suppl 1):S140-s157. https://doi.org/10.2337/dc23-S009
Renko M, Tapanainen P, Tossavainen P, Pokka T, Uhari M (2011) Meta-analysis of the significance of asymptomatic bacteriuria in diabetes. Diabetes Care 34(1):230–235. https://doi.org/10.2337/dc10-0421
Nakano H, Oba K, Saito Y, Ouchi M, Yamashita N, Okamura K, Takai E, Mizuno S, Matsumura N, Inuzuka Y, Suzuki T (2001) Asymptomatic pyuria in diabetic women. J Nippon Med Sch 68(5):405–410. https://doi.org/10.1272/jnms.68.405
Boyko EJ, Fihn SD, Scholes D, Abraham L, Monsey B (2005) Risk of urinary tract infection and asymptomatic bacteriuria among diabetic and nondiabetic postmenopausal women. Am J Epidemiol 161(6):557–564. https://doi.org/10.1093/aje/kwi078
Geerlings SE, Stolk RP, Camps MJ, Netten PM, Collet JT, Schneeberger PM, Hoepelman AI (2001) Consequences of asymptomatic bacteriuria in women with diabetes mellitus. Arch Intern Med 161(11):1421–1427. https://doi.org/10.1001/archinte.161.11.1421
Harding GK, Zhanel GG, Nicolle LE, Cheang M (2002) Antimicrobial treatment in diabetic women with asymptomatic bacteriuria. N Engl J Med 347(20):1576–1583. https://doi.org/10.1056/NEJMoa021042
Köves B, Cai T, Veeratterapillay R, Pickard R, Seisen T, Lam TB, Yuan CY, Bruyere F, Wagenlehner F, Bartoletti R, Geerlings SE, Pilatz A, Pradere B, Hofmann F, Bonkat G, Wullt B (2017) Benefits and harms of treatment of asymptomatic bacteriuria: a systematic review and meta-analysis by the european association of urology urological infection guidelines panel. Eur Urol 72(6):865–868. https://doi.org/10.1016/j.eururo.2017.07.014
Dave CV, Schneeweiss S, Kim D, Fralick M, Tong A, Patorno E (2019) Sodium-glucose cotransporter-2 inhibitors and the risk for severe urinary tract infections: a population-based cohort study. Ann Intern Med 171(4):248–256. https://doi.org/10.7326/m18-3136
Fisher A, Fralick M, Filion KB, Dell’Aniello S, Douros A, Tremblay É, Shah BR, Ronksley PE, Alessi-Severini S, Hu N, Bugden SC, Ernst P, Lix LM (2020) Sodium-glucose co-transporter-2 inhibitors and the risk of urosepsis: A multi-site, prevalent new-user cohort study. Diabetes Obes Metab 22(9):1648–1658. https://doi.org/10.1111/dom.14082
Pelletier R, Ng K, Alkabbani W, Labib Y, Mourad N, Gamble JM (2021) Adverse events associated with sodium glucose co-transporter 2 inhibitors: an overview of quantitative systematic reviews. Ther Adv Drug Saf 12:2042098621989134. https://doi.org/10.1177/2042098621989134
Puckrin R, Saltiel MP, Reynier P, Azoulay L, Yu OHY, Filion KB (2018) SGLT-2 inhibitors and the risk of infections: a systematic review and meta-analysis of randomized controlled trials. Acta Diabetol 55(5):503–514. https://doi.org/10.1007/s00592-018-1116-0
Yang H, Choi E, Park E, Na E, Chung SY, Kim B, Han SY (2022) Risk of genital and urinary tract infections associated with SGLT-2 inhibitors as an add-on therapy to metformin in patients with type 2 diabetes mellitus: a retrospective cohort study in Korea. Pharmacol Res Perspect 10(1):e00910. https://doi.org/10.1002/prp2.910
Uitrakul S, Aksonnam K, Srivichai P, Wicheannarat S, Incomenoy S (2022) The incidence and risk factors of urinary tract infection in patients with type 2 diabetes mellitus using sglt2 inhibitors: a real-world observational study. Medicines (Basel) 9(12):59. https://doi.org/10.3390/medicines9120059
Kang M, Heo KN, Ah YM, Yang BR, Lee JY (2021) Age- and sex-specific risk of urogenital infections in patients with type 2 diabetes treated with sodium-glucose co-transporter 2 inhibitors: a population-based self-controlled case-series study. Maturitas 150:30–36. https://doi.org/10.1016/j.maturitas.2021.06.003
Hopf M, Kloos C, Wolf G, Müller UA, Müller N (2021) Effectiveness and safety of SGLT2 inhibitors in clinical routine treatment of patients with diabetes mellitus type 2. J Clin Med 10(4):571. https://doi.org/10.3390/jcm10040571
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
EA, AGC, ÖD, DÇ and MŞ designed the study. EA, and AGC collected the data. EA and MŞ performed the analyses. EA, AGC, ÖD, DÇ and MŞ interpreted the data. EA wrote the manuscript, EA, AGC, ÖD, DÇ and MŞ reviewed and made final approval of the manuscript. The corresponding author EA had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflict of interests
The authors declare no conflicts of interest and competing financial interests.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Bioethics Committee of the SBU Kanuni Education and Research Hospital, (Decision number: 2022/42).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Akkuş, E., Gökçay Canpolat, A., Demir, Ö. et al. Asymptomatic pyuria and bacteriuria are not risk factors for urinary tract infection in women with type 2 diabetes mellitus initiated SGLT2 inhibitors. Int Urol Nephrol 56, 1165–1172 (2024). https://doi.org/10.1007/s11255-023-03798-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03798-5