Abstract
Background
Although methicillin-resistant Staphylococcus aureus (MRSA) nasal colonization is common among end-stage kidney disease patients undergoing haemodialysis, few studies were focused on MRSA nasal carriers among haemodialysis patients with central venous catheters (CVCs). The aim of this study is to evaluate the risk factors, various clinical outcomes and effect of decolonization for MRSA nasal colonization among patients on haemodialysis via CVCs.
Methods
This was a single-centre non-concurrent cohort study of 676 patients who had new haemodialysis CVCs inserted. They were all screened for MRSA colonization via nasal swabs and were categorized into two groups: MRSA carriers and MRSA noncarriers. Potential risk factors and clinical outcomes were analysed in both groups. All MRSA carriers were given decolonization therapy and the effect of decolonization on subsequent MRSA infection was also performed.
Results
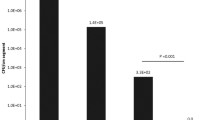
Eighty-two patients (12.1%) were MRSA carriers. Multivariate analysis showed that MRSA carrier (OR 5.44; 95% CI 3.02–9.79), long-term care facility resident (OR 4.08; 95% CI 2.07–8.05), history of Staphylococcus aureus infection (OR 3.20; 95% CI 1.42–7.20) and CVC in situ > 21 days (OR 2.12; 95% CI 1.15–3.93) were independent risk factors for MRSA infection. There was no significant difference in all-cause mortality between MRSA carriers and noncarriers. The MRSA infection rates were similar between MRSA carriers with successful decolonization and those who had failed/incomplete decolonization in our subgroup analysis.
Conclusion
MRSA nasal colonization is an important cause of MRSA infection among haemodialysis patients with CVCs. However, decolonization therapy may not be effective in reducing MRSA infection.

Similar content being viewed by others
References
Li Y, Friedman JY, O’Neal BF et al (2009) Outcomes of Staphylococcus aureus infection in haemodialysis-dependent patients. Clin J Am Soc Nephrol 4:428–434
Koziol-Montewka M, Chudnicka A, Ksiasek A, Majdan M (2001) Rate of Staphylococcus aureus nasal carriage in immunocompromised patients receiving haemodialyis treatment. Int J Antimicrob Agents 18:193–196
Lu PL, Tsai JC, Chiu YW et al (2008) Methicillin-resistant Staphylococcus aureus carriage, infection and transmission in dialysis patients, healthcare workers and their family members. Nephrol Dial Transplant 23:1659–1665
Centers for Disease Control and Prevention (2020) Healthcare-Associated Infections – Community Interface Surveillance Report, Emerging Infections Program Network, Methicillin-Resistant Staphylococcus aureus, 2017
Davis KA, Steward JJ, Crouch HK, Florez CE, Hospenthal DR (2004) Methicillin-resistant Staphylococcus aureus (MRSA) nares colonization at hospital admission and its effect on subsequent MRSA infection. Clin Infect Dis 39:776–782
Lai CF, Liao CH, Pai MF et al (2011) Nasal carriage of methicillin-resistant Staphylococcus aureus is associated with higher all-cause mortality in haemodialysis patient. Clin J Am Soc Nephrol 6:167–174
McGinigle KL, Gourlay ML, Buchanan IB (2008) The use of active surveillance cultures in adult intensive care units to reduce methicillin-resistant Staphylococcus aureus-related morbidity, mortality, and costs: a systematic review. Clin Infect Dis 46:1717–1725
Klevens RM, Edwards JR, Andrus ML, Peterson KD, Dudeck TC, Horan TC (2008) Dialysis surveillance report: National Healthcare Safety Network – Data summary for 2006. Semin Dial 21:24–28
Kluytmans JA, van Belkum A, Verbrugh H (1997) Nasal carriage of Staphylococcus aureus: epidemiology, underlying mechanisms, and associated risks. Clin Microbio Rev 10:505–520
Yu VL, Goetz A, Wagener M et al (1986) Staphylococcus aureus nasal carriage and infection in patients on haemodialysis. Efficacy of antibiotic prophylaxis. N Engl J Med 315:91–96
Kaplowitz LG, Comstock JA, Landwehr DM, Dalton HP, Mayhall CG (1988) Prospective study of microbial colonization of the nose and skin and infection of the vascular access site in haemodialysis patients. J Clin Microbiol 26:1257–1262
Daeschlein G, Assadian O, Rangous I, Kramer A (2006) Risk factors for Staphylococcus aureus nasal carriage in residents of three nursing homes in Germany. J Hosp Infect 63:216–220
Lederer SR, Riedelsdorf G, Schiffl H (2007) Nasal carriage of meticillin resistant Staphylococcus aureus: the prevalence, patients at risk and the effect of elimination on outcomes among outclinic haemodialysis patients. Eur J Med Res 12:284–288
Hadley AC, Karchmer TB, Russell GB, McBride DG, Freedman BI (2007) The prevalence of resistant bacterial colonization in chronic hemodialysis patients. Am J Nephrol 27:352–359
