Abstract
Background
Hemodynamic instability in patients undergoing kidney replacement therapy (KRT) is one of the most common and essential factors influencing mortality, morbidity, and the quality of life in this patient population.
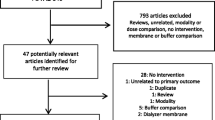
Method
Decreased cardiac preload, reduced systemic vascular resistance, redistribution of fluids, fluid overload, inflammatory factors, and changes in plasma osmolality have all been implicated in the pathophysiology of hemodynamic instability associated with KRT.
Result
A cascade of these detrimental mechanisms may ultimately cause intra-dialytic hypotension, reduced tissue perfusion, and impaired kidney rehabilitation. Multiple parameters, including dialysate composition, temperature, posture during dialysis sessions, physical activity, fluid administrations, dialysis timing, and specific pharmacologic agents, have been studied as possible management modalities. Nevertheless, a clear consensus is not reached.
Conclusion
This review includes a thorough investigation of the literature on hemodynamic instability in KRT patients, providing insight on interventions that may potentially minimize factors leading to hemodynamic instability.



Similar content being viewed by others
References
Douvris A, Zeid K, Hiremath S, Bagshaw SM, Wald R, Beaubien-Souligny W et al (2019) Mechanisms for hemodynamic instability related to renal replacement therapy: a narrative review. Intensive Care Med 45(10):1333–1346
Tonelli M, Astephen P, Andreou P, Beed S, Lundrigan P, Jindal K (2002) Blood volume monitoring in intermittent hemodialysis for acute renal failure. Kidney Int 62(3):1075–1080
Tanguay TA, Jensen L, Johnston C (2007) Predicting episodes of hypotension by continuous blood volume monitoring among critically ill patients in acute renal failure on intermittent hemodialysis. Dynamics 18(3):19–24
Bitker L, Bayle F, Yonis H, Gobert F, Leray V, Taponnier R et al (2016) Prevalence and risk factors of hypotension associated with preload-dependence during intermittent hemodialysis in critically ill patients. Crit Care 20:44
Uchino S, Bellomo R, Morimatsu H, Morgera S, Schetz M, Tan I et al (2007) Continuous renal replacement therapy: a worldwide practice survey. The beginning and ending supportive therapy for the kidney (B.E.S.T. kidney) investigators. Intensive Care Med 33(9):1563–1570
Akhoundi A, Singh B, Vela M, Chaudhary S, Monaghan M, Wilson GA et al (2015) Incidence of adverse events during continuous renal replacement therapy. Blood Purif 39(4):333–339
Tislér A, Akócsi K, Hárshegyi I, Varga G, Ferenczi S, Grosz M et al (2002) Comparison of dialysis and clinical characteristics of patients with frequent and occasional hemodialysis-associated hypotension. Kidney Blood Press Res 25(2):97–102
K/DOQI Workgroup (2005) K/DOQI clinical practice guidelines for cardiovascular disease in dialysis patients. Am J Kidney Dis 45(4 Suppl 3):S1–153. https://www.ajkd.org/article/S0272-6386(05)00092-2/fulltext
Capuano A, Sepe V, Cianfrone P, Castellano T, Andreucci VE (1990) Cardiovascular impairment, dialysis strategy and tolerance in elderly and young patients on maintenance haemodialysis. Nephrol Dial Transplant 5(12):1023–1030
Flythe JE, Chang TI, Gallagher MP, Lindley E, Madero M, Sarafidis PA et al (2020) Blood pressure and volume management in dialysis: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int 97(5):861–876
