Abstract
Purpose
To investigate the prevalence of microalbuminuria and factors associated with microalbuminuria in Graves’ Disease (GD).
Methods
This cross-sectional and single-center study included 99 patients with GD and 47 healthy controls (HC). Exclusion criteria such as active infection, uncontrolled diabetes, and chronic kidney disease were applied to the participants. The participants’ clinical findings, comorbidities, drug use, laboratory tests, and thyroid antibody levels were recorded. Spot urine samples were collected and stored at – 80 ℃ to analyze the presence of microalbuminuria.
Results
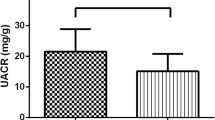
The prevalence of microalbuminuria in patients with GD was 12.1%. The median microalbumin/creatinine ratio in spot urine (UACR) in patients with GD (9.49 mg/g [5.09–18.10]) was higher than in the HC group (7.99 mg/g [3.48–12.88], p = 0.033). UACR was correlated with thyroid-stimulating hormone receptor antibody (TRAb), thyroid-stimulating hormone (TSH), and free triiodothyronine (FT3) levels (p = 0.020, p = 0.006, p = 0.009 respectively). In the regression analysis, only the relationship between TRAb level and UACR remained (p = 0.040).
Conclusion
This study demonstrates an increased prevalence of microalbuminuria in patients with GD. There was a significant correlation between microalbuminuria and TRAb level in patients with GD. This relationship suggests that one of the underlying mechanisms of microalbuminuria seen in patients with GD may be autoimmunity.


Similar content being viewed by others
Data Availability
The data used and analyzed during the current scoping review are available from the corresponding author upon reasonable request.
References
Tomer Y, Huber A (2009) The etiology of autoimmune thyroid disease: a story of genes and environment. J Autoimmun 32(3–4):231–239
Ross DS, Burch HB, Cooper DS, Greenlee MC, Laurberg P et al (2016) 2016 American thyroid association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid 26(10):1343–1421
Kahaly GJ (2020) Management of graves thyroidal and extrathyroidal disease: an update. J Clin Endocrinol Metab 105(12):3704–3720
Iglesias P, Bajo MA, Selgas R, Díez JJ (2017) Thyroid dysfunction and kidney disease: an update. Rev Endocr Metab Disord 18(1):131–144
Santoro D, Vadalà C, Siligato R, Buemi M, Benvenga S (2017) Autoimmune thyroiditis and glomerulopathies. Front Endocrinol 2(8):119
Halimi JM, Hadjadj S, Aboyans V, Allaert FA, Artigou JY et al (2007) Microalbuminuria and urinary albumin excretion: clinical practice guidelines. Nephrol Ther 3(6):384–391 ((In French))
Ruggenenti P, Gaspari F, Perna A, Remuzzi G (1998) Cross-sectional longitudinal study of spot morning urine protein: creatinine ratio, 24-hour urine protein excretion rate, glomerular filtration rate, and end-stage renal failure in chronic renal disease in patients without diabetes. BMJ 316(7130):504–509
Busby DE, Bakris GL (2004) Comparison of commonly used assays for the detection of microalbuminuria. J Clin Hypertens 6(11Suppl3):8–12
Xie J, Wang X, Zhang Y, Li H, Xu Y et al (2019) The longitudinal effect of subclinical hypothyroidism on urine microalbumin-to-urine creatinine ratio in patients with type 2 diabetes mellitus. BMC Endocr Disord 19(1):84
Metcalf PA, Scragg RK (1994) Epidemiology of microalbuminuria in the general population. J Diabetes Complicat 8(3):157–163
Jones CA, Francis ME, Eberhardt MS, Chavers B, Coresh J et al (2002) Microalbuminuria in the US population: third National Health and Nutrition Examination Survey. Am J Kidney Dis 39(3):445–459
Liese AD, Hense HW, Döring A, Stieber J, Keil U (2001) Microalbuminuria, central adiposity, and hypertension in the non-diabetic urban population of the MONICA Augsburg survey 1994/95. J Hum Hypertens 15(11):799–804
