Abstract
Purpose
Several clinical scenarios regulate the final ejaculated semen, which is pivotal to reproductive success. Sperm motility and plasma membrane fusogenic activity primarily rely on the peculiar sperm lipid composition, influenced by the patient’s metabolism, genetics, nutritional, environmental status, and concomitant clinical entities such as varicocele. This study aimed to determine the relationship between serum lipid profile and testicular function (semen quality and testosterone levels).
Methods
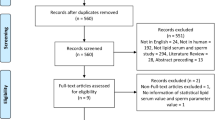
This retrospective study uses medical charts of 278 infertile men who attended andrological care between 2000 and 2019. Seminal analysis data, lipid profile, and total serum testosterone were collected. A multiple linear regression analysis was performed to evaluate the influence of the lipid parameters on the seminal variables. Statistical analyses were carried out with p ≤ 0.05 considered statistically significant.
Results
Seminal creatine kinase activity (p = 0.024) is negatively related to HDL (p = 0.032) and triglycerides (p = 0.037), while total testosterone (p < 0.0001) and seminal volume (p = 0.046) appeared both to be negatively related to triglycerides (p = 0.030 and p = 0.033, respectively).
Conclusion
Medical advice commonly advocated to prevent endothelial dysfunction and cardiovascular disease and improve HDL-cholesterol and triglyceride levels in dyslipidemic patients should also be given to infertile men. Physicians should give patients a thorough assessment, including the blood lipid profile, hormonal status, and routine seminal examinations. We propose a more comprehensive men´s health check-up for the infertile male population, not limited to a simple evaluation of basic sperm parameters.
Similar content being viewed by others
References
World Health O (2010) Laboratory manual for the examination and processing of human semen, 5th edn. World Health Organization, Geneva
Barazani Y, Katz BF, Nagler HM, Stember DS (2014) Lifestyle, environment, and male reproductive health. Urol Clin North Am 41(1):55–66. https://doi.org/10.1016/j.ucl.2013.08.017
Smith JF, Walsh TJ, Shindel AW et al (2009) Sexual, marital, and social impact of a man’s perceived infertility diagnosis. J Sex Med 6(9):2505–2515. https://doi.org/10.1111/j.1743-6109.2009.01383.x
Agarwal A, Mulgund A, Hamada A, Chyatte MR (2015) A unique view on male infertility around the globe. Reprod Biol Endocrinol 13:9–37. https://doi.org/10.1186/s12958-015-0032-1
Belladelli F, Boeri L, Pozzi E et al (2022) Triglycerides/glucose index is associated with sperm parameters and sperm DNA fragmentation in primary infertile men: a cross-sectional study. Metabolites 12(2):11. https://doi.org/10.3390/metabo12020143
Lu JC, Jing J, Yao Q et al (2016) Relationship between lipids levels of serum and seminal plasma and semen parameters in 631 Chinese subfertile men. PLoS One 11(1):13. https://doi.org/10.1371/journal.pone.0146304
Ergun A, Kose SK, Aydos K, Ata A, Avci A (2007) Correlation of seminal parameters with serum lipid profile and sex hormones. Arch Androl 53(1):21–23. https://doi.org/10.1080/01485010600888961
Schisterman EF, Mumford SL, Chen Z et al (2014) Lipid concentrations and semen quality: the LIFE study. Andrology 2(3):408–415. https://doi.org/10.1111/j.2047-2927.2014.00198.x
Ouvrier A, Alves G, Damon-Soubeyrand C et al (2011) Dietary cholesterol-induced post-testicular infertility. PLoS One 6(11):13. https://doi.org/10.1371/journal.pone.0026966
Whitfield M, Pollet-Villard X, Levy R, Drevet JR, Saez F (2015) Posttesticular sperm maturation, infertility, and hypercholesterolemia. Asian J Androl 17(5):742–748. https://doi.org/10.4103/1008-682x.155536