Keane DF, Raimann JG, Zhang H, Willetts J, Thijssen S, Kotanko P (2021) The time of onset of intradialytic hypotension during a hemodialysis session associates with clinical parameters and mortality. Kidney Int 99(6):1408–1417
Moore TJ, Lazarus JM, Hakim RM (1989) Reduced angiotensin receptors and pressor responses in hypotensive hemodialysis patients. Kidney Int 36(4):696–701
Burton JO, Jefferies HJ, Selby NM, McIntyre CW (2009) Hemodialysis-induced repetitive myocardial injury results in global and segmental reduction in systolic cardiac function. Clin J Am Soc Nephrol 4(12):1925–1931
Pillinger NL, Kam P (2017) Endothelial glycocalyx: basic science and clinical implications. Anaesth Intensive Care 45(3):295–307
Doshi M, Murray PT (2003) Approach to intradialytic hypotension in intensive care unit patients with acute renal failure. Artif Organs 27(9):772–780
Van der Mullen J, Wise R, Vermeulen G, Moonen PJ, Malbrain M (2018) Assessment of hypovolaemia in the critically ill. Anaesthesiol Intensive Ther 50(2):141–149
Silversides JA, Pinto R, Kuint R, Wald R, Hladunewich MA, Lapinsky SE et al (2014) Fluid balance, intradialytic hypotension, and outcomes in critically ill patients undergoing renal replacement therapy: a cohort study. Crit Care 18(6):624
Vincent JL, Sakr Y, Sprung CL, Ranieri VM, Reinhart K, Gerlach H et al (2006) Sepsis in European intensive care units: results of the SOAP study. Crit Care Med 34(2):344–353
Payen D, de Pont AC, Sakr Y, Spies C, Reinhart K, Vincent JL (2008) A positive fluid balance is associated with a worse outcome in patients with acute renal failure. Crit Care 12(3):R74
Murugan R, Balakumar V, Kerti SJ, Priyanka P, Chang CH, Clermont G et al (2018) Net ultrafiltration intensity and mortality in critically ill patients with fluid overload. Crit Care 22(1):223
Reilly RF (2014) Attending rounds: a patient with intradialytic hypotension. Clin J Am Soc Nephrol 9(4):798–803
Monnet X, Teboul JL (2015) Passive leg raising: five rules, not a drop of fluid! Crit Care 19(1):18
Monnet X, Cipriani F, Camous L, Sentenac P, Dres M, Krastinova E et al (2016) The passive leg raising test to guide fluid removal in critically ill patients. Ann Intensive Care 6(1):46
Schortgen F, Soubrier N, Delclaux C, Thuong M, Girou E, Brun-Buisson C et al (2000) Hemodynamic tolerance of intermittent hemodialysis in critically ill patients: usefulness of practice guidelines. Am J Respir Crit Care Med 162(1):197–202
Verbrugge FH, Dupont M, Steels P, Grieten L, Malbrain M, Tang WH et al (2013) Abdominal contributions to cardiorenal dysfunction in congestive heart failure. J Am Coll Cardiol 62(6):485–495
Converse RL Jr, Jacobsen TN, Jost CM, Toto RD, Grayburn PA, Obregon TM et al (1992) Paradoxical withdrawal of reflex vasoconstriction as a cause of hemodialysis-induced hypotension. J Clin Invest 90(5):1657–1665
Shimizu K, Kurosawa T, Sanjo T (2008) Effect of hyperosmolality on vasopressin secretion in intradialytic hypotension: a mechanistic study. Am J Kidney Dis 52(2):294–304
Cernaro V, Lacquaniti A, Lorenzano G, Loddo S, Romeo A, Donato V et al (2012) Apelin, plasmatic osmolality and hypotension in dialyzed patients. Blood Purif 33(4):317–323
Stabellini G, Bosi GP, Valeno V, Pellati A, Masotti M, Fiocchi O et al (1998) Relation between the osmolality trend and ornithine decarboxylase activity in red blood cells of uremic patients during hemodialytic treatment. Biomed Pharmacother 52(4):166–168
