Abstract
Background
Metabolic syndrome, a significant risk factor for cardiovascular mortality in patients with end-stage renal disease, profoundly impacts patient prognosis and survival. Despite its clinical importance, the prevalence of metabolic syndrome remains unexplored in this population. Therefore, the objective of this study was to systematically assess the prevalence of metabolic syndrome among patients with end-stage renal disease and raise awareness among healthcare professionals.
Methods
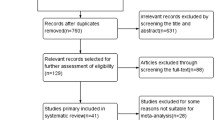
We conducted a comprehensive search in CNKI, WANFANG, WeiPu, CBM, PubMed, Web of Science, EMBASE, and The Cochrane Library databases. The search time was until August 21, 2023. Standardized tables were employed for data extraction and imported into Stata 16.0 software for subsequent meta-analysis. A random-effects model was employed to estimate combined prevalence and 95% confidence intervals. Subgroup and sensitivity analyses were conducted to explore potential sources of heterogeneity, while publication bias was evaluated using a funnel plot and Egger's test. This study has been registered with PROSPERO under the registration number CRD42023456284.
Results
This meta-analysis comprised 35 studies involving a total of 14,202 participants. The pooled prevalence estimate for metabolic syndrome was 49.0% [95% CI (46.0,53.0)]. We conducted subgroup analyses based on participant characteristics, gender distribution, publication year, national economic status, diagnostic criteria employed, and components of metabolic syndrome.
Conclusions
The prevalence of metabolic syndrome is higher among patients with end-stage renal disease, necessitating early prevention and control measures to reduce its incidence and delay the progression of the disease, thereby improving patient life expectancy.





Similar content being viewed by others
References
Shu KH, Wu MJ, Chen CH et al (2014) Short-term prospective study of metabolic syndrome in renal transplant recipients. Transplant Proc 46(2):540–542. https://doi.org/10.1016/j.transproceed.2013.11.031
Kim HJ, Lee J, Chae DW et al (2019) Serum klotho is inversely associated with metabolic syndrome in chronic kidney disease: results from the KNOW-CKD study. BMC Nephrol. https://doi.org/10.1186/s12882-019-1297-y
Zhang X, Lerman LO (2017) The metabolic syndrome and chronic kidney disease. Transl Res 183:14–25. https://doi.org/10.1016/j.trsl.2016.12.004
Tu SF, Chou YC, Sun CA, Hsueh SC, Yang T (2012) The prevalence of metabolic syndrome and factors associated with quality of dialysis among hemodialysis patients in Southern Taiwan. Article Global J Health Sci 4(5):53–62. https://doi.org/10.5539/gjhs.v4n5p53
Alswat KA, Althobaiti A, Alsaadi K et al (2017) Prevalence of Metabolic Syndrome Among the End-Stage Renal Disease Patients on Hemodialysis. J Clin Med Res 9(8):687–694
Zhang RN, Hao HF, Zhang W et al (2019) Clinical characterization and prognostic implications of metabolic syndrome in patients undergoing peritoneal dialysis at a Chinese center. J Int Med Res 47(11):5573–5583. https://doi.org/10.1177/0300060519875335
Navaneethan SD, Schold JD, Kirwan JP et al (2013) Metabolic syndrome, ESRD, and death in CKD. Clin J Am Soc Nephrol 8(6):945–952. https://doi.org/10.2215/cjn.09870912
Boronat M, Bosch E, Lorenzo D et al (2016) Prevalence and determinants of the metabolic syndrome among subjects with advanced nondiabetes-related chronic kidney disease in Gran Canaria. Spain Ren Fail 38(2):198–203. https://doi.org/10.3109/0886022x.2015.1117904
Sanguankeo A, Upala S (2018) Metabolic Syndrome Increases Mortality Risk in Dialysis Patients: A Systematic Review and Meta-Analysis. Int J Endocrinol Metab. https://doi.org/10.5812/ijem.61201
