Abstract
Purpose
Excessive alkalization will increase the incidence of nephrolithiasis. Sodium bicarbonate (NaHCO3) and potassium sodium hydrogen citrate (PSHC) are commonly used drugs for urinary alkalization. We designed a trial to compare PSHC with NaHCO3 in the urine alkalization for the Chinese healthy participants and to explore the effects of PSHC and NaHCO3 on circadian rhythms of urine pH value.
Method
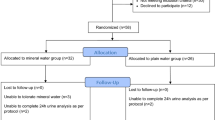
This study was a prospective, crossover, randomized, controlled trial, in which a total of 34 healthy volunteers participated in two study phases and took PSHC and NaHCO3 at the maintenance dose, respectively.
Result
The average level of urine pH of PSHC participants in 24 h was significantly higher than that of NaHCO3 (P < 0.001). The urine pH value of participants taking PSHC and NaHCO3 or under physiological conditions showed significant variation in 24 h (P < 0.05) and fitted to a mathematical model (Fourier series). Under physiological conditions, the average urine pH value in the daytime was higher than that in the night, and reached the peak at about 10:00, 16:00, and 22:00. The peak of urine pH at 24 h after taking PSHC and NaHCO3 was both higher than the baseline. The peak time of urine pH and the curve trend were similar, but the peak value in PSHC group was significantly higher than that in NaHCO3 group.
Conclusions
There was a circadian rhythm of urine pH value under physiological conditions. PSHC was more effective in urinary alkalization than NaHCO3 at the current maintenance oral dose and administration time without changing the rhythm of urine pH value.
Clinical trial registration
NCT04352153.


Similar content being viewed by others
References
Sorokin I, Mamoulakis C, Miyazawa K, Rodgers A, Talati J, Lotan Y (2017) Epidemiology of stone disease across the world. World J Urol 35(9):1301–1320. https://doi.org/10.1007/s00345-017-2008-6
Keoghane S, Walmsley B, Hodgson D (2010) The natural history of untreated renal tract calculi. BJU Int 105(12):1627–1629. https://doi.org/10.1111/j.1464-410X.2010.09389.x
Moe O, Pearle M, Sakhaee K (2011) Pharmacotherapy of urolithiasis: evidence from clinical trials. Kidney Int 79(4):385–392. https://doi.org/10.1038/ki.2010.389
Alvarez-Nemegyei J, Medina-Escobedo M, Villanueva-Jorge S, Vazquez-Mellado J (2005) Prevalence and risk factors for urolithiasis in primary gout: is a reappraisal needed? J Rheumatol 32(11):2189–2191
Shimizu T, Kitada H, Umeyama M, Hori H, Takasaki N (2013) Novel evaluation of nephrolithiasis as a complication of gout: a cross-sectional study using helical computerized tomography. J Urol 189(5):1747–1752. https://doi.org/10.1016/j.juro.2012.11.076
Ma Q, Fang L, Su R, Ma L, Xie G, Cheng Y (2018) Uric acid stones, clinical manifestations and therapeutic considerations. Postgrad Med J 94(1114):458–462. https://doi.org/10.1136/postgradmedj-2017-135332
Liu R, Han C, Wu D, Xia X, Gu J, Guan H, Shan Z, Teng W (2015) Prevalence of hyperuricemia and gout in mainland China from 2000 to 2014: a systematic review and meta-analysis. BioMed Res Int. https://doi.org/10.1155/2015/762820
Kamphuis G, Wouter van Hattum J, de Bie P, Somani B (2019) Method of alkalization and monitoring of urinary pH for prevention of recurrent uric acid urolithiasis a systematic review. Transl Androl Urol. https://doi.org/10.21037/tau.2019.05.01
Smith RC, Gore JZ, Mckee M, Hargis H (1988) The first dissociation constant of uric acid. Microchem J 38(1):118–124
