Abstract
Objective
To investigate the risk factors of acute kidney injury (AKI) patients with acute myocardial infarction (AMI) and establish potential microRNA (miRNA) biomarkers in the peripheral blood of AMI–AKI patients.
Methods
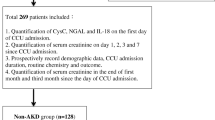
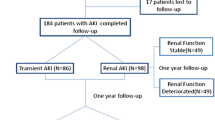
Patients hospitalized from 2016 to 2020 and diagnosed with AMI (with AKI or without AKI groups) were recruited. The data of the two groups were compared and the risk factors of AMI–AKI were analyzed by logistic regression. The receiver operator characteristics (ROC) curve was drawn and the predictive value of risk factors in AMI–AKI was evaluated. Six AMI–AKI patients were selected and six healthy subjects were enrolled as the control. The peripheral blood samples of the two groups were collected for miRNA high-throughput sequencing.
Results
A total of 300 AMI patients were collected, including 190 patients with AKI and 110 patients without AKI. Multivariate logistic regression analysis indicated that diastolic pressure (68–80 mmHg), urea nitrogen, creatinine, serum uric acid (SUA), aspartate aminotransferase (AST), and left ventricular ejection fraction were the dependent risk factors of AMI–AKI patients (P < 0.05). ROC curve showed that the incidence of AMI–AKI patients was most correlated with urea nitrogen, creatinine, and SUA. In addition, 60 differentially expressed miRNAs were identified between AMI–AKI and controls. Then, hsa-miR-2278, hsa-miR-1827, and hsa-miR-149-5p were more corrected with predictors. Twelve of them targeted 71 genes involved in phagosome, oxytocin signaling pathway, and microRNAs in cancer pathways.
Conclusion
Urea nitrogen, creatinine, and SUA were the dependent risk factors and important predictors for AMI–AKI patients. Three miRNAs may be considered as biomarkers for AMI–AKI.




Similar content being viewed by others
Data availability
The datasets generated during and analyzed during the current study are publicly available. We have published the relevant data on Genome sequence archive (https://ngdc.cncb.ac.cn/gsa/).
References
Bruetto RG, Rodrigues FB, Torres US, Otaviano AP, Zanetta DM, Burdmann EA (2012) Renal function at hospital admission and mortality due to acute kidney injury after myocardial infarction. PLoS One 7(4):e35496
Rodrigues FB, Bruetto RG, Torres US, Otaviano AP, Zanetta DM, Burdmann EA (2013) Incidence and mortality of acute kidney injury after myocardial infarction: a comparison between KDIGO and RIFLE criteria. PLoS One 8(7):e69998
Zahler D, Rozenfeld KL, Merdler I, Itach T, Morgan S, Levit D et al (2022) Relation between serum creatine phosphokinase levels and acute kidney injury among ST-segment elevation myocardial infarction patients. J Clin Med. https://doi.org/10.3390/jcm11041137
Shacham Y, Leshem-Rubinow E, Steinvil A, Assa EB, Keren G, Roth A et al (2014) Renal impairment according to acute kidney injury network criteria among ST elevation myocardial infarction patients undergoing primary percutaneous intervention: a retrospective observational study. Clin Res Cardiol 103(7):525–532
Tsai TT, Patel UD, Chang TI, Kennedy KF, Masoudi FA, Matheny ME et al (2014) Contemporary incidence, predictors, and outcomes of acute kidney injury in patients undergoing percutaneous coronary interventions: insights from the NCDR Cath-PCI registry. JACC Cardiovasc Interv 7(1):1–9
Wald R, McArthur E, Adhikari NK, Bagshaw SM, Burns KE, Garg AX et al (2015) Changing incidence and outcomes following dialysis-requiring acute kidney injury among critically ill adults: a population-based cohort study. Am J Kidney Dis 65(6):870–877
Ledeganck KJ, Gielis EM, Abramowicz D, Stenvinkel P, Shiels PG, Van Craenenbroeck AH (2019) MicroRNAs in AKI and Kidney transplantation. Clin J Am Soc Nephrol 14(3):454–468
Hodgkinson CP, Kang MH, Dal-Pra S, Mirotsou M, Dzau VJ (2015) MicroRNAs and cardiac regeneration. Circ Res 116(10):1700–1711
Jones TF, Bekele S, O’Dwyer MJ, Prowle JR (2018) MicroRNAs in acute kidney injury. Nephron 140(2):124–128
