Abstract
Purpose
Few studies have examined the risk factors for postoperative healthcare resource utilization (HRU) among minimally invasive partial nephrectomy (MIPN), minimally invasive prostatectomy (MIP), and cystectomy (Cx). The aim of this study is to assess if operative duration (OD) is a predictor of HRU in this population.
Methods
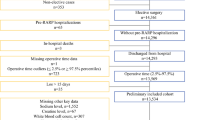
The ACS-NSQIP database was filtered for MIPN, MIP, and Cx. Patient characteristics and intraoperative variables were examined. HRU was defined as prolonged length of stay (LOS), unplanned readmission within 30 days, and discharge to continued care facility. Multivariate regression analysis was used to identify independent predictors of HRU.
Results
18,904 MIPN, 50,807 MIP, and 12,451 Cx were included. For MIPN, HRU was seen in 13.9% of cases < 1.75 h, increasing to 36.2% in OD > 4.5 h (p < 0.001). For MIP, HRU was seen in 10.6% of OD < 2 h, increasing to 32.2% for OD > 4.9 h (p < 0.001). For Cx, 57% of those with OD > 8.5 h required HRU compared to 42.1% for OD < 3.3 h (p < 0.001). On multivariate analyses, OD was an independent predictor for increased HRU for all procedures regardless of patient characteristics or comorbidities. For MIPN, OD > 4.5 h had 3.5-fold increased use of HRU (p < 0.001). For MIP, OD > 5 h had 3.7-fold increased use of HRU (p < 0.001). For Cx, OD > 8.5 h demonstrated a twofold increased use of HRU (p < 0.001).
Conclusions
OD during MIPN, MIP, and Cx is an independent predictor of increased HRU irrespective of patient comorbidities. Patients with OD > 4.5 h for MIPN, > 5 h for MIP, and > 8.5 h for Cx have 3.5-fold, 3.7-fold, and twofold increased risk of HRU, respectively.

Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author, ST.
References
Cheng H, Clymer JW, Po-Han Chen B et al (2018) Prolonged operative duration is associated with complications: a systematic review and meta-analysis. J Surg Res 229:134–144
Cheng H, Po-Han Chen B, Soleas IM, Ferko NC, Cameron CG, Hinoul P (2017) Prolonged operative duration increases risk of surgical site infections: A systematic review. Surg Infect 18(6):722–735
Procter LD, Davenport DL, Bernard AC, Zwischenberger JB (2010) General surgical operative duration is associated with increased risk-adjusted infectious complication rates and length of hospital stay. J Am Coll Surg 210(1):60-65.e1–2
Hardy KL, Davis KE, Constantine RS et al (2014) The impact of operative time on complications after plastic surgery: a multivariate regression analysis of 1753 cases. Aesthet Surg J 34(4):614–622
Golebiowski A, Drewes C, Gulati S, Jakola AS, Solheim O (2015) Is duration of surgery a risk factor for extracranial complications and surgical site infections after intracranial tumor operations? Acta Neurochir (Wien) 157(2):235–240
Harris AM, James A, Dugan A, Bylund J (2019) Increased operative duration in minimally invasive partial nephrectomy is associated with significantly increased risk of 30-day morbidity. J Endourol 33(7):549–556
Huang KH, Kaplan AL, Carter SC, Lipsitz SR, Hu JC (2014) The impact of radical prostatectomy operative time on outcomes and costs. Urology 83(6):1265–1271
Tan WS, Lamb BW, Kelly JD (2015) Complications of radical cystectomy and orthotopic reconstruction. Adv Urol 2015:323157
McBride A, McKibben MJ, Vukina J et al (2014) Longer operative times predict increased length of stay after cystectomy. J Am Coll Surg 219(3):S146
Taylor BL, Xia L, Guzzo TJ, Scherr DS, Hu JC (2019) Frailty and greater health care resource utilization following major urologic oncology surgery. Eur Urol Oncol 2(1):21–27
Butt ZM, Fazili A, Tan W et al (2009) Does the presence of significant risk factors affect perioperative outcomes after robot-assisted radical cystectomy? BJU Int 104(7):986–990
Harris AM, James A, Dugan A, Bylund J (2020) Increased operative duration of minimally invasive prostatectomy is associated with significantly increased risk of 30-Day morbidity. Urol Pract 7(1):21–27
Smith CG, Davenport DL, Gorski J et al (2019) Clinical factors associated with longer hospital stay following ovarian cancer surgery. Healthcare 7(3):85
Chiu HC, Lin YC, Hsieh HM, Chen HP, Wang HL, Wang JY (2017) The impact of complications on prolonged length of hospital stay after resection in colorectal cancer: a retrospective study of Taiwanese patients. J Int Med Res 45(2):691–705
Osborn DJ, Dmochowski RR, Kaufman MR, Milam DF, Mock S, Reynolds WS (2014) Cystectomy with urinary diversion for benign disease: indications and outcomes. Urology 83(6):1433–1437
Routh JC, Bacon DR, Leibovich BC, Zincke H, Blute ML, Frank I (2008) How long is too long? The effect of the duration of anaesthesia on the incidence of non-urological complications after surgery. BJU Int 102(3):301–304
Lehtonen EJ, Hess MC, McGwin G Jr, Shah A, Godoy-Santos AL, Narange S (2018) Risk factors for early hospital readmission following total knee arthroplasty. Acta Ortop Bras 26(5):309–313
Gupta PK, Fernandes-Taylor S, Ramanan B, Engelbert TL, Kent KC (2014) Unplanned readmissions after vascular surgery. J Vasc Surg 59(2):473–482
Baack Kukreja J, Kamat AM (2017) Strategies to minimize readmission rates following major urologic surgery. Ther Adv Urol 9(5):111–119
Suskind AM, Jin C, Cooperberg MR et al (2016) Preoperative frailty is associated with discharge to skilled or assisted living facilities after urologic procedures of varying complexity. Urology 97:25–32
Divatia J, Ranganathan P (2015) Can we improve operating room efficiency? J Postgrad Med 61(1):1–2
6 Cornerstones of Operating Room Efficiency: Best Practices for Each. https://www.beckershospitalreview.com/or-efficiencies/6-cornerstones-of-operating-room-efficiency-best-practices-for-each.html. Accessed 28 Sept 2020
Welk B, Winick-Ng J, McClure A, Vinden C, Dave S, Pautler S (2016) The impact of teaching on the duration of common urological operations. Can Urol Assoc J 10(5–6):172–178
Funding
The authors did not receive financial support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
JPM: Manuscript writing/editing. ST: Project development, manuscript editing. AB: Data analysis, AH: Project development, data collecting/management, manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest relevant to the content of this article.
Ethics approval and consent to participate
Approval of the research protocol by an Institutional Reviewer Board and the approval number: N/A. This is an observational study using a de-identified database. No formal IRB approval or other ethical approval is required.
Informed consent
N/A. Due to the de-identified nature of the database used in this study, informed consent was not required to obtain data. Registry and the Registration No. of the study/trial: N/A.
Animal studies
Not available.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Morin, J., Teplitsky, S., Bettis, A. et al. Operative duration as independent predictor of increased postoperative healthcare utilization. Int Urol Nephrol 56, 23–28 (2024). https://doi.org/10.1007/s11255-023-03785-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03785-w