Abstract
Objective
To examine the association between dyslipidemia and kidney stone disease (KSD).
Methods
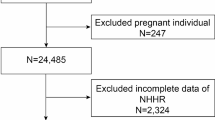
A cross-sectional study data from 2007 to 2020 National Health and Nutrition Examination Survey (NHANES) were analyzed. Multivariate logistic regression was conducted with serum lipid levels as the exposure and presence of KSD as the outcome, and included adjustment for confounders and subgroup analysis.
Results
A total of 38,617 participants were enrolled and classified into two groups according to whether they ever had (n = 3689) or did not have (n = 34,928) KSD. After multivariate logistic regression models, compared to quartile 1 (Q1) of lipid profile, the participants in Q3 (OR 0.8380; 95 CI 0.7380, 0.9515, P < 0.01) and Q4 (OR 0.7373; 95 CI 0.6377, 0.8525, P < 0.01) of high-density lipoprotein cholesterol (HDL) had a significantly lower risk of KSD in adjusted model 3. Results remained stable after stratified by age, gender, and body mass index (BMI) in subgroup analysis. No association was observed between low-density lipoprotein cholesterol (LDL), total cholesterol (TC) and triglycerides (TG) levels, and KSD.
Conclusions
Low HDL was associated with a higher risk of kidney stones in the USA adult population.


Similar content being viewed by others
Availability of data and materials
The datasets generated during the current study are available in the public database (NHANES) (https://www.cdc.gov/nchs/nhanes/).
References
Romero V, Akpinar H, Assimos DG (2010) Kidney stones: a global picture of prevalence, incidence, and associated risk factors. Rev Urol 12(2–3):e86-96
Abufaraj M, Xu T, Cao C, Waldhoer T, Seitz C, D’Andrea D, Siyam A, Tarawneh R, Fajkovic H, Schernhammer E, Yang L, Shariat SF (2021) Prevalence and Trends in Kidney Stone Among Adults in the USA: analyses of National Health and Nutrition Examination Survey 2007–2018 Data. Eur Urol Focus 7(6):1468–1475. https://doi.org/10.1016/j.euf.2020.08.011
Fink HA, Wilt TJ, Eidman KE, Garimella PS, MacDonald R, Rutks IR, Brasure M, Kane RL, Ouellette J, Monga M (2013) Medical management to prevent recurrent nephrolithiasis in adults: a systematic review for an American College of Physicians Clinical Guideline. Ann Intern Med 158(7):535–543. https://doi.org/10.7326/0003-4819-158-7-201304020-00005
Scales CD Jr, Smith AC, Hanley JM, Saigal CS, Urologic Diseases in America P (2012) Prevalence of kidney stones in the United States. Eur Urol 62(1):160–165. https://doi.org/10.1016/j.eururo.2012.03.052
Johri N, Cooper B, Robertson W, Choong S, Rickards D, Unwin R (2010) An update and practical guide to renal stone management. Nephron Clin Pract 116(3):c159-171. https://doi.org/10.1159/000317196
Kirkali Z, Rasooly R, Star RA, Rodgers GP (2015) Urinary stone disease: progress, status, and needs. Urology 86(4):651–653. https://doi.org/10.1016/j.urology.2015.07.006
Kopin L, Lowenstein C (2017) Dyslipidemia. Ann Intern Med 167(11):ITC81–ITC96. https://doi.org/10.7326/AITC201712050
Li J, Nie Z, Ge Z, Shi L, Gao B, Yang Y (2022) Prevalence of dyslipidemia, treatment rate and its control among patients with type 2 diabetes mellitus in Northwest China: a cross-sectional study. Lipids Health Dis 21(1):77. https://doi.org/10.1186/s12944-022-01691-1
Vekic J, Zeljkovic A, Stefanovic A, Jelic-Ivanovic Z, Spasojevic-Kalimanovska V (2019) Obesity and dyslipidemia. Metabolism 92:71–81. https://doi.org/10.1016/j.metabol.2018.11.005
Torricelli FC, De SK, Gebreselassie S, Li I, Sarkissian C, Monga M (2014) Dyslipidemia and kidney stone risk. J Urol 191(3):667–672. https://doi.org/10.1016/j.juro.2013.09.022
Cohen AJ, Adamsky MA, Nottingham CU, Pruitt J, Lapin B, Wang CH, Park S (2019) Impact of statin intake on kidney stone formation. Urology 124:57–61. https://doi.org/10.1016/j.urology.2018.01.029
Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults (1998). WMJ 97(9):20–21, 24–25, 27–37
Chen TC, Clark J, Riddles MK, Mohadjer LK, Fakhouri THI (2020) National Health and Nutrition Examination Survey, 2015–2018: sample design and estimation procedures. Vital Health Stat 2(184):1–35
Johnson CL, Paulose-Ram R, Ogden CL, Carroll MD, Kruszon-Moran D, Dohrmann SM, Curtin LR (2013) National health and nutrition examination survey: analytic guidelines, 1999–2010. Vital Health Stat 2(161):1–24
Emerging Risk Factors C, Di Angelantonio E, Sarwar N, Perry P, Kaptoge S, Ray KK, Thompson A, Wood AM, Lewington S, Sattar N, Packard CJ, Collins R, Thompson SG, Danesh J (2009) Major lipids, apolipoproteins, and risk of vascular disease. JAMA 302(18):1993–2000. https://doi.org/10.1001/jama.2009.1619
Kontush A (2014) HDL-mediated mechanisms of protection in cardiovascular disease. Cardiovasc Res 103(3):341–349. https://doi.org/10.1093/cvr/cvu147
