Abstract
Purpose
To evaluate urinary outcomes of pelvic construction and lateral capsule sparing techniques in robot-assisted radical cystectomy with orthotopic ileal neobladder (RARC-OIN).
Methods
A total of 107 male patients who underwent RARC-OIN during January 2017 and February 2021 in Sun Yat-sen Memorial Hospital were analyzed retrospectively. Standard RARC-OIN with or without nerve sparing technique was performed in 44 patients (standard group), lateral prostate capsule sparing technique was performed in 20 patients (LCS group), combined pelvic reconstruction (CPR) technique including anterior suspension and posterior reconstruction were performed in 43 patients (CPR group). The urinary function was assessed by the use of pads and the Bladder Cancer Index (BCI). Continence was defined as the use of 0–1 pad during daytime or night-time.
Results
There was no statistical difference between the three groups regarding demographic, perioperative, and pathological data. Continence rates were 6.8, 50.0 and 34.9% for daytime, 4.6, 40.0 and 32.6% for night-time in the standard group, LCS group and CPR group at 1 month post-operation, respectively. Continence rates were 34.1, 80.0 and 69.8% for daytime, 27.3, 75.0 and 65.1% for night-time in the standard group, LCS group and CPR group at 3 month post-operation, respectively. No statistically significant difference was observed in the daytime and night-time continence rates at 12 months.
Conclusions
Lateral capsule-sparing and combined pelvic reconstruction techniques are feasible to improve early daytime and night-time continence rates in RARC with orthotopic neobladder.
Clinical trial registration
The trial registration number: ChiCTR2100047606.

Similar content being viewed by others
References
Witjes JA et al (2021) European Association of Urology Guidelines on Muscle-invasive and Metastatic Bladder Cancer: Summary of the 2020 Guidelines. Eur Urol 79(1):82–104
Lee RK et al (2014) Urinary diversion after radical cystectomy for bladder cancer: options, patient selection, and outcomes. BJU Int 113(1):11–23
JA Nieuwenhuijzen et al. (2008) Urinary diversions after cystectomy: the association of clinical factors, complications and functional results of four different diversions. Eur Urol 53(4): 834–42
Singh V et al (2014) Prospective comparison of quality-of-life outcomes between ileal conduit urinary diversion and orthotopic neobladder reconstruction after radical cystectomy: a statistical model. BJU Int 113(5):726–732
Tostivint V. et al. (2021) Quality of life and functional outcomes after radical cystectomy with ileal orthotopic neobladder replacement for bladder cancer: a multicentre observational study. World J Urol 39(7):2525-2530.
Hautmann, R.E., et al. (2021) Functional outcome and complications following Ileal neobladder reconstruction in male patients without tumor recurrence More than 35 years of experience from a single center. J Urol 205(1): 174–182.
Hautmann RE et al (2006) Long-term results of standard procedures in urology: the ileal neobladder. World J Urol 24(3):305–314
Kulkarni JN et al (2003) Long-term results of orthotopic neobladder reconstruction after radical cystectomy. BJU Int 91(6):485–488
Clifford T et al (2016) Prospective evaluation of continence following radical cystectomy and orthotopic urinary diversion using a Validated Questionnaire. J Urol 196(6):1685–1691
Krhut J et al (2018) Effect of severity of urinary incontinence on quality of life in women. Neurourol Urodyn 37(6):1925–1930
Bernardes, M., et al. (2019) Impact of urinary incontinence on the quality of life of individuals undergoing radical prostatectomy. Rev Lat Am Enfermagem 27: e3131.
Saad M et al (2020) Long-term functional and oncological outcomes of nerve-sparing and prostate capsule-sparing cystectomy: a single-centre experience. BJU Int 125(2):253–259
Abdelaziz AY et al (2019) Early oncological and functional outcomes of prostate capsule sparing cystectomy compared with standard radical cystectomy. Curr Urol 13(1):37–45
R. S. Hollabaugh Jr, R.R. Dmochowski, and M.S. Steiner (1997) Neuroanatomy of the male rhabdosphincter. Urology, 49(3): 426–34.