Fasanella d’Amore T, Wauters JP, Waeber B, Nussberger J, Brunner HR (1985) Response of plasma vasopressin to changes in extracellular volume and/or plasma osmolality in patients on maintenance hemodialysis. Clin Nephrol 23(6):299–302
Mc Causland FR, Waikar SS (2015) Association of predialysis calculated plasma osmolarity with intradialytic blood pressure decline. Am J Kidney Dis 66(3):499–506
Mc Causland FR, Brunelli SM, Waikar SS (2013) Dialysis dose and intradialytic hypotension: results from the HEMO study. Am J Nephrol 38(5):388–396
Lynch KE, Ghassemi F, Flythe JE, Feng M, Ghassemi M, Celi LA et al (2016) Sodium modelling to reduce intradialytic hypotension during haemodialysis for acute kidney injury in the intensive care unit. Nephrology (Carlton) 21(10):870–877
Lima EQ, Silva RG, Donadi EL, Fernandes AB, Zanon JR, Pinto KR et al (2012) Prevention of intradialytic hypotension in patients with acute kidney injury submitted to sustained low-efficiency dialysis. Ren Fail 34(10):1238–1243
Paganini EP, Sandy D, Moreno L, Kozlowski L, Sakai K (1996) The effect of sodium and ultrafiltration modelling on plasma volume changes and haemodynamic stability in intensive care patients receiving haemodialysis for acute renal failure: a prospective, stratified, randomized, cross-over study. Nephrol Dial Transplant 11(Suppl 8):32–37
Brummelhuis WJ, van Geest RJ, van Schelven LJ, Boer WH (2009) Sodium profiling, but not cool dialysate, increases the absolute plasma refill rate during hemodialysis. Asaio j 55(6):575–580
Flythe JE, Xue H, Lynch KE, Curhan GC, Brunelli SM (2015) Association of mortality risk with various definitions of intradialytic hypotension. J Am Soc Nephrol 26(3):724–734
Yu J, Liu Z, Shen B, Teng J, Zou J, Ding X (2018) Intradialytic hypotension as an independent risk factor for long-term mortality in maintaining hemodialysis patients: a 5-year follow-up cohort study. Blood Purif 45(4):320–326
Vincent JL, De Backer D, Wiedermann CJ (2016) Fluid management in sepsis: the potential beneficial effects of albumin. J Crit Care 35:161–167
Weil MH, Henning RJ, Puri VK (1979) Colloid oncotic pressure: clinical significance. Crit Care Med 7(3):113–116
Ricci Z, Romagnoli S, Ronco C (2018) The 10 false beliefs in adult critical care nephrology. Intensive Care Med 44(8):1302–1305
Sherman RA (2016) We lower blood flow for intradialytic hypotension. Semin Dial 29(4):295–296
Schytz PA, Mace ML, Soja AM, Nilsson B, Karamperis N, Kristensen B et al (2015) Impact of extracorporeal blood flow rate on blood pressure, pulse rate and cardiac output during haemodialysis. Nephrol Dial Transplant 30(12):2075–2079
Trivedi HS, Kukla A, Prowant B, Lim HJ (2007) A study of the extracorporeal rate of blood flow and blood pressure during hemodialysis. Hemodial Int 11(4):424–429
McIntyre CW, Burton JO, Selby NM, Leccisotti L, Korsheed S, Baker CS et al (2008) Hemodialysis-induced cardiac dysfunction is associated with an acute reduction in global and segmental myocardial blood flow. Clin J Am Soc Nephrol 3(1):19–26
Buchanan C, Mohammed A, Cox E, Köhler K, Canaud B, Taal MW et al (2017) Intradialytic cardiac magnetic resonance imaging to assess cardiovascular responses in a short-term trial of hemodiafiltration and hemodialysis. J Am Soc Nephrol 28(4):1269–1277