Department of Health and Central Renal Committee, Hospital Authority. Infection Control Guidelines on Nephrology Services in Hong Kong 2018 (3rd edn, version 3.2). https://www.chp.gov.hk/files/pdf/ic_gu_nephrology_services_in_hk.pdf. Accessed 4 Jan 2021
Coia JE, Duckworth GJ, Edwards DI, Joint Working Party of the British Society of Antimicrobial Chemotherapy; Hospital Infection Society; Infection Control Nurses Association et al (2006) Guidelines for the control and prevention of meticillin-resistant Staphylococcus aureus (MRSA) in healthcare facilities. J Hosp Infect 63(Suppl 1):S1–S44
Centers for Disease Control (2007) Invasive methicillin-resistant Staphylococcus aureus infections among dialysis patients, United States, 2005. MMWR Morb Mortal Wkly Rep 56:197–199
Yeoh LY, Tan FL, Willis GC, Ooi ST (2014) Methicillin-resistant Staphylococcus aureus carriage in hospitalized chronic haemodialysis patients and its predisposing factors. Hemodial Int 18:142–147
Johnson LB, Jose J, Yousif F, Pawlak J, Saravolatz LD (2009) Prevalence of colonization with community-associated methicillin-resistant Staphylococcus aureus among end-stage renal disease patients and healthcare workers. Infect Control Hosp Epidemiol 30:4–8
Price A, Sarween N, Gupta I, Baharani J (2015) Meticillin-resistant Staphylococcus aureus and meticillin-susceptible Staphylococcus aureus screening in a cohort of haemodialysis patients: carriage, demographics and outcomes. Journal of Hosp Infect 90:22–27
Leman R, Alvarado-Ramy F, Pocock S et al (2004) Nasal carriage of methicillin-resistant Staphylococcus aureus in an American Indian population. Infect Control Hosp Epidemiol 25:121–125
Ray GT, Suaya JA, Baxter R (2012) Trends and characteristics of culture-confirmed Staphylococcus aureus infections in a large U.S. integrated health care organization. J Clin Microbiol 50:1950–1957
Nielsen J, Ladefoged SD, Kolmos HJ (1998) Dialysis catheter-related septicaemia – focus on Staphylococcus aureus septicaemia. Nephrol Dial Transplant 13:2847–2852
Chuang VW, Tsang IH, Keung JP et al (2015) Infection control intervention on meticillin resistant Staphylococcus aureus transmission in residential care homes for the elderly. J Infect Prev 16:58–66
Wendt C, Svodoba D, Schmidt C, Bock-Hensley O, von Baum H (2005) Characteristics that promote transmission of Staphylococcus aureus in German nursing homes. Infect Control Hosp Epidemiol 26:816–821
Patel G, Jenkins SG, Mediavilla JR et al (2011) Clinical and molecular epidemiology of methicillin-resistant Staphylococcus aureus among patients in an ambulatory hemodialysis center. Infect Control Hosp Epidemiol 32:881–888
Kluytmans JA, Wertheim HF (2005) Nasal carriage of Staphylococcus aureus and prevention of nosocomial infections. Infection 33:3–8
Herwaldt LA (1998) Reduction of Staphylococcus aureus nasal carriage and infection in dialysis patients. J Hosp Infect 40(Suppl B):S13–S23
Laupland KB, Conly JM (2003) Treatment of Staphylococcus aureus colonization and prophylaxis for infection with topical intranasal mupirocin: an evidence-based review. Clin Infect Dis 37:933–938
Gebreselassie HM, Lo Priore E, Marschall J (2015) Effectiveness of meticillin-resistant Staphylococcus aureus decolonization in long-term haemodialysis patients: a systematic review and meta-analysis. J Hosp Infect 91:250–256
Boelaert JR, Van Landuyt HW, Godard CA et al (1993) Nasal mupirocin ointment decreases the incidence of Staphylococcus aureus bacteraemias in haemodialysis patients. Nephrol Dial Transplant 8:235–239
Kalmeijer MD, Coertjens H, van Nieuwland-Bollen E, deBaere G, Kluytmans J (2002) Surgical site infections in orthopedic surgery: the effect of mupirocin nasal ointment in a double-blind, randomized, placebo-controlled study. Clin Infect Dis 35:353–358
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that no conflict of interest exists.
Ethical approval
This study was conducted in accordance with the Declaration of Helsinki and was approved by the local Research Ethics Committee [REC (KC/KE)-20-0158/ER-3].
Informed consent
The requirement to obtain informed consent was waived based on the observational design.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wong, Y.T., Yeung, C.S., Chak, W.L. et al. Methicillin-resistant Staphylococcus aureus nasal carriage among patients on haemodialysis with newly inserted central venous catheters. Int Urol Nephrol 55, 2059–2066 (2023). https://doi.org/10.1007/s11255-023-03521-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03521-4