Greffin S, André MB, Matos JPS et al (2017) Chronic kidney disease and metabolic syndrome as risk factors for cardiovascular disease in a primary care program. J Bras Nefrol Jul-Sep 39(3):246–252. https://doi.org/10.5935/0101-2800.20170040
Moher D, Shamseer L, Clarke M et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. https://doi.org/10.1186/2046-4053-4-1
Shamseer L, Moher D, Clarke M et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. https://doi.org/10.1136/bmj.g7647
Zeng XT, Liu H, Chen X et al (2012) Meta-analysis Series IV: Quality assessment tools for observational studies. Chine J Evid-Based Cardiovasc Med 4(04):297–299. https://doi.org/10.3969/j.1674-4055.2012.04.004
Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, Botella J (2006) Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods 11(2):193–206. https://doi.org/10.1037/1082-989x.11.2.193
Tsangalis G, Papaconstantinou S, Kosmadakis G, Valis D, Zerefos N (2007) Prevalence of the metabolic syndrome in hemodialysis. Art Int J Artif Org 30(2):118–123. https://doi.org/10.1177/039139880703000206
Zhang WX, Gong ZF, Peng XM et al (2008) Prevalence of the metabolic syndrome in maintenance hemodialysis patients. Int Med 1:21–24
Jiang N, Qian J, Lin A, Lindholm B, Axelsson J, Yao Q (2008) Initiation of glucose-based peritoneal dialysis is associated with increased prevalence of metabolic syndrome in non-diabetic patients with end-stage renal disease. Art Blood Purific 26(5):423–428. https://doi.org/10.1159/000153248
Park JT, Chang TI, Kim DK et al (2009) Association of white blood cell count with metabolic syndrome in patients undergoing peritoneal dialysis. Art Metab Clin Exp 58(10):1379–1385. https://doi.org/10.1016/j.metabol.2009.05.002
Chen YH, Pang HH, Zhu ML et al (2010) Prevalence of metabolic syndrome and analysis of risk factors among patients with maintenance hemodialysis. J Shang Jiao Tong Univ (Med Sci) 30(05):558–561
Stolic RV, Trajkovic GZ, Peric VM et al (2010) Impact of Metabolic Syndrome and Malnutrition on Mortality in Chronic Hemodialysis Patients. Art J Renal Nutr 20(1):38–43. https://doi.org/10.1053/j.jrn.2009.01.021
Zhang CH, Shen S, Yu L, Wang SX (2011) Analysis on risk factors for metabolic syndrome in patients with maintaining hemodialysis. Chin J Gen Practit 10(8):543–547. https://doi.org/10.3760/cma.j.issn.1671-7368.2011.08.004
Jalalzadeh M, Mohammadi R, Mirzamohammadi F, Ghadiani MH (2011) Prevalence of Metabolic Syndrome in a Hemodialysis Population. Iran J Kidney Dis 5(4):248–254
Borazan A, Ucar E, Gursu M, Emir I, Ozturk Y (2012) Relationship between metabolic syndrome and inflammation in peritoneal dialysis patients. Eur J Inflamm 10(2):203–207. https://doi.org/10.1177/1721727x1201000205
Shahrokh S, Heydarian P, Ahmadi F, Saddadi F, Razeghi E (2012) Association of inflammatory biomarkers with metabolic syndrome in hemodialysis patients. Ren Fail 34(9):1109–1113. https://doi.org/10.3109/0886022x.2012.713280
Marjani A, Moujerloo M, Hezarkhani S (2013) Age related metabolic syndrome among hemodialysis patients in Gorgan. Iran Art Open Biochem J 7(1):15–18. https://doi.org/10.2174/1874091X01307010015
Prasad N, Sinha A, Gupta A et al (2013) Effect of metabolic syndrome on clinical outcomes of non-diabetic peritoneal dialysis patients in India. Nephrology 18(10):657–664. https://doi.org/10.1111/nep.12124
Dong J, Wang Q, Chen MH et al (2014) Associations between serum-intact parathyroid hormone, serum 25-hydroxyvitamin d, oral vitamin d analogs and metabolic syndrome in peritoneal dialysis patients: a multi-center cross-sectional study. Perit Dial Int 34(4):447–455. https://doi.org/10.3747/pdi.2013.00001