Aneman A, Vieillard-Baron A (2016) Cardiac dysfunction in sepsis. Intensive Care Med 42(12):2073–2076
Mahmoud H, Forni LG, McIntyre CW, Selby NM (2017) Myocardial stunning occurs during intermittent haemodialysis for acute kidney injury. Intensive Care Med 43(6):942–944
Slessarev M, Salerno F, Ball IM, McIntyre CW (2019) Continuous renal replacement therapy is associated with acute cardiac stunning in critically ill patients. Hemodial Int 23(3):325–332
Schindler R, Beck W, Deppisch R, Aussieker M, Wilde A, Göhl H et al (2004) Short bacterial DNA fragments: detection in dialysate and induction of cytokines. J Am Soc Nephrol 15(12):3207–3214
Bommer J, Becker KP, Urbaschek R (1996) Potential transfer of endotoxin across high-flux polysulfone membranes. J Am Soc Nephrol 7(6):883–888
Schiffl H (2011) High-flux dialyzers, backfiltration, and dialysis fluid quality. Semin Dial 24(1):1–4
Ra WARD (2007) Worldwide water standards for hemodialysis. Hemodial Int 11(s1):S18–S25
Moore I, Bhat R, Hoenich NA, Kilner AJ, Prabhu M, Orr KE et al (2009) A microbiological survey of bicarbonate-based replacement circuits in continuous veno-venous hemofiltration. Crit Care Med 37(2):496–500
Levy B, Fritz C, Tahon E, Jacquot A, Auchet T, Kimmoun A (2018) Vasoplegia treatments: the past, the present, and the future. Crit Care 22(1):52
Fani F, Regolisti G, Delsante M, Cantaluppi V, Castellano G, Gesualdo L et al (2018) Recent advances in the pathogenetic mechanisms of sepsis-associated acute kidney injury. J Nephrol 31(3):351–359
Peerapornratana S, Manrique-Caballero CL, Gómez H, Kellum JA (2019) Acute kidney injury from sepsis: current concepts, epidemiology, pathophysiology, prevention and treatment. Kidney Int 96(5):1083–1099
Pun PH, Horton JR, Middleton JP (2013) Dialysate calcium concentration and the risk of sudden cardiac arrest in hemodialysis patients. Clin J Am Soc Nephrol 8(5):797–803
Afshinnia F, Belanger K, Palevsky PM, Young EW (2013) Effect of ionized serum calcium on outcomes in acute kidney injury needing renal replacement therapy: secondary analysis of the acute renal failure trial network study. Ren Fail 35(10):1310–1318
Fellner SK, Lang RM, Neumann A, Spencer KT, Bushinsky DA, Borow KM (1989) Physiological mechanisms for calcium-induced changes in systemic arterial pressure in stable dialysis patients. Hypertension 13(3):213–218
Scholze A, Maier A, Stocks F, Karamohamad F, Vetter R, Zidek W et al (2005) Sustained increase of extracellular calcium concentration causes arterial vasoconstriction in humans. J Hypertens 23(11):2049–2054
Schepelmann M, Yarova PL, Lopez-Fernandez I, Davies TS, Brennan SC, Edwards PJ et al (2016) The vascular Ca2+-sensing receptor regulates blood vessel tone and blood pressure. Am J Physiol Cell Physiol 310(3):C193-204
Haddy FJ, Vanhoutte PM, Feletou M (2006) Role of potassium in regulating blood flow and blood pressure. Am J Physiol Regul Integr Comp Physiol 290(3):R546–R552
Dolson GM, Ellis KJ, Bernardo MV, Prakash R, Adrogué HJ (1995) Acute decreases in serum potassium augment blood pressure. Am J Kidney Dis 26(2):321–326
Gabutti L, Salvadé I, Lucchini B, Soldini D, Burnier M (2011) Haemodynamic consequences of changing potassium concentrations in haemodialysis fluids. BMC Nephrol 12:14
Patel S, Raimann JG, Kotanko P (2017) The impact of dialysis modality and membrane characteristics on intradialytic hypotension. Semin Dial 30(6):518–531
