Abstract
Purpose
Glomerular hyperfiltration (GHF) has been associated with cardiovascular disease and all-cause mortality. We aimed to evaluate whether preoperative GHF is associated with 30-day complications following major urologic oncology procedures.
Methods
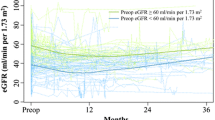
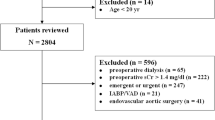
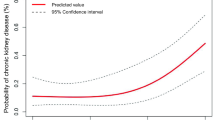
We conducted a retrospective cohort study using subjects from the 2006 to 2019 American College of Surgeons National Surgical Quality Improvement Program database who underwent prostatectomy, cystectomy, or nephrectomy. Estimated glomerular filtration rate (eGFR) was calculated using the CKD-EPI equation. Patients were classified as having either low, normal, or high eGFR based on the 5th and 95th percentiles of age- and sex-specific quintiles for eGFR. Using multivariable logistic regression, we evaluated GHF as an independent predictor of postoperative complications.
Results
A total of 120,013 patients were eligible for analysis, of which 1706 (1.4%) were identified as having GHF, with a median eGFR of 105.37 ml/min per 1.73 m2 (IQR 94.84–116.77). Compared to patients with normal eGFR, patients with GHF were older (68 years, [IQR 60–71], p < 0.001), had a lower BMI (27.52 kg/m2 [IQR 23.71–31.95], p < 0.001), and greater 5-item modified frailty index scores (≥ 1, 70.6%, p < 0.001). Multivariable logistic regression demonstrated that GHF was associated with greater odds of any complication (OR 1.23, 95% CI 1.08–1.40, p = 0.002), non-home discharge (OR 1.86, 95% CI 1.50–2.30, p < 0.001), and prolonged LOS (OR 1.33, 95% CI 1.18–1.51, p < 0.001).
Conclusion
GHF is associated with greater odds of 30-day complications following major urologic oncology surgery.



Similar content being viewed by others
References
Inker LA, Titan S (2021) Measurement and estimation of GFR for use in clinical practice: core curriculum 2021. Am J Kidney Dis 78(5):736–749. https://doi.org/10.1053/j.ajkd.2021.04.016
Helal I, Fick-Brosnahan GM, Reed-Gitomer B, Schrier RW (2012) Glomerular hyperfiltration: definitions, mechanisms and clinical implications. Nat Rev Nephrol 8(5):293–300. https://doi.org/10.1038/nrneph.2012.19
Cachat F, Combescure C, Cauderay M, Girardin E, Chehade H (2015) A systematic review of glomerular hyperfiltration assessment and definition in the medical literature. Clin J Am Soc Nephrol 10(3):382–389. https://doi.org/10.2215/CJN.03080314
Shilpasree AS, Patil VS, Revanasiddappa M, Patil VP, Ireshnavar D (2021) Renal dysfunction in prediabetes: confirmed by glomerular hyperfiltration and albuminuria. J Lab Physicians 13(3):257–262. https://doi.org/10.1055/s-0041-1731107
Rodriguez-Poncelas A, Franch-Nadal J, Coll-de Tuero G, Mata-Cases M, Alonso-Fernandez M, Mur-Marti T, Ruiz A, Giraldez-Garcia C, Regidor E (2019) High levels of fasting glucose and glycosylated hemoglobin values are associated with hyperfiltration in a Spanish prediabetes cohort. PREDAPS Study PLoS One 14(9):e0222848. https://doi.org/10.1371/journal.pone.0222848
Kanbay M, Ertuglu LA, Afsar B, Ozdogan E, Kucuksumer ZS, Ortiz A, Covic A, Kuwabara M, Cherney DZI, van Raalte DH, de Zeeuw D (2019) Renal hyperfiltration defined by high estimated glomerular filtration rate: a risk factor for cardiovascular disease and mortality. Diabetes Obes Metab 21(11):2368–2383. https://doi.org/10.1111/dom.13831
