Abstract
Purpose
Testicular cancer is frequently seen, especially in young males, and constitutes 1% of all male cancers. Family history, testicular dysgenesis syndrome, and the presence of tumour in the contralateral testis are each well-defined epidemiological risk factors. The aim of the current study was to determine the distribution of these risk factors according to tumour stage and to evaluate the effects on progression.
Materials and methods
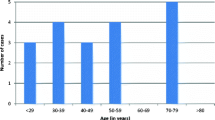
A total of 71 patients diagnosed with testicular cancer in our clinic between January 2018 and December 2021 were classified according to tumour stage (Group 1: Early, n = 29; Group 2: Advanced, n = 42). The presence of risk factors, and demographic and pathological data were recorded.
Results
No significant difference was determined between the groups in respect of age, comorbidities, and tumour type (p > 0.05). There was no difference between Group 1 and Group 2 in terms of median follow-up time [15.5 (17.5), 16.5(26.5) months, respectively, p = 0.4]. Epidemiological risk factors were seen more in Group 2 than in Group 1 (p = 0.03). Progression-free survival was determined to be shorter in patients with risk factors compared to those without (7.95 ± 1.3 vs. 29.4 ± 2.06 months, p < 0.001, respectively). Family history and testicular dysgenesis syndrome were determined to be independent risk factors for progression [HR:0.046 (0.004–0.485); HR:0.101 (0.03–0.347), p < 0.05, respectively].
Conclusions
More advanced-stage tumours are seen in patients with testicular cancer when epidemiological risk factors are also present. Of these risk factors, family history and testicular dysgenesis syndrome have a negative effect on progression.




Similar content being viewed by others
References
Del Risco KR, Ruud E et al (2019) Family history of cancer and risk of paediatric and young adult’s testicular cancer: a Norwegian cohort study. Br J Cancer 120(10):1007–1014
IARC (2021) Cancer Today. Estimated number of new cases in 2020, worldwide, both sexes, all ages.2021 , Accessed March 2021
Etter JL, Eng K, Cannioto R et al (2018) Hereditary association between testicular cancer and familial ovarian cancer: a familial ovarian cancer registry study. Cancer Epidemiol 53:184–186. https://doi.org/10.1016/j.canep.2018.02.005
Low ZY, Yan A, Arul D et al (2019) Metachronous bilateral testicular cancer: case reports and review of literature. Urologia 86(4):220–224
Xing JS, Bai ZM (2018) Is testicular dysgenesis syndrome a genetic, endocrine, or environmental disease, or an unexplained reproductive disorder? Life Sci 1(194):120–129
de Melo AC (2020) Editorial comment: effects of testicular dysgenesis syndrome componentes on testicular germ cell tumor prognosis and oncological outcomes. Int Braz J Urol 46(5):741–742
Albers P, Albrecht W, Algaba F, Bokemeyer C, Cohn-Cedermark G, Fizazi K et al (2015) Guidelines on testicular cancer: 2015 update. Eur Urol 68:1054–1068
Park JS, Kim J, Elghiaty A, Ham WS (2018) Recent global trends in testicular cancer incidence and mortality. Medicine (Baltimore) 97(37):e12390. https://doi.org/10.1097/MD.0000000000012390 (PMID: 30213007; PMCID: PMC6155960)
Gillessen S, Sauvé N, Collette L et al (2021) Predicting outcomes in men with metastatic nonseminomatous germ cell tumors (NSGCT): results from the IGCCCG update consortium. J Clin Oncol 39(14):1563–1574
Gandaglia G, Leni R, Bray F, Fleshner N, Freedland SJ, Kibel A, Stattin P, Van Poppel H, La Vecchia C (2021) Epidemiology and prevention of prostate cancer. Eur Urol Oncol 4(6):877–892. https://doi.org/10.1016/j.euo.2021.09.006 (Epub 2021 Oct 26 PMID: 34716119)
Spiller CM, Bowles J (2017) Germ cell neoplasia in situ: the precursor cell for invasive germ cell tumors of the testis. Int J Biochem Cell Biol 86:22–25
Kharazmi E, Hemminki K, Pukkala E et al (2015) Cancer risk in relatives of testicular cancer patients by histology type and age at diagnosis: a joint study from five nordic countries. Eur Urol 68(2):283–289
Loveday C, Law P, Litchfield K et al (2018) Large-scale analysis demonstrates familial testicular cancer to have polygenic aetiology. Eur Urol 74(3):248–252. https://doi.org/10.1016/j.eururo.2018.05.036
