Abstract
Purpose
To evaluate whether bladder wall thickness (BWT) measured by CT can be used to predict bladder outlet obstruction in men with low urinary tract symptoms (LUTS).
Methods
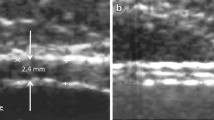
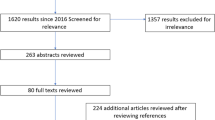
From 2015 to 2018, a total of 120 men with lower urinary tract symptoms who underwent both urodynamic studies and CT tests of the lower abdomen or pelvis were involved. Bladder wall thickness values were measured by CT scanning.
Results
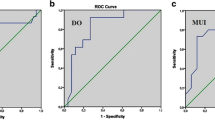
Based on the urodynamic studies, 120 men were categorized into two groups, including 70/120 men (58.3%) in the bladder outlet obstruction (BOO) group and 50/120 men (41.7%) in the non-BOO group. The mean BWT was thicker in the BOO group than in the non-BOO group (3.87 vs. 2.75 mm, p < 0.001). The mean maximum bladder capacity (MBC) was lower in the BOO group than in the non-BOO group (263.42 vs. 308.96 ml, p < 0.001). The mean detrusor pressure at maximum urinary flow rate (PdetQmax) was higher in the patients in the BOO group than in those in the non-BOO group (102.28 vs. 49.25 cmH2O, p < 0.001). The ROC curve showed that BWT was a good predictor with an AUC of 0.855 (95% CI 0.785–0.924, p < 0.001). At the cutoff value of 3.20 mm, the predictive sensitivity of BWT for BOO was 72.9%, and the specificity was 90%.
Conclusion
Increased bladder wall thickness was correlated with bladder outlet obstruction in men with LUTS. Bladder wall thickness measured by CT scans may be a noninvasive parameter to predict bladder outlet obstruction in men with LUTS.


Similar content being viewed by others
Availability of data and materials
The datasets used and analyzed during the current study are not publicly available due to the relevant data protection law but are available from the corresponding author on reasonable request. Data used in the present study were original medical records in Peking University People's Hospital. To access/use the original medical records, you would need administrative proposal consent for publication.
Abbreviations
- AUC:
-
Area under the curve
- BOO:
-
Bladder outlet obstruction
- BOOI:
-
BOO index
- BPH:
-
Benign prostatic hyperplasia
- BWT:
-
Bladder wall thickness
- CI:
-
Confidence interval
- CT:
-
Computed tomography
- DWT:
-
Detrusor wall thickness
- IPP:
-
Intravesical prostatic protrusion
- LUTs:
-
Lower urinary tract symptom
- MBC:
-
Maximum bladder capacity
- PdetQmax:
-
Detrusor pressure at maximum urinary flow rate
- PV:
-
Prostate volume
- PVR:
-
Postvoid residual urine volume
- Qmax:
-
Maximum urinary flow rate
- ROC:
-
Receiver operating characteristic
- SMCs:
-
Smooth muscle cells
- UDS:
-
Urodynamic studies
References
Patel ND, Parsons JK (2014) Epidemiology and etiology of benign prostatic hyperplasia and bladder outlet obstruction. Indian J Urol 30(2):170–176
Zhang W, Zhang X, Li H, Wu F, Wang H, Zhao M, Hu H, Xu K (2019) Prevalence of lower urinary tract symptoms suggestive of benign prostatic hyperplasia (LUTS/BPH) in China: results from the China Health and Retirement Longitudinal Study. BMJ Open 9(6):e022792
Gratzke C, Bachmann A, Descazeaud A, Drake MJ, Madersbacher S, Mamoulakis C, Oelke M, Tikkinen KAO, Gravas S (2015) EAU guidelines on the assessment of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol 67(6):1099–1109
Harding C, Robson W, Drinnan M, McIntosh S, Sajeel M, Giffiths C, Pickard R (2009) The penile cuff test: a clinically useful non-invasive urodynamic investigation to diagnose men with lower urinary tract symptoms. Indian J Urol IJU J Urol Soc India 25(1):116–121
Ghoniem GM, Regnier CH, Biancani P, Johnson L, Susset JG (1986) Effect of vesical outlet obstruction on detrusor contractility and passive properties in rabbits. J Urol 135(6):1284–1289
Fusco F, Creta M, De Nunzio C, Iacovelli V, Mangiapia F, Li Marzi V, Finazzi Agrò E (2018) Progressive bladder remodeling due to bladder outlet obstruction: a systematic review of morphological and molecular evidences in humans. BMC Urol 18(1):15
Niemczyk G, Czarzasta K, Radziszewski P, Włodarski P, Cudnoch-Jędrzejewska A (2018) Pathophysiological effect of bladder outlet obstruction on the urothelium. Ultrastruct Pathol 42(3):317–322
Park J, Suh J, Yoo S, Cho MC, Son H (2020) Bladder wall thickness and detrusor wall thickness can help to predict the bladder outlet obstruction in men over the age of 70 years with symptomatic benign prostatic hyperplasia. Investig Clin Urol 61(5):491–497
Güzel Ö, Aslan Y, Balcı M, Tuncel A, Keten T, Erkan A, Atan A (2015) Can bladder wall thickness measurement be used for detecting bladder outlet obstruction? Urology 86(3):439–444
Khullar V, Salvatore S, Cardozo L, Bourne TH, Abbott D, Kelleher C (1994) A novel technique for measuring bladder wall thickness in women using transvaginal ultrasound. Ultrasound Obstet Gynecol 4(3):220–223
