Abstract
Objective
To establish an automatic diagnostic system based on machine learning for preliminarily analysis of urodynamic study applying in lower urinary tract dysfunction (LUTD).
Methods
The eight most common conditions of LUTDs were included in the present study. A total of 527 eligible patients with complete data, from the year of 2015 to 2020, were enrolled in this study. In total, two global parameters (patients’ age and sex) and 13 urodynamic parameters were considered to be the input for machine learning algorithms. Three machine learning approaches were applied and evaluated in this study, including Decision Tree (DT), Logistic Regression (LR), and Support Vector Machine (SVM).
Results
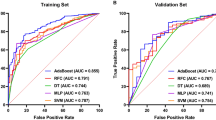
By applying machine learning algorithms into the 8 common LUTDs, the DT models achieved the AUC of 0.63–0.98, the LR models achieved the AUC of 0.73–0.99, and the SVM models achieved the AUC of 0.64–1.00. For mutually exclusive diagnoses of underactive detrusor and acontractile detrusor, we developed a classification model that classifies the patients into either of these two diseases or double-negative class. For this classification method, the DT models achieved the AUC of 0.82–0.85 and the SVM models achieved the AUC of 0.86–0.90. Among all these models, the LR and the SVM models showed better performance. The best model of these diagnostic tasks achieved an average AUC of 0.90 (0.90 ± 0.08).
Conclusions
An automatic diagnostic system was developed using three machine learning models in urodynamic studies. This automated machine learning process could lead to promising assistance and enhancements of diagnosis and provide more useful reference for LUTD treatment.



Similar content being viewed by others
Data availability
The data were obtained from UDS records in a single center, and the data was available with kindly request to corresponding authors.
Abbreviations
- LUTD:
-
Lower urinary tract dysfunction
- DT:
-
Decision tree
- LR:
-
Logistic regression
- SVM:
-
Support vector machine
- ML:
-
Machine learning
- AUC:
-
Area under the curve
- PFS:
-
Pressure flow study
- UDS:
-
Urodynamics
- Pves:
-
Vesical pressure
- Pabd:
-
Abdominal pressure
- Pdet:
-
Detrusor pressure
- Vinf:
-
Infused volume
- Qura:
-
Urinary flow rate
- ROC curve:
-
Receiver operator characteristic curve
- OAB:
-
Overactive bladder
References
Rosier PFWM, Schaefer W, Lose G et al (2017) International continence society good urodynamic practices and terms 2016: urodynamics, uroflowmetry, cystometry, and pressure-flow study. Neurourol Urodyn 36(5):1243–1260
Wessels F, Schmitt M, Krieghoff-Henning E et al (2021) Deep learning approach to predict lymph node metastasis directly from primary tumour histology in prostate cancer. BJU Int 128(3):352–360
Lebret T, Pignot G, Colombel M et al (2022) Artificial intelligence to improve cytology performances in bladder carcinoma detection: results of the VisioCyt test. BJU Int 129(3):356–363
Goecks J, Jalili V, Heiser LM, Gray JW (2020) How machine learning will transform biomedicine. Cell 181(1):92–101
Mincholé A, Rodriguez B (2019) Artificial intelligence for the electrocardiogram. Nat Med 25(1):22–23
Hogan S, Gammie A, Abrams P (2012) Urodynamic parameters and artefacts. Neurourol Urodyn 31(7):1104–1117
Sotoudeh H, Shafaat O, Bernstock JD, Brooks MD, Elsayed GA, Chen JA, Szerip P, Chagoya G, Gessler F, Sotoudeh E, Shafaat A, Friedman GK (2019) Artificial intelligence in the management of glioma: era of personalized medicine. Front Oncol 14(9):768
Birkhäuser V, Sartori AM, Bodmer NS et al (2020) Metaepidemiological inventory of diagnostic studies on urodynamics. Eur Urol Focus 6(5):880–908
Xiao Z, Jiapei W, Deyi L et al (2021) Urodynamics quality in southwest China: a multicenter random study. Chin J Urol 12:455–461
Raz O, Tse V, Chan L (2014) Urodynamic testing: physiological background, setting-up, calibration and artefacts. BJU Int 114(Suppl 1):22–28
Bentellis I, Guérin S, Khene ZE et al (2021) Artificial intelligence in functional urology: how it may shape the future. Curr Opin Urol 31(4):385–390
Sonke GS, Heskes T, Verbeek AL et al (2000) Prediction of bladder outlet obstruction in men with lower urinary tract symptoms using artificial neural networks. J Urol 163(1):300–305
Wadie BS, Badawi AM, Abdelwahed M et al (2006) Application of artificial neural network in prediction of bladder outlet obstruction: a model based on objective, noninvasive parameters. Urology 68(6):1211–1214
Niederhauser T, Gafner ES, Cantieni T et al (2018) Detection and quantification of overactive bladder activity in patients: can we make it better and automatic? Neurourol Urodyn 37(2):823–831
Wang HS, Cahill D, Panagides J et al (2021) Pattern recognition algorithm to identify detrusor overactivity on urodynamics. Neurourol Urodyn 40(1):428–434
Cullingsworth ZE, Kelly BB, Deebel NA et al (2018) Automated quantification of low amplitude rhythmic contractions (LARC) during real-world urodynamics identifies a potential detrusor overactivity subgroup. PLoS ONE 13(8):e0201594
Rantell A, Dolan L, Bonner L et al (2016) Minimum standards for continence care in the UK. Neurourol Urodyn 35(3):400–406
Panicker JN (2020) Neurogenic bladder: epidemiology, diagnosis, and management. Semin Neurol 40(5):569–579
Stöhrer M, Blok B, Castro-Diaz D, Chartier-Kastler E, Del Popolo G, Kramer G, Pannek J, Radziszewski P, Wyndaele J-J (2009) EAU guidelines on neurogenic lower urinary tract dysfunction. Eur Urol 56(1):81–88
Acknowledgements
We gratefully acknowledge Mr. Jingwen Chen and Mr. Yiran Sun in the Department of Urology to have performed all of the urodynamic studies in the past ten years in our center.
Funding
The present study was supported by Peking University People’s Hospital Scientific Research Development Funds (RDH2019-04) and National Natural Science Foundation of China (grant no. 81970660).
Author information
Authors and Affiliations
Contributions
Design and conduct of study, KX, HW, WZ; Manuscript draft, ZD, WZ; Acquisition of data, QW, ZD; Analysis performs, FS, HW; Critical revision and final approval, KX, KB, WZ, HK, DS.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors state a conflict of interest.
Ethical approval
The present study was approved by Ethics Review Committee of Peking University People’s Hospital (2022PHB098-001) and performed in line with international ethics norms.
Patient consent statement
Not required for the natural parameters of retrospective study. Permission to reproduce material from other sources. Reasonable request to corresponding authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ding, Z., Zhang, W., Wang, H. et al. An automatic diagnostic system for the urodynamic study applying in lower urinary tract dysfunction. Int Urol Nephrol 56, 441–449 (2024). https://doi.org/10.1007/s11255-023-03795-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03795-8