Haroon S, Davenport A (2018) Choosing a dialyzer: What clinicians need to know. Hemodial Int 22(S2):S65-s74
Heegard KD, Tilley MA, Stewart IJ, Edgecombe HP, Lundy JB, Renz EM et al (2013) Anaphylactoid reaction during first hemofiltration with a PUREMA polysulfone membrane. Int J Artif Organs 36(5):363–366
Ansorge W, Pelger M, Dietrich W, Baurmeister U (1987) Ethylene oxide in dialyzer rinsing fluid: effect of rinsing technique, dialyzer storage time, and potting compound. Artif Organs 11(2):118–122
Müller TF, Seitz M, Eckle I, Lange H, Kolb G (1998) Biocompatibility differences with respect to the dialyzer sterilization method. Nephron 78(2):139–142
Dolovich J, Bell B (1978) Allergy to a product(s) of ethylene oxide gas: demonstration of IgE and IgG antibodies and hapten specificity. J Allergy Clin Immunol 62(1):30–32
Tielemans C, Madhoun P, Lenaers M, Schandene L, Goldman M, Vanherweghem JL (1990) Anaphylactoid reactions during hemodialysis on AN69 membranes in patients receiving ACE inhibitors. Kidney Int 38(5):982–984
Kokubo K, Kurihara Y, Kobayashi K, Tsukao H, Kobayashi H (2015) Evaluation of the biocompatibility of dialysis membranes. Blood Purif 40(4):293–297
Itoh S, Susuki C, Tsuji T (2006) Platelet activation through interaction with hemodialysis membranes induces neutrophils to produce reactive oxygen species. J Biomed Mater Res A 77(2):294–303
Stricker KH, Takala J, Hullin R, Ganter CC (2009) When drugs disappear from the patient: elimination of intravenous medication by hemodiafiltration. Anesth Analg 109(5):1640–1643
Mohammad A, Zafar N, Feerick A (2010) Cardiac arrest in intensive care unit: Case report and future recommendations. Saudi J Anaesth 4(1):31–34
Rosa AA, Fryd DS, Kjellstrand CM (1980) Dialysis symptoms and stabilization in long-term dialysis. Practical application of the CUSUM plot. Arch Intern Med 140(6):804–807
McGuire S, Horton EJ, Renshaw D, Jimenez A, Krishnan N, McGregor G (2018) Hemodynamic instability during dialysis: the potential role of intradialytic exercise. Biomed Res Int 2018:8276912
Sharma S, Waikar SS (2017) Intradialytic hypotension in acute kidney injury requiring renal replacement therapy. Semin Dial 30(6):553–558
Basile C, Pisano A, Lisi P, Rossi L, Lomonte C, Bolignano D (2016) High versus low dialysate sodium concentration in chronic haemodialysis patients: a systematic review of 23 studies. Nephrol Dial Transplant 31(4):548–563
Munoz Mendoza J, Arramreddy R, Schiller B (2015) Dialysate sodium: choosing the optimal hemodialysis bath. Am J Kidney Dis 66(4):710–720
Venkatasubba Rao CP, Bershad EM, Calvillo E, Maldonado N, Damani R, Mandayam S et al (2018) Real-time noninvasive monitoring of intracranial fluid shifts during dialysis using volumetric integral phase-shift spectroscopy (VIPS): a proof-of-concept study. Neurocrit Care 28(1):117–126
Ertuglu LA, Demiray A, Basile C, Afsar B, Covic A, Kanbay M (2021) Sodium and ultrafiltration profiling in hemodialysis: a long-forgotten issue revisited. Hemodial Int 25(4):433–446
Rosales LM, Schneditz D, Morris AT, Rahmati S, Levin NW (2000) Isothermic hemodialysis and ultrafiltration. Am J Kidney Dis 36(2):353–361
Maggiore Q, Pizzarelli F, Sisca S, Catalano C, Delfino D (1984) Vascular stability and heat in dialysis patients. Contrib Nephrol 41:398–402