Weetman AP, Tomlinson K, Amos N, Lazarus JH, Hall R et al (1985) Proteinuria in autoimmune thyroid disease. Acta Endocrinol 109(3):341–347
Sellitti DF, Akamizu T, Doi SQ, Kim GH, Kariyil JT et al (2000) Renal expression of two “thyroid-specific” genes: thyrotropin receptor and thyroglobulin. Exp Nephrol 8(4–5):235–243
Davies TF, Ando T, Lin RY, Tomer Y, Latif R (2005) Thyrotropin receptor-associated diseases: from adenomata to Graves disease. J Clin Invest 115(8):1972–1983
Agarwal S, Koh KH, Tardi NJ, Chen C, Dande RR et al (2021) Deiodinase-3 is a thyrostat to regulate podocyte homeostasis. EBioMedicine 72:103617. https://doi.org/10.1016/j.ebiom.2021.103617
Chaker L, Sedaghat S, Hoorn EJ, Elzen WP, Gussekloo J et al (2016) The association of thyroid function and the risk of kidney function decline: a population-based cohort study. Eur J Endocrinol 175(6):653–660
Schultheiss UT, Daya N, Grams ME, Seufert J, Steffes M et al (2017) Thyroid function, reduced kidney function and incident chronic kidney disease in a community-based population: the atherosclerosis risk in communities study. Nephrol Dial Transplant 32(11):1874–1881
Lo JC, Chertow GM, Go AS, Hsu CY (2005) Increased prevalence of subclinical and clinical hypothyroidism in persons with chronic kidney disease. Kidney Int 67(3):1047–1052
Meuwese CL, Gussekloo J, de Craen AJ, Dekker FW, den Elzen WP (2014) Thyroid status and renal function in older persons in the general population. J Clin Endocrinol Metab 99(8):2689–2696
Zhang Y, Chang Y, Ryu S, Cho J, Lee WY et al (2014) Thyroid hormone levels and incident chronic kidney disease in euthyroid individuals: the Kangbuk Samsung Health Study. Int J Epidemiol 43(5):1624–1632
Wu J, Li X, Tao Y, Wang Y, Peng Y (2015) Free triiodothyronine levels are associated with diabetic nephropathy in euthyroid patients with type 2 diabetes. Int J Endocrinol. https://doi.org/10.1155/2015/204893
Gilles R, den Heijer M, Ross AH, Sweep FC, Hermus AR et al (2008) Thyroid function in patients with proteinuria. Neth J Med 66(11):483–485
Chavan VU, Durgawale PP, Sayyed AK, Sontakke AV, Attar NR et al (2011) A comparative study of clinical utility of spot urine samples with 24-h urine albumin excretion for screening of microalbuminuria in type 2 diabetic patients. Indian J Clin Biochem 26(3):283–289
Author information
Authors and Affiliations
Contributions
All authors provided substantial contributions to the design and implementation of this study and the generation of the manuscript. The contributions of each author are as follows: MSG, HMO, NS, and DK conceived the design and purpose of the work. OAA and GZ: took part in the collection of data and spot urine samples. AND, ZK, ED, CS, and CK: analyzed the data AND: interpreted the results based on the available literature and drafted the manuscript. MSG, HMÖ, and AND: made critical revisions. MSG, HMÖ, and AND: provided the final version of the article.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any potential conflicts of interest associated with this research.
Ethical approval
The study adhered to the ethical principles for medical research involving human participants described in the World Medical Association's Declaration of Helsinki. Istanbul University-Cerrahpaşa Ethics Committee approved the study (Approval Number: 2019-09-83045809-604.01.02).
Informed consent
Signed informed consent was obtained from all study participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Demir, A.N., Kara, Z., Durcan, E. et al. Do not forget the kidney in graves’ disease. Int Urol Nephrol 55, 2667–2673 (2023). https://doi.org/10.1007/s11255-023-03600-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03600-6