Guo C, Dong G, Liang X, Dong Z (2019) Epigenetic regulation in AKI and kidney repair: mechanisms and therapeutic implications. Nat Rev Nephrol 15(4):220–239
Sun T, Dong YH, Du W, Shi CY, Wang K, Tariq MA et al (2017) The role of microRNAs in myocardial infarction: from molecular mechanism to clinical application. Int J Mol Sci. 18(4):745
Liu Y, Feng DJ, Wang LF, Liu LH, Ren ZH, Hao JY et al (2022) The impact of cardiac dysfunction based on killip classification on gastrointestinal bleeding in acute myocardial infarction. Front Med (Lausanne) 9:865663
Wiersema R, Jukarainen S, Eck RJ, Kaufmann T, Koeze J, Keus F et al (2020) Different applications of the KDIGO criteria for AKI lead to different incidences in critically ill patients: a post hoc analysis from the prospective observational SICS-II study. Crit Care 24(1):164
Ugwuowo U, Yamamoto Y, Arora T, Saran I, Partridge C, Biswas A et al (2020) Real-time prediction of acute kidney injury in hospitalized adults: implementation and proof of concept. Am J Kidney Dis 76(6):806–14 e1
Ejaz AA, Beaver TM, Shimada M, Sood P, Lingegowda V, Schold JD et al (2009) Uric acid: a novel risk factor for acute kidney injury in high-risk cardiac surgery patients? Am J Nephrol 30(5):425–429
Lapsia V, Johnson RJ, Dass B, Shimada M, Kambhampati G, Ejaz NI et al (2012) Elevated uric acid increases the risk for acute kidney injury. Am J Med 125(3):302 e9–17
Gaipov A, Solak Y, Turkmen K, Toker A, Baysal AN, Cicekler H et al (2015) Serum uric acid may predict development of progressive acute kidney injury after open heart surgery. Ren Fail 37(1):96–102
Otomo K, Horino T, Miki T, Kataoka H, Hatakeyama Y, Matsumoto T et al (2016) Serum uric acid level as a risk factor for acute kidney injury in hospitalized patients: a retrospective database analysis using the integrated medical information system at Kochi Medical School hospital. Clin Exp Nephrol 20(2):235–243
Grivei A, Giuliani KTK, Wang X, Ungerer J, Francis L, Hepburn K et al (2020) Oxidative stress and inflammasome activation in human rhabdomyolysis-induced acute kidney injury. Free Radic Biol Med 160:690–695
Shimada M, Dass B, Ejaz AA (2011) Paradigm shift in the role of uric acid in acute kidney injury. Semin Nephrol 31(5):453–458
Ejaz AA, Dass B, Lingegowda V, Shimada M, Beaver TM, Ejaz NI et al (2013) Effect of uric acid lowering therapy on the prevention of acute kidney injury in cardiovascular surgery. Int Urol Nephrol 45(2):449–458
Wilson M, Packington R, Sewell H, Bartle R, McCole E, Kurth MJ et al (2022) Biomarkers during recovery from AKI and prediction of long-term reductions in estimated GFR. Am J Kidney Dis 79(5):646–56 e1
Shao M, Wang S, Parameswaran PK (2017) Hypoalbuminemia: a risk factor for acute kidney injury development and progression to chronic kidney disease in critically ill patients. Int Urol Nephrol 49(2):295–302
Lee EH, Kim HR, Baek SH, Kim KM, Chin JH, Choi DK et al (2014) Risk factors of postoperative acute kidney injury in patients undergoing esophageal cancer surgery. J Cardiothorac Vasc Anesth 28(4):936–942
Kim CS, Oak CY, Kim HY, Kang YU, Choi JS, Bae EH et al (2013) Incidence, predictive factors, and clinical outcomes of acute kidney injury after gastric surgery for gastric cancer. PLoS One 8(12):e82289
Sang BH, Bang JY, Song JG, Hwang GS (2015) Hypoalbuminemia within two postoperative days is an independent risk factor for acute kidney injury following living donor liver transplantation: a propensity score analysis of 998 consecutive patients. Crit Care Med 43(12):2552–2561
He H, Cai M, Zhu J, Xiao W, Liu B, Shi Y et al (2018) miR-148a-3p promotes rabbit preadipocyte differentiation by targeting PTEN. In Vitro Cell Dev Biol Anim 54(3):241–249
Zhai C, Li R, Hou K, Chen J, Alzogool M, Hu Y et al (2020) Value of blood-based microRNAs in the diagnosis of acute myocardial infarction: a systematic review and meta-analysis. Front Physiol 11:691
Shihana F, Wong WKM, Joglekar MV, Mohamed F, Gawarammana IB, Isbister GK et al (2021) Urinary microRNAs as non-invasive biomarkers for toxic acute kidney injury in humans. Sci Rep 11(1):9165