Jost CM, Agarwal R, Khair-el-Din T, Grayburn PA, Victor RG, Henrich WL (1993) Effects of cooler temperature dialysate on hemodynamic stability in “problem” dialysis patients. Kidney Int 44(3):606–612
Selby NM, Burton JO, Chesterton LJ, McIntyre CW (2006) Dialysis-induced regional left ventricular dysfunction is ameliorated by cooling the dialysate. Clin J Am Soc Nephrol 1(6):1216–1225
Curley FJ (1995) Hypothermia: a critical problem in the intensive care unit. J Intensive Care Med 10(1):1–2
Manthous CA, Hall JB, Olson D, Singh M, Chatila W, Pohlman A et al (1995) Effect of cooling on oxygen consumption in febrile critically ill patients. Am J Respir Crit Care Med 151(1):10–14
Rokyta R Jr, Matejovic M, Krouzecky A, Opatrny K Jr, Ruzicka J, Novak I (2004) Effects of continuous venovenous haemofiltration-induced cooling on global haemodynamics, splanchnic oxygen and energy balance in critically ill patients. Nephrol Dial Transplant 19(3):623–630
Robert R, Méhaud JE, Timricht N, Goudet V, Mimoz O, Debaene B (2012) Benefits of an early cooling phase in continuous renal replacement therapy for ICU patients. Ann Intensive Care 2(1):40
Knoll GA, Grabowski JA, Dervin GF, O’Rourke K (2004) A randomized, controlled trial of albumin versus saline for the treatment of intradialytic hypotension. J Am Soc Nephrol 15(2):487–492
Jardin F, Prost JF, Ozier Y, Margairaz A (1982) Hemodialysis in septic patients: improvements in tolerance of fluid removal with concentrated albumin as the priming fluid. Crit Care Med 10(10):650–652
Macedo E, Karl B, Lee E, Mehta RL (2021) A randomized trial of albumin infusion to prevent intradialytic hypotension in hospitalized hypoalbuminemic patients. Crit Care 25(1):18
Henrich WL, Woodard TD, Blachley JD, Gomez-Sanchez C, Pettinger W, Cronin RE (1980) Role of osmolality in blood pressure stability after dialysis and ultrafiltration. Kidney Int 18(4):480–488
Mc Causland FR, Prior LM, Heher E, Waikar SS (2012) Preservation of blood pressure stability with hypertonic mannitol during hemodialysis initiation. Am J Nephrol 36(2):168–174
Nette RW, Krepel HP, van den Meiracker AH, Weimar W, Zietse R (2002) Specific effect of the infusion of glucose on blood volume during haemodialysis. Nephrol Dial Transplant 17(7):1275–1280
van der Sande FM, Kooman JP, Barendregt JN, Nieman FH, Leunissen KM (1999) Effect of intravenous saline, albumin, or hydroxyethylstarch on blood volume during combined ultrafiltration and hemodialysis. J Am Soc Nephrol 10(6):1303–1308
Rubinstein S, Haimov M, Ross MJ (2008) Midodrine-induced vascular ischemia in a hemodialysis patient: a case report and literature review. Ren Fail 30(8):808–812
Parsaik AK, Singh B, Altayar O, Mascarenhas SS, Singh SK, Erwin PJ et al (2013) Midodrine for orthostatic hypotension: a systematic review and meta-analysis of clinical trials. J Gen Intern Med 28(11):1496–1503
Prakash S, Garg AX, Heidenheim AP, House AA (2004) Midodrine appears to be safe and effective for dialysis-induced hypotension: a systematic review. Nephrol Dial Transplant 19(10):2553–2558
van der Zee S, Thompson A, Zimmerman R, Lin J, Huan Y, Braskett M et al (2007) Vasopressin administration facilitates fluid removal during hemodialysis. Kidney Int 71(4):318–324
du Cheyron D, Terzi N, Seguin A, Valette X, Prevost F, Ramakers M et al (2013) Use of online blood volume and blood temperature monitoring during haemodialysis in critically ill patients with acute kidney injury: a single-centre randomized controlled trial. Nephrol Dial Transplant 28(2):430–437