Dupuis ME, Nadeau-Fredette AC, Madore F, Agharazii M, Goupil R (2020) Association of glomerular hyperfiltration and cardiovascular risk in middle-aged healthy individuals. JAMA Netw Open 3(4):e202377. https://doi.org/10.1001/jamanetworkopen.2020.2377
Sundaram K, Warren JA, Krebs OK, Anis HK, Klika AK, Molloy RM, Higuera-Rueda CA, Barsoum WK, Piuzzi NS (2021) Estimated glomerular filtration rate is a prognosticator of adverse outcomes after primary total knee arthroplasty among patients with chronic kidney disease and glomerular hyperfiltration. Knee 28:36–44. https://doi.org/10.1016/j.knee.2020.11.008
Ui T, Obi Y, Shimomura A, Lefor AK, Fazl Alizadeh R, Said H, Nguyen NT, Stamos MJ, Kalantar-Zadeh K, Sata N, Ichii H (2019) High and low estimated glomerular filtration rates are associated with adverse outcomes in patients undergoing surgery for gastrointestinal malignancies. Nephrol Dial Transplant 34(5):810–818. https://doi.org/10.1093/ndt/gfy108
Konety BR, Allareddy V, Modak S, Smith B (2006) Mortality after major surgery for urologic cancers in specialized urology hospitals: are they any better? J Clin Oncol 24(13):2006–2012. https://doi.org/10.1200/JCO.2005.04.2622
American College of Surgeons (ACS). User guide for the 2019 ACS NSQIP participant use data file (PUF). (2020). https://www.facs.org/-/media/files/quality-programs/cancer/ncdb/puf_data_dictionary.ashx.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J, Ckd EPI (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612. https://doi.org/10.7326/0003-4819-150-9-200905050-00006
Subramaniam S, Aalberg JJ, Soriano RP, Divino CM (2018) New 5-factor modified frailty index using american college of surgeons NSQIP data. J Am Coll Surg 226(2):173–181 e178. https://doi.org/10.1016/j.jamcollsurg.2017.11.005
Stevens LA, Claybon MA, Schmid CH, Chen J, Horio M, Imai E, Nelson RG, Van Deventer M, Wang HY, Zuo L, Zhang YL, Levey AS (2011) Evaluation of the Chronic Kidney Disease Epidemiology Collaboration equation for estimating the glomerular filtration rate in multiple ethnicities. Kidney Int 79(5):555–562. https://doi.org/10.1038/ki.2010.462
Reboldi G, Verdecchia P, Fiorucci G, Beilin LJ, Eguchi K, Imai Y, Kario K, Ohkubo T, Pierdomenico SD, Schwartz JE, Wing L, Saladini F, Palatini P (2018) Glomerular hyperfiltration is a predictor of adverse cardiovascular outcomes. Kidney Int 93(1):195–203. https://doi.org/10.1016/j.kint.2017.07.013
Kanda Y (2013) Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant 48(3):452–458. https://doi.org/10.1038/bmt.2012.244
Park M, Yoon E, Lim YH, Kim H, Choi J, Yoon HJ (2015) Renal hyperfiltration as a novel marker of all-cause mortality. J Am Soc Nephrol 26(6):1426–1433. https://doi.org/10.1681/ASN.2014010115
Zengin A, Karataş MB, Çanga Y, Durmuş G, Güzelburç Ö, Yelgeç NS, Emre A (2021) Renal glomerular hyperfiltration is associated with poor prognosis in acute ST-elevation myocardial infarction. Renal Glomerüler Hiperfiltrasyon Akut ST-Yükselmeli Miyokard İnfarktüsünde Kötü Prognoz ile İlişkilidir 22(3):180–185. https://doi.org/10.4274/imj.galenos.2021.00243
Tomaszewski M, Charchar FJ, Maric C, McClure J, Crawford L, Grzeszczak W, Sattar N, Zukowska-Szczechowska E, Dominiczak AF (2007) Glomerular hyperfiltration: a new marker of metabolic risk. Kidney Int 71(8):816–821. https://doi.org/10.1038/sj.ki.5002160
Low S, Zhang X, Wang J, Yeoh LY, Liu YL, Ang KKL, Tang WE, Kwan PY, Tavintharan S, Sum CF, Lim SC (2018) Long-term prospective observation suggests that glomerular hyperfiltration is associated with rapid decline in renal filtration function: a multiethnic study. Diab Vasc Dis Res 15(5):417–423. https://doi.org/10.1177/1479164118776465