Szeto CC, Kwan BC, Chow KM et al (2014) Metabolic syndrome in peritoneal dialysis patients: choice of diagnostic criteria and prognostic implications. Clin J Am Soc Nephrol 9(4):779–787. https://doi.org/10.2215/cjn.06620613
Zhang JB, Hu XZ, Zhang Y et al (2015) Multicenter survey on the prevalence and risk factors of metabolic syndrome among patients with maintenance hemodialysis. J Pract Med 18:3075–3078. https://doi.org/10.3969/j.issn.1006-5725.2015.18.045
Jalalzadeh M, Mousavinasab N, Soloki M, Miri R, Ghadiani MH, Hadizadeh M (2015) Association between metabolic syndrome and coronary heart disease in patients on hemodialysis. Nephro-Urol Month. https://doi.org/10.5812/numonthly.25560
Kubrusly M, Oliveira CM, Simões PS et al (2015) Prevalence of metabolic syndrome according to NCEP-ATP III and IDF criteria in patients on hemodialysis. J Bras Nefrol Jan-Mar 37(1):72–78. https://doi.org/10.5935/0101-2800.20150011
Vogt BP, Ponce D, Caramori JC (2016) Anthropometric Indicators Predict Metabolic Syndrome Diagnosis in Maintenance Hemodialysis Patients. Nutr Clin Pract 31(3):368–374. https://doi.org/10.1177/0884533615601849
Li WW, Shan WW, Zhang ZJ et al (2017) Relationship between hyperuricemia and metabolic syndrome in non-diabetic patients undergoing peritoneal dialysis. Jian Med J. 43(3):160–163
Wang XL, Chen JH (2017) Prevalence of metabolic syndrome in maintenance hemodialysis patients. China Health Care&Nutrition 27(28):336–337. https://doi.org/10.3969/j.issn.1004-7484.2017.28.486
Tek NA, Şanlier N, Akbulut G, Öneç K, Erten Y (2017) Assessment of nutritional status and metabolic syndrome in peritoneal dialysis patients: A pilot study. Gazi Med J 28(3):191–195
Meng PH, Wei F, Wang Z et al (2018) Relationship between low vitamin D level and metabolic syndrome in maintenance hemodialysis patients. Chin J Nephrol 34(1):10–16. https://doi.org/10.3760/cma.j.issn.1001-7097.2018.01.003
Duong TV, Wong TC, Chen HH et al (2018) Inadequate dietary energy intake associates with higher prevalence of metabolic syndrome in different groups of hemodialysis patients: a clinical observational study in multiple dialysis centers. Bmc Nephrol. https://doi.org/10.1186/s12882-018-1041-z
Jiang R, Ma S, Wang XY et al (2019) Association between metabolic syndrome and prognosis in patients with peritoneal dialysis. Chine J Nephrol 35(3):184–190. https://doi.org/10.3760/cma.j.issn.1001-7097.2019.03.004
Xiao W, Wen XQ, Zeng Y et al (2019) Influencing factors of metabolic syndrome among patients with maintenance hemodialysis. J Hunan Normal Univer (Med Sci) 16(3):48–51. https://doi.org/10.3969/j.issn.1673-016X.2019.03.015
Delautre A, Chantrel F, Dimitrov Y et al (2020) Metabolic syndrome in haemodialysis patients: Prevalence, determinants and association to cardiovascular outcomes. BMC Nephrol. https://doi.org/10.1186/s12882-020-02004-3
El Ati Z, Machfar H, Boussafa H et al (2020) Metabolic syndrome, malnutrition, and its associations with cardiovascular and all-cause mortality in hemodialysis patients: Follow-up for three years. Saudi J Kidney Dis Transplant Off Publ Saudi Cent Org Transplant Saudi Arabia 31(1):129–135. https://doi.org/10.4103/1319-2442.279932
Syukri M, Virnardo R, Salwani D, Abdullah SH, Marthoenis, (2020) The prevalence and associated factors of metabolic syndrome among patients with end-stage renal failure undergoing hemodialysis in Indonesia. Diab Metab Synd Clin Res Rev 14(6):2069–2072
Wung CH, Chung CY, Wu PY et al (2021) Associations between Metabolic Syndrome and Obesity-Related Indices and Bone Mineral Density T-Score in Hemodialysis Patients. J Personal Med. https://doi.org/10.3390/jpm11080775