Beladi Mousavi SS, Tamadon MR (2014) Vasopressin and prevention of hypotension during hemodialysis. Iran Red Crescent Med J 16(11):e20219
Dungey M, Bishop NC, Young HM, Burton JO, Smith AC (2015) The impact of exercising during haemodialysis on blood pressure, markers of cardiac injury and systemic inflammation-preliminary results of a pilot study. Kidney Blood Press Res 40(6):593–604
Mohseni R, Emami Zeydi A, Ilali E, Adib-Hajbaghery M, Makhlough A (2013) The effect of intradialytic aerobic exercise on dialysis efficacy in hemodialysis patients: a randomized controlled trial. Oman Med J 28(5):345–349
Ookawara S, Miyazawa H, Ito K, Ueda Y, Kaku Y, Hirai K et al (2016) Blood volume changes induced by low-intensity intradialytic exercise in long-term hemodialysis patients. Asaio j 62(2):190–196
March DS, Graham-Brown MP, Stover CM, Bishop NC, Burton JO (2017) Intestinal barrier disturbances in haemodialysis patients: mechanisms, consequences, and therapeutic options. Biomed Res Int 2017:5765417
Bivins HG, Knopp R, dos Santos PA (1985) Blood volume distribution in the Trendelenburg position. Ann Emerg Med 14(7):641–643
Sibbald WJ, Paterson NA, Holliday RL, Baskerville J (1979) The Trendelenburg position: hemodynamic effects in hypotensive and normotensive patients. Crit Care Med 7(5):218–224
Coll E, Vallès M, Torguet P, Bronsoms J, Maté G, Mauri JM (2004) Evaluation of plasma volume variation during different hemodialysis maneuvers. Nefrologia 24(5):463–469
Brunet P, Saingra Y, Leonetti F, Vacher-Coponat H, Ramananarivo P, Berland Y (1996) Tolerance of haemodialysis: a randomized cross-over trial of 5-h versus 4-h treatment time. Nephrol Dial Transplant 11(Suppl 8):46–51
Fagugli RM, Reboldi G, Quintaliani G, Pasini P, Ciao G, Cicconi B et al (2001) Short daily hemodialysis: blood pressure control and left ventricular mass reduction in hypertensive hemodialysis patients. Am J Kidney Dis 38(2):371–376
André MB, Rembold SM, Pereira CM, Lugon JR (2002) Prospective evaluation of an in-center daily hemodialysis program: results of two years of treatment. Am J Nephrol 22(5–6):473–479
Okada K, Abe M, Hagi C, Maruyama T, Maruyama N, Ito K et al (2005) Prolonged protective effect of short daily hemodialysis against dialysis-induced hypotension. Kidney Blood Press Res 28(2):68–76
Heidenheim AP, Muirhead N, Moist L, Lindsay RM (2003) Patient quality of life on quotidian hemodialysis. Am J Kidney Dis 42(1 Suppl):36–41
Kanbay M, Ertuglu LA, Afsar B, Ozdogan E, Siriopol D, Covic A et al (2020) An update review of intradialytic hypotension: concept, risk factors, clinical implications and management. Clin Kidney J 13(6):981–993
John S, Griesbach D, Baumgärtel M, Weihprecht H, Schmieder RE, Geiger H (2001) Effects of continuous haemofiltration vs intermittent haemodialysis on systemic haemodynamics and splanchnic regional perfusion in septic shock patients: a prospective, randomized clinical trial. Nephrol Dial Transplant 16(2):320–327
Schefold JC, von Haehling S, Pschowski R, Bender T, Berkmann C, Briegel S et al (2014) The effect of continuous versus intermittent renal replacement therapy on the outcome of critically ill patients with acute renal failure (CONVINT): a prospective randomized controlled trial. Crit Care 18(1):R11