Nolte E, Wach S, Silva IT, Lukat S, Ekici AB, Munkert J et al (2017) A new semisynthetic cardenolide analog 3beta-[2-(1-amantadine)- 1-on-ethylamine]-digitoxigenin (AMANTADIG) affects G2/M cell cycle arrest and miRNA expression profiles and enhances proapoptotic survivin-2B expression in renal cell carcinoma cell lines. Oncotarget 8(7):11676–11691
Wang K, Hu YB, Zhao Y, Ye C (2021) Long noncoding RNA ASAP1IT1 suppresses ovarian cancer progression by regulating Hippo/YAP signaling. Int J Mol Med. https://doi.org/10.3892/ijmm.2021.4877
Zhu S, Peng W, Li X, Weng J, Zhang X, Guo J et al (2017) miR-1827 inhibits osteogenic differentiation by targeting IGF1 in MSMSCs. Sci Rep 7:46136
Zhou Z, Zheng X, Mei X, Li W, Qi S, Deng Y et al (2021) Hsa_circ_0080229 upregulates the expression of murine double minute-2 (MDM2) and promotes glioma tumorigenesis and invasion via the miR-1827 sponging mechanism. Ann Transl Med 9(9):762
Wang J, Yang K, Cao J, Li L (2021) Knockdown of circular RNA septin 9 inhibits the malignant progression of breast cancer by reducing the expression of solute carrier family 1 member 5 in a microRNA-149-5p-dependent manner. Bioengineered 12(2):10624–10637
Liu G, Yin L, Ouyang X, Zeng K, Xiao Y, Li Y (2020) M2 macrophages promote HCC cells invasion and migration via miR-149-5p/MMP9 signaling. J Cancer 11(5):1277–1287
Ruan D, Liu Y, Wang X, Yang D, Sun Y (2019) miR-149-5p protects against high glucose-induced pancreatic beta cell apoptosis via targeting the BH3-only protein BIM. Exp Mol Pathol 110:104279
Chen F, Chen H, Jia Y, Lu H, Tan Q, Zhou X (2020) miR-149-5p inhibition reduces Alzheimer’s disease beta-amyloid generation in 293/APPsw cells by upregulating H4K16ac via KAT8. Exp Ther Med 20(5):88
Breyer F, Hartlova A, Thurston T, Flynn HR, Chakravarty P, Janzen J et al (2021) TPL-2 kinase induces phagosome acidification to promote macrophage killing of bacteria. EMBO J 40(10):e106188
Ding C, Leow MK, Magkos F (2019) Oxytocin in metabolic homeostasis: implications for obesity and diabetes management. Obes Rev 20(1):22–40
Elnagar A, El-Dawy K, El-Belbasi HI, Rehan IF, Embark H, Al-Amgad Z et al (2022) Ameliorative effect of oxytocin on FBN1 and PEPCK gene expression, and behavioral patterns in rats’ obesity-induced diabetes. Front Public Health 10:777129
Phie J, Haleagrahara N, Newton P, Constantinoiu C, Sarnyai Z, Chilton L et al (2015) Prolonged subcutaneous administration of oxytocin accelerates angiotensin II-induced hypertension and renal damage in male rats. PLoS One 10(9):e0138048
Acknowledgements
We would like to give our sincere appreciation to the reviewers for their helpful comments on this article.
Funding
This study is funded by the National Natural Science Foundation of China (81860125) and the Youth fund of Natural Science Foundation of Xinjiang Uygur Autonomous Region (2017D01C342).
Author information
Authors and Affiliations
Contributions
XH performed molecular experiments and wrote this manuscript. MM prepared the samples and collected clinical information. MT performed statistical analyses. SL reviewed and edited the manuscripts. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the study was conducted without any commercial or financial relationship and can be understood as free of any potential conflict of interest.
Ethical approval and consent to participate
The specimens used in this study were approved by the ethics committee of the First Affiliated Hospital of Xinjiang Medical University (approval number: K202003-01) and all experiments were performed with informed consent.
Consent for publication
All authors approved the final manuscript and the submission to this journal.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huang, X., Mulasihan, M., Tudi, M. et al. A single-center clinical study of acute kidney injury associated with acute myocardial infarction. Int Urol Nephrol 56, 325–334 (2024). https://doi.org/10.1007/s11255-023-03676-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03676-0