Abstract
Background
Chronic kidney disease (CKD) patients have high levels of inflammatory mediators. These inflammatory mediators contribute to the increased risk of cardiovascular events and all-cause mortality. Platelet-lymphocyte ratio (PLR) has recently been recognized as a novel inflammatory marker and has been shown to be associated with the prognosis in CKD patients. However, the quality of these studies varies and their results are controversial. The purpose of this meta-analysis was to investigate the relationship between PLR and all-cause mortality in CKD patients.
Methods
A systematic literature search of PubMed, EMBASE, CENTRAL and ISI Web of Science was conducted. The databases were searched from their inception dates up to the latest issue (31 October 2021). Two reviewers independently searched the databases and screened studies. Data were extracted using a standardized collection form. Meta-analysis was performed to compare PLR values between CKD and non-CKD patients, and to investigate the association between PLR and all-cause mortality in CKD patients. This meta-analysis is reported in adherence to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).
Results
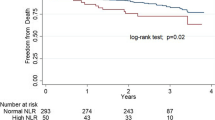
A total of 11 studies involving 4244 participants were selected. The pooled data indicated that PLR values were significantly higher in CKD patients than non-CKD controls (weighted mean difference = 21.6, 95% CI 17.39–25.81, p < 0.01), and PLR is associated with an increased risk of all-cause mortality in CKD patients (hazard ratio = 2.49, 95% CI 1.78–3.49, p < 0.01).
Conclusions
Patients with CKD have higher PLR values compared to non-CKD patients. Meanwhile, PLR values were highly associated with all-cause mortality in CKD patients. PLR is a valid predictor as a clinically accessible indicator for patients with CKD.




Similar content being viewed by others
References
Zhang L et al (2012) Prevalence of chronic kidney disease in China: a cross-sectional survey. Lancet 379:815–822. https://doi.org/10.1016/S0140-6736(12)60033-6
Coresh J et al (2007) Prevalence of chronic kidney disease in the United States. JAMA 298:2038–2047. https://doi.org/10.1001/jama.298.17.2038
Zhong J, Yang HC, Fogo AB (2017) A perspective on chronic kidney disease progression. Am J Physiol Renal Physiol 312:F375–F384. https://doi.org/10.1152/ajprenal.00266.2016
Kim H, Hong JY, Jeon WJ, Baek SH, Ha IH (2020) Bee venom melittin protects against cisplatin-induced acute kidney injury in mice via the regulation of M2 macrophage activation. Toxins (Basel). https://doi.org/10.3390/toxins12090574
Tang Y et al (2015) The protective mechanism of fluorofenidone in renal interstitial inflammation and fibrosis. Am J Med Sci 350:195–203. https://doi.org/10.1097/MAJ.0000000000000501
Podkowinska A, Formanowicz D (2020) Chronic kidney disease as oxidative stress- and inflammatory-mediated cardiovascular disease. Antioxidants (Basel). https://doi.org/10.3390/antiox9080752
Sarnak MJ et al (2019) Chronic kidney disease and coronary artery disease: JACC state-of-the-art review. J Am Coll Cardiol 74:1823–1838. https://doi.org/10.1016/j.jacc.2019.08.1017
Ermer T, Eckardt KU, Aronson PS, Knauf F (2016) Oxalate, inflammasome, and progression of kidney disease. Curr Opin Nephrol Hypertens 25:363–371. https://doi.org/10.1097/MNH.0000000000000229
Chen TK, Knicely DH, Grams ME (2019) Chronic kidney disease diagnosis and management: a review. JAMA 322:1294–1304. https://doi.org/10.1001/jama.2019.14745
Li WJ et al (2015) Cardiac troponin and C-reactive protein for predicting all-cause and cardiovascular mortality in patients with chronic kidney disease: a meta-analysis. Clinics (Sao Paulo) 70:301–311. https://doi.org/10.6061/clinics/2015(04)14