Fraietta R, Zylberstejn DS, Esteves SC (2013) Hypogonadotropic hypogonadism revisited. Clinics 68:81–88. https://doi.org/10.6061/clinics/2013(Sup01)09
Ciccone IM, Costa EM, Pariz JR et al (2021) Serum vitamin D content is associated with semen parameters and serum testosterone levels in men. Asian J Androl 23(1):52. https://doi.org/10.4103/aja.aja_9_20
Zhang N, Zhang HQ, Zhang X et al (2014) The relationship between endogenous testosterone and lipid profile in middle-aged and elderly Chinese men. Eur J Endocrinol 170(4):487–494. https://doi.org/10.1530/eje-13-0802
Makinen JI, Perheentupa A, Irjala K et al (2007) Endogenous testosterone and serum lipids in middle-aged men. Atherosclerosis 197(2):688–693. https://doi.org/10.1016/j.atherosclerosis.2007.05.009
Simon D, Charles MA, Nahoul K et al (1997) Association between plasma total testosterone and cardiovascular risk factors in healthy adult men: the telecom study. J Clin Endocrinol Metab 82(2):682–685. https://doi.org/10.1210/jc.82.2.682
Agledahl I, Skjaerpe PA, Hansen JB, Svartberg J (2008) Low serum testosterone in men is inversely associated with non-fasting serum triglycerides: the Tromso study. Nutr Metab Cardiovasc Dis 18(4):256–262. https://doi.org/10.1016/j.numecd.2007.01.014
Akishita M, Fukai S, Hashimoto M et al (2010) Association of low testosterone with metabolic syndrome and its components in middle-aged Japanese men. Hypertens Res 33(6):587–591. https://doi.org/10.1038/hr.2010.43
Haring R, Baumeister SE, Volzke H et al (2011) Prospective association of low total testosterone concentrations with an adverse lipid profile and increased incident dyslipidemia. Eur J Cardiovasc Prev Rehabil 18(1):86–96. https://doi.org/10.1097/HJR.0b013e32833c1a8d
Hagiuda J, Ishikawa H, Furuuchi T, Hanawa Y, Marumo K (2014) Relationship between dyslipidaemia and semen quality and serum sex hormone levels: an infertility study of 167 Japanese patients. Andrologia 46(2):131–135. https://doi.org/10.1111/and.12057
Hallak J, Sharma RK, Pasqualotto FF, Ranganathan P, Thomas AJ, Agarwal A (2001) Creatine kinase as an indicator of sperm quality and maturity in men with oligospermia. Urology 58(3):446–451. https://doi.org/10.1016/s0090-4295(01)01224-9
Vargas-Vazquez A, Bello-Chavolla OY, Antonio-Villa NE, Mehta R, Cruz-Bautista I, Aguilar-Salinas CA (2021) Comparative assessment of LDL-C and VLDL-C estimation in familial combined hyperlipidemia using Sampson’s, Martin’ and Friedewald’s equations. Lipids Health Dis 20(1):9–46. https://doi.org/10.1186/s12944-021-01471-3
Salonia A, Matloob R, Gallina A et al (2009) Are infertile men less healthy than fertile men? Results of a prospective case-control survey. Eur Urol 56(6):1025–1031. https://doi.org/10.1016/j.eururo.2009.03.001
Hallak J, Teixeira TA, Barrozo LV, Singer J, Kallas EG, Saldiva PHN (2022) Male sex rather than socioeconomic vulnerability as a determinant for COVID-19 death in Sao Paulo: a population-based study. Sage Open Med 10:9. https://doi.org/10.1177/20503121221105583
Hallak J, Teixeira TA, Bernardes FS et al (2021) SARS-CoV-2 and its relationship with the genitourinary tract: implications for male reproductive health in the context of COVID-19 pandemic. Andrology 9(1):73–79. https://doi.org/10.1111/andr.12896
Lotti F, Marchiani S, Corona G, Maggi M (2021) Metabolic syndrome and reproduction. Int J Mol Sci 22(4):26. https://doi.org/10.3390/ijms22041988
Maresch CC, Stute DC, Alves MG, Oliveira PF, de Kretser DM, Linn T (2018) Diabetes-induced hyperglycemia impairs male reproductive function: a systematic review. Hum Reprod Update 24(1):86–105. https://doi.org/10.1093/humupd/dmx033
Cabler S, Agarwal A, Flint M, Du Plessis SS (2010) Obesity: modern man’s fertility nemesis. Asian J Androl 12(4):480–489. https://doi.org/10.1038/aja.2010.38
