Abstract
Purpose
The development of roxadustat is a standard treatment for renal anemia, and multiple clinical trials have proved its safety and efficacy. However, less information is available from trials of the population with diabetic nephropathy (DN). This study aimed to determine whether roxadustat is effective for treating DN.
Methods
This was a single-center, retrospective, institutional review board-approved cohort study. The patients with DN were chosen and given roxadustat or erythropoietin (EPO) for 8 weeks. The mean hemoglobin (Hb) level after 8 weeks of treatment served as the primary outcome. Alterations in the iron index and lipid levels were considered secondary objectives. Sub-group analysis was performed to observe the impact of inflammation and glycemic status on Hb.
Results
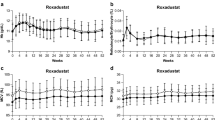
A total of 80 patients were enrolled, 40 in each group. After 8 weeks of treatment, the Hb levels in the roxadustat group were higher than those in the control group. The number of patients who achieved Hb response was higher in the roxadustat group than in the control group (77.5% versus 27.5%; P < 0.001). In addition to lowering total cholesterol and low-density lipoprotein cholesterol, roxadustat decreased ferritin and elevated total iron-binding capacity. Compared to the control group, roxadustat was more beneficial for patients with an inflammatory condition and poor glycemic control.
Conclusions
Roxadustat treatment remarkably corrected anemia in patients with DN, and its effectiveness was unaffected by inflammation or glycemic control levels. In addition, roxadustat can also reduce a patient's blood lipid level and enhance the body's use of iron.
Clinical trial registration
ChiCTR2200057232.


Similar content being viewed by others
References
Alicic RZ, Rooney MT, Tuttle KR (2017) Diabetic kidney disease: challenges, progress, and possibilities. Clin J Am Soc Nephrol 12(12):2032–2045
Pappa M, Dounousi E, Duni A, Katopodis K (2015) Less known pathophysiological mechanisms of anemia in patients with diabetic nephropathy. Int Urol Nephrol 47(8):1365–1372
Reutens AT (2013) Epidemiology of diabetic kidney disease. Med Clin North Am 97(1):1–18
Tuttle KR, Bakris GL, Bilous RW et al (2014) Diabetic kidney disease: a report from an ADA consensus conference. Diabetes Care 37:2864–2883 (Tuttle KR, Bakris GL, Bilous RW, et al., eds)
McFarlane SI, Salifu MO, Makaryus J, Sowers JR (2006) Anemia and cardiovascular disease in diabetic nephropathy. Curr Diab Rep 6:213–218 (McFarlane SI, Salifu MO, Makaryus J, Sowers JR, eds)
Loutradis C, Skodra A, Georgianos P et al (2016) Diabetes mellitus increases the prevalence of anemia in patients with chronic kidney disease: A nested case-control study. World J Nephrol. 5:358–366 (Loutradis C, Skodra A, Georgianos P, et al., eds)
Magwood JS, Lebby A, Chen B, Kessler S, Norris L, Bennett CL (2013) Emerging drugs for treatment of anemia of chronic kidney disease. Expert Opin Emerg Drugs 18(4):421–429
Solomon SD, Uno H, Lewis EF et al (2010) Erythropoietic response and outcomes in kidney disease and type 2 diabetes. N Engl J Med 363(12):1146–1155
Pfeffer MA, Burdmann EA, Chen CY et al (2009) A trial of darbepoetin alfa in type 2 diabetes and chronic kidney disease. N Engl J Med 361(21):2019–2032
Dhillon S (2019) Roxadustat: first global approval. Drugs 79(5):563–572
Chen N, Hao C, Liu BC et al (2019) Roxadustat treatment for anemia in patients undergoing long-term dialysis. N Engl J Med 381(11):1011–1022
Chen N, Hao C, Peng X et al (2019) Roxadustat for anemia in patients with kidney disease not receiving dialysis. N Engl J Med 381(11):1001–1010
Provenzano R, Shutov E, Eremeeva L et al (2021) Roxadustat for anemia in patients with end-stage renal disease incident to dialysis. Nephrol Dial Transplant 36(9):1717–1730
Fishbane S, El-Shahawy MA, Pecoits-Filho R et al (2021) Roxadustat for treating anemia in patients with CKD not on dialysis: results from a randomized phase 3 study. J Am Soc Nephrol 32(3):737–755
Zhu X, Jiang L, Wei X, Long M, Du Y (2022) Roxadustat: Not just for anemia. Front Pharmacol 13:971795
Voit RA, Sankaran VG (2020) Stabilizing HIF to ameliorate anemia. Cell 180(1):6
Rytkönen KT, Williams TA, Renshaw GM, Primmer CR, Nikinmaa M (2011) Molecular evolution of the metazoan PHD-HIF oxygen-sensing system. Mol Biol Evol 28(6):1913–1926