Song P, Zhao Y, Zhang H et al (2022) Comparison of Inflammatory Markers in the Diagnosis of Metabolic Syndrome in Hemodialysis Patients: A Multicenter Observational Study. Diab Metab Syndr Obes. https://doi.org/10.2147/DMSO.S370835
Kobayashi S, Mochida Y, Ishioka K et al (2023) Malnutrition and Insulin Resistance May Interact with Metabolic Syndrome in Prevalent Hemodialysis Patients. J Clin Med. https://doi.org/10.3390/jcm12062239
Yang Y, Li Q, Long Y, Yuan J, Zha Y (2023) Associations of metabolic syndrome, its severity with cognitive impairment among hemodialysis patients. Diabetol Metab Syndr. https://doi.org/10.1186/s13098-023-01080-3
Zhou J, Yuan W, Guo Y et al (2023) Asprosin is positively associated with metabolic syndrome in hemodialysis patients: a cross-sectional study. Ren Fail. https://doi.org/10.1080/0886022X.2023.2220425
Chowdhury MZI, Anik AM, Farhana Z et al (2018) Prevalence of metabolic syndrome in Bangladesh: a systematic review and meta-analysis of the studies. BMC Publ Health. https://doi.org/10.1186/s12889-018-5209-z
Yang GX, Wu YB, Wang X et al (2012) Relationship between microinflammation and cardiovascular events in maintenance hemodialysis patients. J Pract Med 28(02):251–253
Prasad GV (2014) Metabolic syndrome and chronic kidney disease: Current status and future directions. World J Nephrol 3(4):210–219. https://doi.org/10.5527/wjn.v3.i4.210
Sweigert PJ, Bansal VK, Hoppensteadt DA, Saluk JL, Syed DA, Fareed J (2017) Inflammatory and Metabolic Syndrome Biomarker Analysis of Vascular Outcomes in End-stage Renal Disease. Int J Angiol 26(1):43–48. https://doi.org/10.1055/s-0036-1593409
Wissing KM, Pipeleers L (2014) Obesity, metabolic syndrome and diabetes mellitus after renal transplantation: prevention and treatment. Transplant Rev (Orlando) 28(2):37–46. https://doi.org/10.1016/j.trre.2013.12.004
Türker PF, Kiziltan G, Güller Arslan D, Gencaslan D, Demircan E (2011) Comparison of obesity and metabolic syndrome frequency in hemodialysis and continuous ambulatory peritoneal dialysis patients. Conf Abst Obes Rev 12:195–196. https://doi.org/10.1111/j.1467-789X.2011.00889.x
Tbahriti HF, Meknassi D, Moussaoui R et al (2013) Inflammatory status in chronic renal failure: The role of homocysteinemia and pro-inflammatory cytokines. World J Nephrol 2(2):31–37. https://doi.org/10.5527/wjn.v2.i2.31
Harmankaya O, Akalin N, Akay H et al (2015) Comparison of risk factors for cardiovascular disease in hemodialysis and peritoneal dialysis patients. Clinics (Sao Paulo) 70(9):601–605. https://doi.org/10.6061/clinics/2015(09)01
Hami M, Sabbagh MG, Sefidgaran A, Mojahedi MJ (2017) Prevalence of the metabolic syndrome in kidney transplant recipients: A single-center study. Saudi J Kidney Dis Transpl Mar-Apr 28(2):362–367. https://doi.org/10.4103/1319-2442.202786
Pucci G, Alcidi R, Tap L, Battista F, Mattace-Raso F, Schillaci G (2017) Sex- and gender-related prevalence, cardiovascular risk and therapeutic approach in metabolic syndrome: A review of the literature. Pharmacol Res 120:34–42. https://doi.org/10.1016/j.phrs.2017.03.008
Ye Y, Zhou Q, Dai W et al (2023) Gender differences in metabolic syndrome and its components in southern china using a healthy lifestyle index: a cross-sectional study. BMC Pub Health. https://doi.org/10.1186/s12889-023-15584-0
Dimitrijevic Z, Jovanovic A, Cvetkovic M, Vrecic T, Kostic E, Mitic B (2019) Associations of Cardiovascular and All-Cause Mortality with Metabolic Syndrome in Hemodialysis Patients: A Prospective Single-Center Study. Med (Kaunas). https://doi.org/10.3390/medicina55100694
Kittiskulnam P, Thokanit NS, Katavetin P et al (2018) The magnitude of obesity and metabolic syndrome among diabetic chronic kidney disease population: A nationwide study. PLoS ONE. https://doi.org/10.1371/journal.pone.0196332