Kielstein JT, Kretschmer U, Ernst T, Hafer C, Bahr MJ, Haller H et al (2004) Efficacy and cardiovascular tolerability of extended dialysis in critically ill patients: a randomized controlled study. Am J Kidney Dis 43(2):342–349
Uehlinger DE, Jakob SM, Ferrari P, Eichelberger M, Huynh-Do U, Marti HP et al (2005) Comparison of continuous and intermittent renal replacement therapy for acute renal failure. Nephrol Dial Transplant 20(8):1630–1637
Augustine JJ, Sandy D, Seifert TH, Paganini EP (2004) A randomized controlled trial comparing intermittent with continuous dialysis in patients with ARF. Am J Kidney Dis 44(6):1000–1007
Russo DS, Eugenio CS, Balestrin IG, Rodrigues CG, Rosa RG, Teixeira C et al (2022) Comparison of hemodynamic instability among continuous, intermittent and hybrid renal replacement therapy in acute kidney injury: a systematic review of randomized clinical trials. J Crit Care 69:153998
Aberegg SK (2016) Ionized calcium in the ICU: should it be measured and corrected? Chest 149(3):846–855
Heering P, Ivens K, Thümer O, Braüse M, Grabensee B (1999) Acid-base balance and substitution fluid during continuous hemofiltration. Kidney Int Suppl 72:S37-40
Tian JH, Ma B, Yang K, Liu Y, Tan J, Liu TX (2015) Bicarbonate- versus lactate-buffered solutions for acute continuous haemodiafiltration or haemofiltration. Cochrane Database Syst Rev 3:Cd006819
Davenport A, Davison AM, Will EJ (1993) Membrane biocompatibility: effects on cardiovascular stability in patients on hemofiltration. Kidney Int Suppl 41:S230–S234
Hakim RM, Wingard RL, Parker RA (1994) Effect of the dialysis membrane in the treatment of patients with acute renal failure. N Engl J Med 331(20):1338–1342
Alonso A, Lau J, Jaber BL (2005) Biocompatible hemodialysis membranes for acute renal failure. Cochrane Database Syst Rev 2:Cd005283
Jaber BL, Lau J, Schmid CH, Karsou SA, Levey AS, Pereira BJ (2002) Effect of biocompatibility of hemodialysis membranes on mortality in acute renal failure: a meta-analysis. Clin Nephrol 57(4):274–282
Subramanian S, Venkataraman R, Kellum JA (2002) Influence of dialysis membranes on outcomes in acute renal failure: a meta-analysis. Kidney Int 62(5):1819–1823
Maheut H, Lacour F (2001) Using AN69 ST membrane: a dialysis centre experience. Nephrol Dial Transplant 16(7):1519–1520
Coppo R, Amore A, Cirina P, Scelfo B, Giacchino F, Comune L et al (2000) Bradykinin and nitric oxide generation by dialysis membranes can be blunted by alkaline rinsing solutions. Kidney Int 58(2):881–888
Sars B, van der Sande FM, Kooman JP (2020) Intradialytic hypotension: mechanisms and outcome. Blood Purif 49(1–2):158–167
Sumi H, Ishii A, Yamada Y, Shibagaki Y, Tominaga N (2022) Central volume shift in acute heart failure revealed by blood volume monitoring during haemodialysis. Clin Kidney J 15(5):1007–1009
Funding
This study was not funded by any grant.
Author information
Authors and Affiliations
Contributions
Contributed substantially to the conception or design of the work: ABY, SV, MK, AC. Drafted the work and revised it critically for important intellectual content: ABY, SV, AC, AB, MK.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yildiz, A.B., Vehbi, S., Covic, A. et al. An update review on hemodynamic instability in renal replacement therapy patients. Int Urol Nephrol 55, 929–942 (2023). https://doi.org/10.1007/s11255-022-03389-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-022-03389-w