Souma T, Abe M, Moriguchi T, Takai J, Yanagisawa-Miyazawa N, Shibata E, Akiyama Y, Toyohara T, Suzuki T, Tanemoto M, Abe T, Sato H, Yamamoto M, Ito S (2011) Luminal alkalinization attenuates proteinuria-induced oxidative damage in proximal tubular cells. J Am Soc Nephrol 22(4):635–648. https://doi.org/10.1681/asn.2009111130
Elsawy A, Elshal A, El-Nahas A, Elbaset M, Farag H, Shokeir A (2019) Can We predict the outcome of oral dissolution therapy for radiolucent renal calculi? A prospective study. J Urol 201(2):350–357. https://doi.org/10.1016/j.juro.2018.09.027
Gridley C, Sourial M, Lehman A, Knudsen B (2019) Medical dissolution therapy for the treatment of uric acid nephrolithiasis. World J Urol 37(11):2509–2515. https://doi.org/10.1007/s00345-019-02688-9
Tsaturyan A, Bokova E, Bosshard P, Bonny O, Fuster D, Roth B (2020) Oral chemolysis is an effective, non-invasive therapy for urinary stones suspected of uric acid content. Urolithiasis 48(6):501–507. https://doi.org/10.1007/s00240-020-01204-8
Elbaset M, Hashem A, Eraky A, Badawy M, El-Assmy A, Sheir K, Shokeir A (2020) Optimal non-invasive treatment of 1–2.5 cm radiolucent renal stones: oral dissolution therapy, shock wave lithotripsy or combined treatment-a randomized controlled trial. World J Urol 38(1):207–212. https://doi.org/10.1007/s00345-019-02746-2
Türk C, Petřík A, Sarica K, Seitz C, Skolarikos A, Straub M, Knoll T (2016) EAU guidelines on interventional treatment for urolithiasis. Eur Urol 69(3):475–482. https://doi.org/10.1016/j.eururo.2015.07.041
Taguchi K, Cho S, Ng A, Usawachintachit M, Tan Y, Deng Y, Shen C, Gyawali P, Alenezi H, Basiri A, Bou S, Djojodemedjo T, Sarica K, Shi L, Singam P, Singh S, Yasui T (2019) The urological association of Asia clinical guideline for urinary stone disease. Int J Urol Off J Japn Urol Assoc 26(7):688–709. https://doi.org/10.1111/iju.13957
Hui M, Carr A, Cameron S, Davenport G, Doherty M, Forrester H, Jenkins W, Jordan K, Mallen C, McDonald T, Nuki G, Pywell A, Zhang W, Roddy E (2017) The British society for rheumatology guideline for the management of gout. Rheumatology (Oxford) 56(7):e1–e20. https://doi.org/10.1093/rheumatology/kex156
FitzGerald J, Dalbeth N, Mikuls T, Brignardello-Petersen R, Guyatt G, Abeles A, Gelber A, Harrold L, Khanna D, King C, Levy G, Libbey C, Mount D, Pillinger M, Rosenthal A, Singh J, Sims J, Smith B, Wenger N, Bae S, Danve A, Khanna P, Kim S, Lenert A, Poon S, Qasim A, Sehra S, Sharma T, Toprover M, Turgunbaev M, Zeng L, Zhang M, Turner A, Neogi T (2020) 2020 American college of rheumatology guideline for the management of gout. Arthritis rheumatology (Hoboken, N.J.) 72(6):879–895. https://doi.org/10.1002/art.41247
Melamed M, Horwitz E, Dobre M, Abramowitz M, Zhang L, Lo Y, Mitch W, Hostetter T (2020) Effects of sodium bicarbonate in CKD stages 3 and 4: A randomized, placebo-controlled, multicenter clinical trial. Am J Kidney Dis 75(2):225–234. https://doi.org/10.1053/j.ajkd.2019.07.016
Pearle M, Goldfarb D, Assimos D, Curhan G, Denu-Ciocca C, Matlaga B, Monga M, Penniston K, Preminger G, Turk T, White J (2014) Medical management of kidney stones: AUA guideline. J Urol 192(2):316–324. https://doi.org/10.1016/j.juro.2014.05.006
Fontenelle L, Sarti T (2019) Kidney stones: treatment and prevention. Am Fam Physician 99(8):490–496
Cameron M, Maalouf N, Poindexter J, Adams-Huet B, Sakhaee K, Moe O (2012) The diurnal variation in urine acidification differs between normal individuals and uric acid stone formers. Kidney Int 81(11):1123–1130. https://doi.org/10.1038/ki.2011.480
Costello H, Johnston J, Juffre A, Crislip G, Gumz M (2022) Circadian clocks of the kidney: function, mechanism, and regulation. Physiol Rev 102(4):1669–1701. https://doi.org/10.1152/physrev.00045.2021