Maxwell PH, Eckardt KU (2016) HIF prolyl hydroxylase inhibitors for the treatment of renal anaemia and beyond. Nat Rev Nephrol 12(3):157–168
Zhang L, Liu Y, Huang Y et al (2022) Effect of roxadustat versus erythropoietin (EPO) for treating anemia in patients with diabetic kidney disease: a retrospective cohort study. Ann Transl Med 10(22):1224
Li Y, Shi H, Wang WM et al (2016) Prevalence, awareness, and treatment of anemia in Chinese patients with nondialysis chronic kidney disease: First multicenter, cross-sectional study. Medicine 95(24):e3872
Navarro-González JF, Mora-Fernández C, de Muros Fuentes M, García-Pérez J (2011) Inflammatory molecules and pathways in the pathogenesis of diabetic nephropathy. Nat Rev Nephrol 7(6):327–340
Hom J, Dulmovits BM, Mohandas N, Blanc L (2015) The erythroblastic island as an emerging paradigm in the anemia of inflammation. Immunol Res 63(1–3):75–89
Joksimovic Jovic J, Antic S, Nikolic T et al (2022) Erythropoietin resistance development in hemodialysis patients: the role of oxidative stress. Oxid Med Cell Longev 2022:9598211
Xiao ZZ, Huang Y, Mei W et al (2018) Associated factors of anemia in patients with diabetic nephropathy diagnosed by renal biopsy. China J Modern Med 28(29):79–86
Soliman AT, De Sanctis V, Yassin M, Soliman N (2017) Iron deficiency anemia and glucose metabolism. Acta Bio-med Atenei Parmensis 88(1):112–118
Huri HZ, Lim LP, Lim SK (2015) Glycemic control and antidiabetic drugs in type 2 diabetes mellitus patients with renal complications. Drug Des Dev Ther 9:4355–4371
Töyry JP, Niskanen LK, Mäntysaari MJ, Länsimies EA, Uusitupa MI (1996) Occurrence, predictors, and clinical significance of autonomic neuropathy in NIDDM ten-year follow-up from the diagnosis. Diabetes 45(3):308–315
Kratochvilová M, Zakiyanov O, Kalousová M, Kříha V, Zima T, Tesař V (2011) Associations of serum levels of advanced glycation end products with nutrition markers and anemia in patients with chronic kidney disease. Ren Fail 33(2):131–137
Liu JL, Zhang JG (2016) Effect of blood glucose control level on serum ferritin, islet alpha and beta cell function in patients with diabetes mellitus and atherosclerosis. Chin J Diabetes. 24:820–825 (in Chinese)
Jiang F, Sun ZZ, Tang YT, Xu C, Jiao XY (2011) Hepcidin expression and iron parameters change in Type 2 diabetic patients. Diabetes Res Clin Pract 93:43–48 (Jiang F, Sun ZZ, Tang YT, Xu C, Jiao XY, eds.)
Dev S, Babitt JL (2017) Overview of iron metabolism in health and disease. Hemodial Int 21(Suppl 1):6–20 (Dev S, Babitt JL, eds)
Li YK, Zhang MX (2012) Study on the relationship between urine albumin excretion and iron metabolism biomarkers in patients with type 2 diabetes mellitus. J Clin Intern Med 29(5):324–326
Feng M, Xu CB, Wen JP, Lv Q, Yang XL (2018) Correlation between serum iron metabolism and diabetic nephropathy in elderly patients with type 2 diabetes mellitus. Chin J Gerontol 38(3):547–549
Coyne DW, Roger SD, Shin SK et al (2021) Roxadustat for CKD-related anemia in non-dialysis patients. Kidney Int Rep 6(3):624–635
Hou YP, Mao XY, Wang C et al (2022) Roxadustat treatment for anemia in peritoneal dialysis patients: a randomized controlled trial. J Formosan Med Assoc. 121(2):529–538
Hwang S, Nguyen AD, Jo Y, Engelking LJ, Brugarolas J, DeBose-Boyd RA (2017) Hypoxia-inducible factor 1α activates insulin-induced gene 2 (Insig-2) transcription for degradation of 3-hydroxy-3-methylglutaryl (HMG)-CoA reductase in the liver. J Biol Chem 292(22):9382–9393
Kim JW, Tchernyshyov I, Semenza GL, Dang CV (2006) HIF-1-mediated expression of pyruvate dehydrogenase kinase: a metabolic switch required for cellular adaptation to hypoxia. Cell Metab 3(3):177–185
Shen GM, Zhao YZ, Chen MT et al (2012) Hypoxia-inducible factor-1 (HIF-1) promotes LDL and VLDL uptake through inducing VLDLR under hypoxia. Biochem J 441(2):675–683
Funding
This work (research, review, or writing) required no funding of any type from any agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jiang, L., Jia, R., Zheng, Z. et al. A clinical study on roxadustat for anemia in diabetic nephropathy: a 8-week study. Int Urol Nephrol 56, 1093–1101 (2024). https://doi.org/10.1007/s11255-023-03757-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03757-0