Abstract
Purpose
In our study, diagnostic and demographic characteristics of patients diagnosed with minimal change disease (MCD) by biopsy, clinical and laboratory findings in our country were investigated.
Methods
Data were obtained from the Turkish Society of Nephrology Glomerular Diseases (TSN-GOLD) Working Group database. Demographic characteristics, indications for biopsy, diagnosis of the glomerular diseases, comorbidities, laboratory and biopsy findings of all patients were recorded. The data presented are cross-sectional and includes application data for the biopsy period.
Results
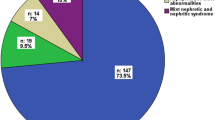
Of 3875 patients, 233 patients with MCD (median age 35.0 years) were included in the study, which constitutes 6.0% of the total glomerulonephritis database. Renal biopsy was performed in 196 (84.1%) patients due to nephrotic syndrome. Median serum creatinine was 0.7 (0.6–1.0) mg/dl, mean eGFR was 104 ± 33 ml/min/1.73 m2 and median proteinuria 6000 mg/day. The number of patients under the age of 40 years was 139 (59.7%) (Group A), and the number of patients aged 40 years and over was 94 (40.3%) (Group B). Compared to Group A, global sclerotic glomeruli (24 vs. 43, p < 0.001) interstitial inflammation (15 vs. 34, p < 0.001), interstitial fibrosis (20 vs. 31, p = 0.001, vascular changes (10 vs. 25, p < 0.001) and tubular atrophy (18 vs. 30, p < 0.001) were found to be significantly higher in Group B. There was no difference in immunofluorescent staining properties between the two groups.
Conclusion
Our data are generally compatible with the literature. Chronic histopathological changes were more common in patients aged 40 years and older than younger patients. Studies investigating the effects of these different features on renal survival are needed.

Similar content being viewed by others
Availability of data and materials
All data and materials are registered at the Turkish Society of Nephrology Glomerular Diseases Working Group (TSN-GOLD) website (http://pgh.tsn.org.tr). All data generated or analyzed during this study are included in this published article.
References
Stefan G, Busuioc R, Stancu S, Hoinoiu M, Zugravu A, Petre N et al (2021) Adult-onset minimal change disease: the significance of histological chronic changes for clinical presentation and outcome. Clin Exp Nephrol 25(3):240–250. https://doi.org/10.1007/s10157-020-01985-7
Vivarelli M, Massella L, Ruggiero B, Emma F (2017) Minimal change disease. Clin J Am Soc Nephrol 12(2):332–345. https://doi.org/10.2215/CJN.05000516
Fogo A, Hawkins EP, Berry PL, Glick AD, Chiang ML, MacDonell RC Jr et al (1990) Glomerular hypertrophy in minimal change disease predicts subsequent progression to focal glomerular sclerosis. Kidney Int 38:115–123. https://doi.org/10.1038/ki.1990.175
Shirato I (2002) Podocyte process effacement in vivo. Microsc Res Tech 57:241–246. https://doi.org/10.1002/jemt.10082
Fiorentino M, Bolignano D, Tesar V, Pisano A, Van Biesen W, D’Arrigo G, ERA-EDTA Immunonephrology Working Group et al (2016) Renal biopsy in 2015—from epidemiology to evidence-based indications. Am J Nephrol 43(1):1–19. https://doi.org/10.1159/000444026
Turkmen A, Sumnu A, Cebeci E, Yazici H, Eren N, Seyahi N et al (2020) Epidemiological features of primary glomerular disease in Turkey: a multicenter study by the Turkish Society of Nephrology Glomerular Diseases Working Group. BMC Nephrol 21(1):481. https://doi.org/10.1186/s12882-020-02134-8
Aydin Z, Turkmen K, Dede F, Yasar E, Ozturk S, Aydin M et al (2021) Demographic, clinical and laboratory characteristics of rapidly progressive glomerulonephritis in Turkey: Turkish Society of Nephrology-Glomerular Diseases (TSN-GOLD) Working Group. Clin Exp Nephrol 25(2):173–183. https://doi.org/10.1007/s10157-020-01978-6