Strazzella A, Ossoli A, Calabresi L (2021) High-density lipoproteins and the kidney. Cells. https://doi.org/10.3390/cells10040764
Smith LE (2020) High-density lipoproteins and acute kidney injury. Semin Nephrol 40(2):232–242. https://doi.org/10.1016/j.semnephrol.2020.01.013
Hung JA, Li CH, Geng JH, Wu DW, Chen SC (2022) Dyslipidemia increases the risk of incident kidney stone disease in a large Taiwanese population follow-up study. Nutrients. https://doi.org/10.3390/nu14071339
Kang HW, Lee SK, Kim WT, Kim YJ, Yun SJ, Lee SC, Kim WJ (2014) Hypertriglyceridemia and low high-density lipoprotein cholesterolemia are associated with increased hazard for urolithiasis. J Endourol 28(8):1001–1005. https://doi.org/10.1089/end.2014.0135
Ding Q, Ouyang J, Fan B, Cao C, Fan Z, Ding L, Li F, Tu W, Jin X, Wang J, Shi Y (2019) Association between dyslipidemia and nephrolithiasis risk in a Chinese population. Urol Int 103(2):156–165. https://doi.org/10.1159/000496208
Kirejczyk JK, Korzeniecka-Kozerska A, Baran M, Porowska H, Porowski T, Wasilewska A (2015) Dyslipidaemia in overweight children and adolescents is associated with an increased risk of kidney stones. Acta Paediatr 104(9):e407-413. https://doi.org/10.1111/apa.13079
Taguchi K, Okada A, Hamamoto S, Iwatsuki S, Naiki T, Ando R, Mizuno K, Tozawa K, Kohri K, Yasui T (2015) Proinflammatory and metabolic changes facilitate renal crystal deposition in an obese mouse model of metabolic syndrome. J Urol 194(6):1787–1796. https://doi.org/10.1016/j.juro.2015.07.083
Tsujihata M, Momohara C, Yoshioka I, Tsujimura A, Nonomura N, Okuyama A (2008) Atorvastatin inhibits renal crystal retention in a rat stone forming model. J Urol 180(5):2212–2217. https://doi.org/10.1016/j.juro.2008.07.024
Masterson JH, Woo JR, Chang DC, Chi T, L’Esperance JO, Stoller ML, Sur RL (2015) Dyslipidemia is associated with an increased risk of nephrolithiasis. Urolithiasis 43(1):49–53. https://doi.org/10.1007/s00240-014-0719-3
Speer T, Rohrer L, Blyszczuk P, Shroff R, Kuschnerus K, Krankel N, Kania G, Zewinger S, Akhmedov A, Shi Y, Martin T, Perisa D, Winnik S, Muller MF, Sester U, Wernicke G, Jung A, Gutteck U, Eriksson U, Geisel J, Deanfield J, von Eckardstein A, Luscher TF, Fliser D, Bahlmann FH, Landmesser U (2013) Abnormal high-density lipoprotein induces endothelial dysfunction via activation of Toll-like receptor-2. Immunity 38(4):754–768. https://doi.org/10.1016/j.immuni.2013.02.009
Taguchi K, Hamamoto S, Okada A, Unno R, Kamisawa H, Naiki T, Ando R, Mizuno K, Kawai N, Tozawa K, Kohri K, Yasui T (2017) Genome-wide gene expression profiling of Randall’s plaques in calcium oxalate stone formers. J Am Soc Nephrol 28(1):333–347. https://doi.org/10.1681/ASN.2015111271
Taguchi K, Chen L, Usawachintachit M, Hamamoto S, Kang M, Sugino T, Unno R, Tzou DT, Sherer BA, Okada A, Yasui T, Ho SP, Stoller ML, Chi T (2020) Fatty acid-binding protein 4 downregulation drives calcification in the development of kidney stone disease. Kidney Int 97(5):1042–1056. https://doi.org/10.1016/j.kint.2020.01.042
Aune D, Mahamat-Saleh Y, Norat T, Riboli E (2018) Body fatness, diabetes, physical activity and risk of kidney stones: a systematic review and meta-analysis of cohort studies. Eur J Epidemiol 33(11):1033–1047. https://doi.org/10.1007/s10654-018-0426-4
Lin BB, Huang RH, Lin BL, Hong YK, Lin ME, He XJ (2020) Associations between nephrolithiasis and diabetes mellitus, hypertension and gallstones: a meta-analysis of cohort studies. Nephrology (Carlton) 25(9):691–699. https://doi.org/10.1111/nep.13740
Yuan S, Larsson SC (2021) Assessing causal associations of obesity and diabetes with kidney stones using Mendelian randomization analysis. Mol Genet Metab 134(1–2):212–215. https://doi.org/10.1016/j.ymgme.2021.08.010
Funding
This work was supported by the National Natural Science Foundation of China (81770705 to Hequn Chen); Central South University Independent Exploration and Innovation Project for Graduate Students (2021zzts0348 to Zewu Zhu).
Author information
Authors and Affiliations
Contributions
MG: conceptualization, visualization, methodology, writing original draft. ZZ: validation, data curation, investigation. ML: methodology, software, formal analysis. ZZ and HC: conceptualization, project administration, supervision. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethics approval
Approval of the study from the National Center of Health and Statistics Research ethics review board was waived because the research relied on publicly used, de-identified secondary data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gao, M., Liu, M., Zhu, Z. et al. The association of dyslipidemia with kidney stone: result from the NHANES 2007–2020. Int Urol Nephrol 56, 35–44 (2024). https://doi.org/10.1007/s11255-023-03784-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03784-x