Kollerud R, Ruud E, Haugnes HS, Cannon-Albright LA, Thoresen M, Nafstad P, Vlatkovic L, Blaasaas KG, Næss Ø, Claussen B (2019) Family history of cancer and risk of paediatric and young adult’s testicular cancer: a Norwegian cohort study. Br J Cancer 120(10):1007–1014. https://doi.org/10.1038/s41416-019-0445-2 (Epub 2019 Apr 10. PMID: 30967648; PMCID: PMC6734662)
Maroto P, Muro XG, Valverde C et al (2021) Spanish germ cell cancer group incidence and clinical pattern of contralateral synchronous and metachronous germ cell testicular cancer. Urol Oncol 39(2):135.e17-135.e23
Hellesnes R, Myklebust TÅ, Bremnes RM, Karlsdottir Á, Kvammen Ø, Negaard HFS, Tandstad T, Wilsgaard T, Fosså SD, Haugnes HS (2021) Metachronous contralateral testicular cancer in the cisplatin era: a population-based cohort study. J Clin Oncol 39(4):308–318. https://doi.org/10.1200/JCO.20.02713 (Epub 2020 Dec 23 PMID: 33356420)
Akdogan B, Divrik RT, Tombul T, Yazici S, Tasar C, Zorlu F, Ozen H (2007) Bilateral testicular germ cell tumors in Turkey: increase in incidence in last decade and evaluation of risk factors in 30 patients. J Urol 178(1):129–133. https://doi.org/10.1016/j.juro.2007.03.027 (Epub 2007 May 17. Erratum in: J Urol. 2007 Sep;178(3 Pt 1):1125. Bulent, Akdogan [corrected to Akdogan, Bulent]; Taner, Divrik Rauf [corrected to Divrik, Rauf Taner]; Tolga, Tombul [corrected to Tombul, Tolga]; Sertac, Yazici [corrected to Yazici, Sertac]; Celik, Tasar [corrected to Tasar, Celik]; Ferruh, Zorlu [correct. PMID: 17499297.)
Osterlind A, Berthelsen JG, Abildgaard N, Hansen SO, Hjalgrim H, Johansen B, Munck-Hansen J, Rasmussen LH (1991) Risk of bilateral testicular germ cell cancer in Denmark: 1960–1984. J Natl Cancer Inst 83(19):1391–1395. https://doi.org/10.1093/jnci/83.19.1391 (PMID: 1656057)
Che M, Tamboli P, Ro JY, Park DS, Ro JS, Amato RJ, Ayala AG (2002) Bilateral testicular germ cell tumors: twenty-year experience at M. D Anderson Cancer Center Cancer 95(6):1228–1233. https://doi.org/10.1002/cncr.10804 (PMID: 12216089)
Holzbeierlein JM, Sogani PC, Sheinfeld J (2003) Histology and clinical outcomes in patients with bilateral testicular germ cell tumors: the Memorial Sloan Kettering Cancer Center experience 1950 to 2001. J Urol 169(6):2122–2125. https://doi.org/10.1097/01.ju.0000067462.24562.8b (PMID: 12771732)
Campobasso D, Ferretti S, Frattini A (2017) Synchronous bilateral testis cancer: clinical and oncological management. Contemp Oncol (Pozn) 21(1):70–76. https://doi.org/10.5114/wo.2017.66660
Pedersen MR, Rafaelsen SR, Møller H et al (2016) Testicular microlithiasis and testicular cancer: review of the literature. Int Urol Nephrol 48:1079–1086
Dave S, Liu K, Clark R et al (2019) A retrospective population-based cohort study to evaluate the impact of an older sibling with undescended testis and hypospadias on the known maternal and fetal risk factors for undescended testis and hypospadias in Ontario, Canada, 1997–2007. J Pediatr Urol 15(1):41.e1-41.e9. https://doi.org/10.1016/j.jpurol.2018.09.021
Cao H, Wan Z, Wang F et al (2021) Downregulation of KIF2C and TEKT2 is associated with male infertility and testicular carcinoma. Aging (Albany NY) 13(19):22898–22911. https://doi.org/10.18632/aging.203583
Selvi I, Ozturk E, Yikilmaz TN, Sarikaya S, Basar H (2020) Effects of testicular dysgenesis syndrome components on testicular germ cell tumor prognosis and oncological outcomes. Int Braz J Urol 46(5):725–740. https://doi.org/10.1590/S1677-5538.IBJU.2019.0387 (PMID: 32648412; PMCID: PMC7822361)
Kliesch S, Schmidt S, Wilborn D et al (2021) Management of germ cell tumours of the testis in adult patients. German clinical practice guideline Part I: epidemiology, classification, diagnosis, prognosis, fertility preservation, and treatment recommendations for localized stages. Urol Int 105(3–4):169–180. https://doi.org/10.1159/000510407
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Demirci, A., Başar, H. Effects of epidemiological risk factors on prognosis in testicular cancer. Int Urol Nephrol 55, 51–59 (2023). https://doi.org/10.1007/s11255-022-03359-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-022-03359-2