Goicoechea M et al (2012) Intraindividual interleukin-6 variations on the cardiovascular prognosis of patients with chronic renal disease. Ren Fail 34:1002–1009. https://doi.org/10.3109/0886022X.2012.696469
Walzik D, Joisten N, Zacher J, Zimmer P (2021) Transferring clinically established immune inflammation markers into exercise physiology: focus on neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio and systemic immune-inflammation index. Eur J Appl Physiol 121:1803–1814. https://doi.org/10.1007/s00421-021-04668-7
Gasparyan AY, Ayvazyan L, Mukanova U, Yessirkepov M, Kitas GD (2019) The platelet-to-lymphocyte ratio as an inflammatory marker in rheumatic diseases. Ann Lab Med 39:345–357. https://doi.org/10.3343/alm.2019.39.4.345
Kumarasamy C et al (2021) Prognostic utility of platelet-lymphocyte ratio, neutrophil-lymphocyte ratio and monocyte-lymphocyte ratio in head and neck cancers: a detailed PRISMA compliant systematic review and meta-analysis. Cancers (Basel). https://doi.org/10.3390/cancers13164166
Catanzaro R, Sciuto M, Lanzafame C, Balakrishnan B, Marotta F (2020) Platelet to lymphocyte ratio as a predictive biomarker of liver fibrosis (on elastography) in patients with hepatitis C virus (HCV)-related liver disease. Indian J Gastroenterol 39:253–260. https://doi.org/10.1007/s12664-020-01038-7
Sevencan NO, Ozkan AE (2019) Associations between neutrophil/lymphocyte ratio, platelet/lymphocyte ratio, albuminuria and uric acid and the estimated glomerular filtration rate in hypertensive patients with chronic kidney disease stages 1–3. Arch Med Sci 15:1232–1239. https://doi.org/10.5114/aoms.2018.76262
Zeng M et al (2020) J-shaped association of platelet-to-lymphocyte ratio with 5-year mortality among patients with chronic kidney disease in a prospective cohort study. Int Urol Nephrol 52:1943–1957. https://doi.org/10.1007/s11255-020-02548-1
Brito GMC et al (2021) Neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios in nondialysis chronic kidney patients. Int J Inflam 2021:6678960. https://doi.org/10.1155/2021/6678960
Toraman A, Aras F, Hekimsoy Z, Kursat S (2019) Is there a relationship between parathyroid hormone and neutrophil lymphocyte ratio or platelet lymphocyte ratio? Acta Endocrinol (Buchar) 5:96–101. https://doi.org/10.4183/aeb.2019.96
Stroup DF et al (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA 283:2008–2012. https://doi.org/10.1001/jama.283.15.2008
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25:603–605. https://doi.org/10.1007/s10654-010-9491-z
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560. https://doi.org/10.1136/bmj.327.7414.557
Noce A et al (2020) A pilot study of a natural food supplement as new possible therapeutic approach in chronic kidney disease patients. Pharmaceuticals (Basel). https://doi.org/10.3390/ph13070148
Ahbap E et al (2016) Serum uric acid levels and inflammatory markers with respect to dipping status: a retrospective analysis of hypertensive patients with or without chronic kidney disease. Clin Exp Hypertens 38:555–563. https://doi.org/10.3109/10641963.2016.1174251
Ozdemir A, Kocak SY, Karabela SN, Yilmaz M (2021) Can systemic immune inflammation index at admission predict in-hospital mortality in chronic kidney disease patients with SARS-CoV-2 infection. Nefrologia (Engl Ed). https://doi.org/10.1016/j.nefro.2021.09.001
Binnetoglu E, Sengul E, Halhalli G, Dindar S, Sen H (2014) Is neutrophil lymphocyte ratio an indicator for proteinuria in chronic kidney disease? J Clin Lab Anal 28:487–492. https://doi.org/10.1002/jcla.21715
Li Q et al (2020) Neutrophil-to-lymphocyte ratio as an independent inflammatory indicator of poor prognosis in IgA nephropathy. Int Immunopharmacol 87:106811. https://doi.org/10.1016/j.intimp.2020.106811
Tatar B, Kose S, Pala E, Tatar E (2017) Inflammatory biomarkers and liver histopathology in non-uremic and uremic chronic hepatitis C patients. Acta Medica (Hradec Kralove) 60:71–75. https://doi.org/10.14712/18059694.2017.96