Marcotte-Chénard A, Deshayes TA, Ghachem A, Brochu M (2019) Prevalence of the metabolic syndrome between 1999 and 2014 in the United States adult population and the impact of the 2007–2008 recession: an NHANES study. Appl Physiol Nutr Metab 44(8):861–868. https://doi.org/10.1139/apnm-2018-0648
Saklayen MG (2018) The Global Epidemic of the Metabolic Syndrome. Curr Hypertens Rep. https://doi.org/10.1007/s11906-018-0812-z
Ren Q, Chen D, Liu X et al (2022) Derivation and Validation of a Prediction Model of End-Stage Renal Disease in Patients With Type 2 Diabetes Based on a Systematic Review and Meta-analysis. Front Endocrinol (Lausanne). https://doi.org/10.3389/fendo.2022.825950
Cheng HT, Xu X, Lim PS, Hung KY (2021) Worldwide Epidemiology of Diabetes-Related End-Stage Renal Disease, 2000–2015. Diabetes Care 44(1):89–97. https://doi.org/10.2337/dc20-1913
Misra A, Khurana L (2008) Obesity and the metabolic syndrome in developing countries. J Clin Endocrinol Metab 93(11 Suppl 1):S9-30. https://doi.org/10.1210/jc.2008-1595
Misra A, Bhardwaj S (2014) Obesity and the metabolic syndrome in developing countries: focus on South Asians. Nestle Nutr Inst Workshop Ser 78:133–140. https://doi.org/10.1159/000354952
Lao XQ, Ma WJ, Sobko T et al (2014) Dramatic escalation in metabolic syndrome and cardiovascular risk in a Chinese population experiencing rapid economic development. BMC Publ Health. https://doi.org/10.1186/1471-2458-14-983
Ebrahimi H, Emamian MH, Khosravi A, Hashemi H, Fotouhi A (2019) Comparison of the accuracy of three diagnostic criteria and estimating the prevalence of metabolic syndrome: A latent class analysis. J Res Med Sci 24:108. https://doi.org/10.4103/jrms.JRMS_858_18
Xie Q, Zhang AH, Chen SY et al (2012) Metabolic syndrome is associated with better nutritional status, but not with cardiovascular disease or all-cause mortality in patients on haemodialysis. Arch Cardiovasc Dis 105(4):211–217. https://doi.org/10.1016/j.acvd.2012.01.012
Lo WK (2016) Metabolic syndrome and obesity in peritoneal dialysis. Kidney Res Clin Pract 35(1):10–14. https://doi.org/10.1016/j.krcp.2015.12.007
Xing Y, Xu S, Jia A et al (2018) Recommendations for revision of Chinese diagnostic criteria for metabolic syndrome: A nationwide study. J Diabetes 10(3):232–239. https://doi.org/10.1111/1753-0407.12578
Cabral LS, Cherubini PA, de Oliveira MA, Bianchini L, Torres CM, Bianchin MM (2017) Diagnostic Yield and Accuracy of Different Metabolic Syndrome Criteria in Adult Patients with Epilepsy. Front Neurol 8:460. https://doi.org/10.3389/fneur.2017.00460
Ecder SA, Sasak G (2019) Body Shape Index Predicts Metabolic Syndrome and Insulin Resistance in Renal Transplant Recipients. Transplant Proc 51(7):2334–2338. https://doi.org/10.1016/j.transproceed.2019.01.172
Johns BR, Pao AC, Kim SH (2012) Metabolic syndrome, insulin resistance and kidney function in non-diabetic individuals. Nephrol Dial Transplant 27(4):1410–1415. https://doi.org/10.1093/ndt/gfr498
AlShelleh S, AlAwwa I, Oweis A et al (2019) Prevalence of metabolic syndrome in dialysis and transplant patients. Diabetes Metab Syndr Obes 12:575–579. https://doi.org/10.2147/dmso.S200362
Funding
Funding provided by Ministry of Science and Technology of the People's Republic of China (Grant number: 2020YFC2003104).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Du, Q., Jiang, Y. & Liu, Y. Prevalence of metabolic syndrome in patients with end-stage renal disease: a systematic review and meta-analysis. Int Urol Nephrol 56, 1057–1069 (2024). https://doi.org/10.1007/s11255-023-03790-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03790-z