Maleki BH, Tartibian B, Chehrazi M (2017) The effects of three different exercise modalities on markers of male reproduction in healthy subjects: a randomized controlled trial. Reproduction 153(2):157–174. https://doi.org/10.1530/rep-16-0318
Karolczak K, Watala C (2019) The mystery behind the pineal gland: melatonin affects the metabolism of cholesterol. Oxid Med Cell Longev 2019:8. https://doi.org/10.1155/2019/4531865
Yoo JE, Han K, Shin DW et al (2022) Association between changes in alcohol consumption and cancer risk. JAMA Netw Open 5(8):14. https://doi.org/10.1001/jamanetworkopen.2022.28544
de Souza GL, Hallak J (2011) Anabolic steroids and male infertility: a comprehensive review. BJU Int 108(11):1860–1865. https://doi.org/10.1111/j.1464-410X.2011.10131.x
Teixeira TA, Iori I, Andrade G et al (2022) Marijuana Is associated with a hormonal imbalance among several habits related to male infertility: a retrospective study. Front Reprod Health 2022:4. https://doi.org/10.3389/frph.2022.820451
Skakkebæk NE, Lindahl-Jacobsen R, Levine H et al (2022) Environmental factors in declining human fertility. Nat Rev Endocrinol 18(3):139–157. https://doi.org/10.1038/s41574-021-00598-8
Carrasco CHL, Noda P, Barbosa AP et al (2022) SARS-CoV-2 nucleocapsid protein is associated with lower testosterone levels: an experimental study. Front Physiol 13:8. https://doi.org/10.3389/fphys.2022.867444
Teixeira TA, Bernardes FS, Oliveira YC et al (2021) SARS-CoV-2 and multi-organ damage - what men’s health specialists should know about the COVID-19 pathophysiology. Int Braz J Urol 47(3):637–646. https://doi.org/10.1590/s1677-5538.ibju.2020.0872
Bataineh HN, Nusier MK (2005) Effect of cholesterol diet on reproductive function in male albino rats. Saudi Med J 26(3):398–404
Chung TH, Kwon YJ, Lee YJ (2020) High triglyceride to HDL cholesterol ratio is associated with low testosterone and sex hormone-binding globulin levels in middle-aged and elderly men. Aging Male 23(2):93–97. https://doi.org/10.1080/13685538.2018.1501015
Grosman H, Rosales M, Fabre B et al (2014) Association between testosterone levels and the metabolic syndrome in adult men. Aging Male 17(3):161–165. https://doi.org/10.3109/13685538.2014.913561
Hallak J (2017) A call for more responsible use of Assisted Reproductive Technologies (ARTs) in male infertility: the hidden consequences of abuse, lack of andrological investigation and inaction. Transl Androl Urol 6(5):997–1004. https://doi.org/10.21037/tau.2017.08.03
Acknowledgements
The authors would like to thank Androscience, Science and Innovation Center in Andrology and High-Complex Clinical and Andrology Laboratory, for providing laboratorial support, and the Androscience Institute (IA) for technical support.
Funding
This work was supported by the Fundação de Amparo à Pesquisa do Estado de São Paulo, under Grant No. 2019/11179-8.
Author information
Authors and Affiliations
Contributions
Conceptualization: JH, TAT, and EMC. Data curation: GA, II, MKH, and GM. Formal analysis: GA, TAT, EMC, and JH. Funding acquisition: PCEZ, JRD, and JH. Investigation: GA, II, MKH, GM, and PCEZ. Methodology: TAT, EMC, JRD, and JH. Project administration: TAT, EMC, and JH. Resources: PCEZ. Software: PCEZ. Supervision: EMC, JRD, and JH. Validation: TAT and PCEZ. Visualization: GA, II, MKH, and GM. Writing—original draft: GA, II, MKH, and GM. Writing—review and editing: PCEZ, TAT, JRD, EMC, and JH.
Corresponding author
Ethics declarations
Conflict of interest
Authors declare that no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Andrade, G., Iori, I., Hsieh, M.K. et al. Serum lipid profile levels and semen quality: new insights and clinical perspectives for male infertility and men’s health. Int Urol Nephrol 55, 2397–2404 (2023). https://doi.org/10.1007/s11255-023-03688-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03688-w