Zhang J, Lu X, Wang S, Li H (2021) High neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio are associated with poor survival in patients with hemodialysis. Biomed Res Int 2021:9958081. https://doi.org/10.1155/2021/9958081
Yaprak M et al (2016) Platelet-to-lymphocyte ratio predicts mortality better than neutrophil-to-lymphocyte ratio in hemodialysis patients. Int Urol Nephrol 48:1343–1348. https://doi.org/10.1007/s11255-016-1301-4
Liu S et al (2021) Platelet-to-lymphocyte ratio is associated with the mortality in peritoneal dialysis patients. Iran J Kidney Dis 15:206–212
Kato A et al (2013) A comparison of systemic inflammation-based prognostic scores in patients on regular hemodialysis. Nephron Extra 3:91–100. https://doi.org/10.1159/000355148
National Kidney F (2012) KDOQI clinical practice guideline for diabetes and CKD: 2012 update. Am J Kidney Dis 60:850–886. https://doi.org/10.1053/j.ajkd.2012.07.005
Wise ME, Lovell C (2013) Public health surveillance in the dialysis setting: opportunities and challenges for using electronic health records. Semin Dial 26:399–406. https://doi.org/10.1111/sdi.12098
Kaplan ZS, Jackson SP (2011) The role of platelets in atherothrombosis. Hematology Am Soc Hematol Educ Program 51–61:2011. https://doi.org/10.1182/asheducation-2011.1.51
Ruggeri ZM (2009) Platelet adhesion under flow. Microcirculation 16:58–83. https://doi.org/10.1080/10739680802651477
Valga F, Monzon T, Henriquez F, Anton-Perez G (2019) Neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios as biological markers of interest in kidney disease. Nefrologia (Engl Ed) 39:243–249. https://doi.org/10.1016/j.nefro.2018.11.005
Hotchkiss RS, Karl IE (2003) The pathophysiology and treatment of sepsis. N Engl J Med 348:138–150. https://doi.org/10.1056/NEJMra021333
Dirnagl U et al (2007) Stroke-induced immunodepression: experimental evidence and clinical relevance. Stroke 38:770–773. https://doi.org/10.1161/01.STR.0000251441.89665.bc
Huang Z, Fu Z, Huang W, Huang K (2020) Prognostic value of neutrophil-to-lymphocyte ratio in sepsis: a meta-analysis. Am J Emerg Med 38:641–647. https://doi.org/10.1016/j.ajem.2019.10.023
Balta S et al (2016) The relation between atherosclerosis and the neutrophil-lymphocyte ratio. Clin Appl Thromb Hemost 22:405–411. https://doi.org/10.1177/1076029615569568
Diaz-Martinez J et al (2019) The relationship of blood neutrophil-to-lymphocyte ratio with nutrition markers and health outcomes in hemodialysis patients. Int Urol Nephrol 51:1239–1247. https://doi.org/10.1007/s11255-019-02166-6
Balboul Y et al (2020) Biological basis of lymphocyte ratios for survival prediction in hemodialysis patients: a longitudinal study. Int Urol Nephrol 52:1345–1356. https://doi.org/10.1007/s11255-020-02471-5
Acknowledgements
We thank all the medical, nursing, and technical staff from the Department of Nephrology, the Central Hospital of Wuhan.
Author information
Authors and Affiliations
Contributions
WG, QG and XH designed the study; XZ, DS and LX collected data; WC had given professional advices on the design and perform of this study; WG, QG, XH, WX and HM analyzed the data and made the figures; WG, QG and XH drafted the paper; WC revised the paper; all authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that they have no conflict of interest. The authors have no relevant financial or non-financial interests to disclose. This article does not contain any studies with human participants performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gan, W., Guan, Q., Hu, X. et al. The association between platelet-lymphocyte ratio and the risk of all-cause mortality in chronic kidney disease: a systematic review and meta-analysis. Int Urol Nephrol 54, 2959–2967 (2022). https://doi.org/10.1007/s11255-022-03234-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-022-03234-0