De Lavallaz L, Musso C (2018) Chronobiology in nephrology: the influence of circadian rhythms on renal handling of drugs and renal disease treatment. Int Urol Nephrol 50(12):2221–2228. https://doi.org/10.1007/s11255-018-2001-z
Yu K, Chen D, Chen J, Chen S, Chen S, Cheng T, Hsieh S, Hsieh T, Hsu P, Kuo C, Kuo M, Lam H, Lee I, Liang T, Lin H, Lin S, Tsai W, Tsay G, Wei J, Yang C, Tsai W (2018) Management of gout and hyperuricemia: multidisciplinary consensus in Taiwan. Int J Rheum Dis 21(4):772–787. https://doi.org/10.1111/1756-185x.13266
Chinese Society of Endocrinology, Association CM (2020) Guideline for the diagnosis and management of hyperuricemia and gout in China. Chin J Endocrinol Metab 36:1–13
Firsov D, Bonny O (2010) Circadian regulation of renal function. Kidney Int 78(7):640–645. https://doi.org/10.1038/ki.2010.227
Cameron M, Baker L, Maalouf N, Moe O, Sakhaee K (2007) Circadian variation in urine pH and uric acid nephrolithiasis risk. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc Eur Ren Assoc 22(8):2375–2378. https://doi.org/10.1093/ndt/gfm250
Kanbara A, Miura Y, Hyogo H, Chayama K, Seyama I (2012) Effect of urine pH changed by dietary intervention on uric acid clearance mechanism of pH-dependent excretion of urinary uric acid. Nutr J 11:39. https://doi.org/10.1186/1475-2891-11-39
Rebholz C, Coresh J, Grams M, Steffen L, Anderson C, Appel L, Crews D (2015) Dietary acid load and incident chronic kidney disease: results from the ARIC Study. Am J Nephrol 42(6):427–435. https://doi.org/10.1159/000443746
Welch A, Mulligan A, Bingham S, Khaw K (2008) Urine pH is an indicator of dietary acid-base load, fruit and vegetables and meat intakes: results from the European Prospective Investigation into Cancer and Nutrition (EPIC)-Norfolk population study. Br J Nutr 99(6):1335–1343. https://doi.org/10.1017/s0007114507862350
Wang S, Lay S, Yu H, Shen S (2016) Dietary guidelines for Chinese residents (2016): comments and comparisons. J Zhejiang Univ Sci B 17(9):649–656. https://doi.org/10.1631/jzus.B1600341
Acknowledgements
The authors would like to thank the patients for their participation. In addition, the authors wish to thank the National Natural Science Foundation of China for providing the financial support for this study.
Funding
This study was funded by the National Natural Science Foundation of China (No. 81970756) and Shanghai Tenth People’s Hospital of Tongji University (Nos. 040120069 and 040319136).
Author information
Authors and Affiliations
Contributions
WX: manuscript preparation and project development. JZ: manuscript preparation and data statistical analysis. LW: patient inclusion and management. AP: project development and study design. JC: study design and manuscript preparation. XL: project development and study design.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no financial competing interests.
Ethical approval
All procedures conducted in studies with participants involved complied with the 1964 Helsinki declaration and its later comparable or amendments ethical standards, and with the ethical standards of Shanghai Tenth People’s Hospital (Ethics Approval No. SHSY-IEC-4.1/20-4/01).
Consent to participate
All study participants provided informed consent before enrollment.
Consent to publication
Patients signed informed consent regarding publishing the study data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xue, W., Cheng, J., Zhao, J. et al. Comparison potassium sodium hydrogen citrate with sodium bicarbonate in urine alkalization: a prospective crossover-controlled trial. Int Urol Nephrol 55, 61–68 (2023). https://doi.org/10.1007/s11255-022-03387-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-022-03387-y