Ozturk S, Sumnu A, Seyahi N, Gullulu M, Sipahioglu M, Artan S et al (2014) Demographic and clinical characteristics of primary glomerular diseases in Turkey. Int Urol Nephrol 46:2347–2355. https://doi.org/10.1007/s11255-014-0838-3
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF III, Feldman HI, CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612. https://doi.org/10.7326/0003-4819-150-9-200905050-00006
Panzer SE, Laskowski J, Renner B, Kulik L, Ljubanovic D, Huber KM et al (2015) IgM exacerbates glomerular disease progression in complement-induced glomerulopathy. Kidney Int 88(3):528–537. https://doi.org/10.1038/ki.2015.120
Malafronte P, Mastroianni-Kirsztajn G, Betônico GN, Romão JE Jr, Alves MA, Carvalho MF et al (2006) Paulista registry of glomerulonephritis: 5-year data report. Nephrol Dial Transplant 21:3098–3105. https://doi.org/10.1093/ndt/gfl237
Li LS, Liu ZH (2004) Epidemiologic data of renal diseases from a single unit in China: analysis based on 13,519 renal biopsies. Kidney Int 66(3):920–923. https://doi.org/10.1111/j.1523-1755.2004.00837.x
Waldman M, Crew RJ, Valeri A, Busch J, Stokes B, Markowitz G et al (2007) Adult minimal-change disease: clinical characteristics, treatment, and outcomes. Clin J Am Soc Nephrol 2(3):445–453. https://doi.org/10.2215/CJN.03531006
Huang JJ, Hsu SC, Chen FF, Sung JM, Tseng CC, Wang MC (2001) Adult-onset minimal change disease among Taiwanese: clinical features, therapeutic response, and prognosis. Am J Nephrol 21(1):28–34. https://doi.org/10.1159/000046215
Mak SK, Short CD, Mallick NP (1996) Long-term outcome of adult-onset minimal-change nephropathy. Nephrol Dial Transplant 11(11):2192–2201. https://doi.org/10.1093/oxfordjournals.ndt.a027136
Nolasco F, Cameron JS, Heywood EF, Hicks J, Ogg C, Williams DG (1986) Adult-onset minimal change nephrotic syndrome: a long-term follow-up. Kidney Int 29(6):1215–1223. https://doi.org/10.1038/ki.1986.130
Tse KC, Lam MF, Yip PS, Li FK, Choy BY, Lai KN et al (2003) Idiopathic minimal change nephrotic syndrome in older adults: steroid responsiveness and pattern of relapses. Nephrol Dial Transplant 18(7):1316–1320. https://doi.org/10.1093/ndt/gfg134
Nakayama M, Katafuchi R, Yanase T, Ikeda K, Tanaka H, Fujimi S (2002) Steroid responsiveness and frequency of relapse in adult-onset minimal change nephrotic syndrome. Am J Kidney Dis 39(3):503–512. https://doi.org/10.1053/ajkd.2002.31400
Acknowledgements
We would like to express our endless thanks to the Turkish Society of Nephrology, who organized the background of the study, and to the pathologists in each center for their contributions to patient care and their help in providing these data.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. All authors contributed to study material preparation, data collection. Analysis; Zeki Aydin, Murvet Yilmaz. The first draft of the manuscript was written by Zeki Aydin and Garip Sahin. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that no conflict of interest exists.
Ethics approval and consent to participate
The present study was approved by the Ethical Committee of the Istanbul Medical Faculty of Istanbul University. Informed consent was obtained from all individual participants included in the study. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee at which the studies were conducted (IRB approval number 1164/2011) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent for publish
All authors declare that they give consent for publication. This manuscript does not contain any information/images that could identify the participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Aydin, Z., Yilmaz, M., Sipahioglu, M. et al. Demographic, clinical and laboratory characteristics of adult-onset minimal change disease in Turkey: Turkish Society of Nephrology-Glomerular Diseases (TSN-GOLD) Working Group. Int Urol Nephrol 55, 975–982 (2023). https://doi.org/10.1007/s11255-022-03382-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-022-03382-3