Chung SD, Chiu B, Kuo HC, Chuang YC, Wang CC, Guan Z, Chancellor MB (2010) Transabdominal ultrasonography of detrusor wall thickness in women with overactive bladder. BJU Int 105(5):668–672
Fananapazir G, Kitich A, Lamba R, Stewart SL, Corwin MT (2018) Normal reference values for bladder wall thickness on CT in a healthy population. Abdom Radiol (NY) 43(9):2442–2445
Reddy SVK, Shaik AB (2019) Non-invasive evaluation of bladder outlet obstruction in benign prostatic hyperplasia: a clinical correlation study. Arab J Urol 17(4):259–264
Mangat R, Ho HSS, Kuo TLC (2018) Non-invasive evaluation of lower urinary tract symptoms (LUTS) in men. Asian J Urol 5(1):42–47
Oelke M, Höfner K, Jonas U, de la Rosette JJ, Ubbink DT, Wijkstra H (2007) Diagnostic accuracy of noninvasive tests to evaluate bladder outlet obstruction in men: detrusor wall thickness, uroflowmetry, postvoid residual urine, and prostate volume. Eur Urol 52(3):827–834
Bright E, Oelke M, Tubaro A, Abrams P (2010) Ultrasound estimated bladder weight and measurement of bladder wall thickness–useful noninvasive methods for assessing the lower urinary tract? J Urol 184(5):1847–1854
Gosling JA, Kung LS, Dixon JS, Horan P, Whitbeck C, Levin RM (2000) Correlation between the structure and function of the rabbit urinary bladder following partial outlet obstruction. J Urol 163(4):1349–1356
Tubaro A, Carter S, Hind A, Vicentini C, Miano L (2001) A prospective study of the safety and efficacy of suprapubic transvesical prostatectomy in patients with benign prostatic hyperplasia. J Urol 166(1):172–176
Sironi D, Levorato CA, Deiana G, Borgonovo G, Belussi D, Ranieri A, Lembo A (2002) Decrease of ultrasound estimated bladder weight during tamsulosin treatment in patients with benign prostatic enlargement. Archivio Italiano Di Urologia, Andrologia: Organo Ufficiale [di] Societa Italiana Di Ecografia Urologica E Nefrologica 74(2):90–94
Garg G, Sankhwar SN, Goel A, Pandey S, Sharma D, Parihar A (2019) Evaluation of resistive index of the prostate and bladder sonomorphologic parameters as replacements for urodynamics to predict bladder outlet obstruction in patients with lower urinary tract symptoms suggestive of benign prostatic hyperplasia. Low Urin Tract Symptoms 11(3):163–168
Farag F, Elbadry M, Saber M, Badawy AA, Heesakkers J (2017) A novel algorithm for the non-invasive detection of bladder outlet obstruction in men with lower urinary tract symptoms. Arab J Urol 15(2):153–158
Gordon MN, Hadjiiski LM, Cha KH, Samala RK, Chan HP, Cohan RH, Caoili EM (2019) Deep-learning convolutional neural network: Inner and outer bladder wall segmentation in CT urography. Med Phys 46(2):634–648
Ahmed AF, Bedewi M (2016) Can bladder and prostate sonomorphology be used for detecting bladder outlet obstruction in patients with symptomatic benign prostatic hyperplasia? Urology 98:126–131
Acknowledgements
We gratefully acknowledge Mr. Jingwen Chen and Mr. Yiran Sun in the Department of Urology to have performed all of the urodynamic tests in the past ten years in our center.
Funding
Funding was provided by National Natural Science Foundation of China (grant no. 81970660) with Kexin Xu as the recipient and Peking University People’s Hospital Research and Development Fund (grant no. RDY2021-16) with Huanrui Wang as the recipient.
Author information
Authors and Affiliations
Contributions
ZD wrote the main manuscript, collected the data and analyzed the data; HW developed the project and got data acquisition, data analysis and data interpretation; KX got project development, data interpretation, manuscript writing; WZ got project development, data acquisition, data analysis, data interpretation; HH got project development, data interpretation; QW got project development, data interpretation; All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval
The study was conducted in accordance with the Declaration of Helsinki. The study did not require an ethical board approval because it was waived by Ethics Committee of Peking University Peoples Hospital because of the nature of retrospective study in line with international ethics norms.
Consent for publication
Not applicable.
Consent to participate
No informed consent was required, because the data are anonymized and the informed consent was waived by Ethics Committee of Peking University Peoples Hospital because of the nature of retrospective study in line with international ethics norms.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ding, Z., Wang, H., Zhang, W. et al. Bladder wall thickness measured by CT can predict bladder outlet obstruction in men: a retrospective cohort study. Int Urol Nephrol 55, 43–49 (2023). https://doi.org/10.1007/s11255-022-03361-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-022-03361-8