Razdan S, Eilender B, Pfail JP, Garcia M, Ranti D, Rosenzweig S, Djordjevic S, Hosseini A, Radros J, Mehrazin R, Wiklund PN, Sfakianos JP (2022) Higher preoperative eGFR is a predictor of worse renal function decline after robotic assisted radical cystectomy: implications for postoperative management. Urol Oncol 40 (6):275 e211–275 e218. https://doi.org/10.1016/j.urolonc.2022.02.011
Lee CU, Choi DK, Chung JH, Song W, Kang M, Sung HH, Jeong BC, Seo SI, Jeon SS, Lee HM, Jeon HG (2021) Comparison of risk factors for the development of proteinuria after radical nephrectomy for renal cell carcinoma. Res Rep Urol 13:407–414. https://doi.org/10.2147/RRU.S317543
Selph JP, Whited WM, Smith AB, Matthews J, Pruthi RS, Wallen EM, Nielsen ME, Woods ME (2014) Metabolic syndrome as a predictor for postoperative complications after urologic surgery. Urology 83(5):1051–1059. https://doi.org/10.1016/j.urology.2014.01.014
Cortinovis M, Perico N, Ruggenenti P, Remuzzi A, Remuzzi G (2022) Glomerular hyperfiltration. Nat Rev Nephrol. https://doi.org/10.1038/s41581-022-00559-y
Oh SW, Yang JH, Kim MG, Cho WY, Jo SK (2020) Renal hyperfiltration as a risk factor for chronic kidney disease: a health checkup cohort study. PLoS ONE 15(9):e0238177. https://doi.org/10.1371/journal.pone.0238177
Schmid M, Ravi P, Abd-El-Barr AE, Klap J, Sammon JD, Chang SL, Menon M, Kibel AS, Fisch M, Trinh QD (2014) Chronic kidney disease and perioperative outcomes in urological oncological surgery. Int J Urol 21(12):1245–1252. https://doi.org/10.1111/iju.12563
Gacci M, Russo GI, De Nunzio C, Sebastianelli A, Salvi M, Vignozzi L, Tubaro A, Morgia G, Serni S (2017) Meta-analysis of metabolic syndrome and prostate cancer. Prostate Cancer Prostatic Dis 20(2):146–155. https://doi.org/10.1038/pcan.2017.1
Kwatra NS, Meany HJ, Ghelani SJ, Zahavi D, Pandya N, Majd M (2017) Glomerular hyperfiltration in children with cancer: prevalence and a hypothesis. Pediatr Radiol 47(2):221–226. https://doi.org/10.1007/s00247-016-3733-5
Shiloach M, Frencher SK Jr, Steeger JE, Rowell KS, Bartzokis K, Tomeh MG, Richards KE, Ko CY, Hall BL (2010) Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg 210(1):6–16. https://doi.org/10.1016/j.jamcollsurg.2009.09.031
Soveri I, Berg UB, Bjork J, Elinder CG, Grubb A, Mejare I, Sterner G, Back SE, Groupaa SGR (2014) Measuring GFR: a systematic review. Am J Kidney Dis 64 (3):411-424. https://doi.org/10.1053/j.ajkd.2014.04.010
Funding
No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
CR: conceptualization; data curation; formal analysis; methodology; software; writing–original draft. VC: writing–Review and editing. EDV: writing—review and editing. MB: writing–review and editing. AF: writing–review and editing. DK: supervision. KCB: project administration; resources; supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Ethics approval
This study was deemed exempt from ethics approval as the database used contains deidentified data.
Disclosure
The American College of Surgeons National Surgical Quality Improvement Program and the hospitals participating in the ACS NSQIP are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Riveros, C., Chalfant, V., Di Valerio, E. et al. Glomerular hyperfiltration is a predictor of adverse outcomes following major urologic oncology surgery. Int Urol Nephrol 55, 229–239 (2023). https://doi.org/10.1007/s11255-022-03400-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-022-03400-4