Hollabaugh RS Jr et al (1998) Preservation of putative continence nerves during radical retropubic prostatectomy leads to more rapid return of urinary continence. Urology 51(6):960–967
Rocco B et al (2007) Posterior reconstruction of the rhabdosphincter allows a rapid recovery of continence after transperitoneal videolaparoscopic radical prostatectomy. Eur Urol 51(4):996–1003
Patel V et al (2009) Periurethral suspension stitch during robot-assisted laparoscopic radical prostatectomy: description of the technique and continence outcomes. Eur Urol 56(3):472–478
Hurtes X et al (2012) Anterior suspension combined with posterior reconstruction during robot-assisted laparoscopic prostatectomy improves early return of urinary continence: a prospective randomized multicentre trial. BJU Int 110(6):875–883
Vis A et al (2019) Posterior, anterior, and periurethral surgical reconstruction of urinary continence mechanisms in robot-assisted radical prostatectomy: a description and video compilation of commonly performed surgical. Techniques 76(6):814–822
Gilbert SM et al (2010) Development and validation of the Bladder Cancer Index: a comprehensive, disease specific measure of health related quality of life in patients with localized bladder cancer. J Urol 183(5):1764–1769
Zhang Z et al (2013) Early and late urodynamic assessment of the orthotopic N-shaped neobladder. Oncol Lett 6(4):1053–1056
Noguchi M et al (2008) A randomized clinical trial of suspension technique for improving early recovery of urinary continence after radical retropubic prostatectomy. BJU Int 102(8):958–963
Nguyen MM et al (2008) Early continence outcomes of posterior musculofascial plate reconstruction during robotic and laparoscopic prostatectomy. BJU Int 101(9):1135–1139
Lopez-Beltran A et al (2017) Concomitant bladder cancer and prostate cancer: challenges and controversies. Nat Rev Urol 14(10):620–629
Funding
This study was funded by the National Key Research and Development Program of China (Grant No. 2018YFA0902803, 2017YFC1308600); the National Natural Science Foundation of China (Grant No. 81825016, 81802530, 81830082, 81672395, 81871945, 81772719, 81772728, 2072639, 91740119, 81472381, 81972385, 82173266, 81802552); the Key Areas Research and Development Program of Guangdong (Grant No. 2020A1515010815, 2018B010109006, 2017A020215072); the Science and Technology Planning Project of Guangdong Province (Grant No. 202002030388, 201803010049, 2017B020227007, 201704020097); Guangdong Clinical Research Center for Urological Diseases(Grant No. 2020B1111170006); Yixian Youth project of Sun Yat-sen Memorial Hospital (Grant No. YXQH201812); Young Teacher Training Funding of Sun Yat-sen University (Grant No. 19ykzd21, 19ykpy121); Science and Technology Program of Guangzhou, China (Grant No.201904010004); Natural Science Foundation of Guangdong Province, China (Grant No.2018A030313545).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. W He: Conception of research, Manuscript writing. JT Yang: Data collection, Manuscript writing. MC Gao: Data collection, Statistical analysis. H Liu: Review of the draft. JB Li: Quality control. JT Hu: Statistical analysis. YS Zhang: Statistical analysis. GZ Zhong: Statistical analysis. KW Li: Data collection. WD: Data collection. H Huang: Manuscript preparation. TL: Conception of research, Quality control. J Huang: Conception of research, Quality control. All persons who meet authorship criteria are listed as authors, and all authors certify that they have participated sufficiently in the work to take public responsibility for the content, including participation in the concept, design, analysis, writing, or revision of the manuscript. Furthermore, each author certifies that this material or similar material has not been and will not be submitted to or published in any other publication before its appearance in the Journal of Endourology.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Research involving human participants
The study was an observational retrospective study and approved by the ethics committee of Sun Yat-sen Memorial Hospital (Approval No. SYSEC-KY-KS-2021–136). All procedures performed in studies involving human participants were under the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. We have received broad consent from the ethics committee of Sun Yat-sen Memorial Hospital.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
11255_2022_3214_MOESM1_ESM.eps
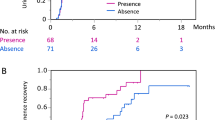
Figure S1 Subgroup analysis: Kaplan-Meier curves showing the probability of postoperative daytime (a) and nighttime (b) continence in NVB sparing, NVB combined with CPR and LCS patients. (EPS 13 KB)
11255_2022_3214_MOESM2_ESM.eps
Figure S2 Kaplan-Meier curves showing the probability of postoperative daytime and nighttime continence after RARC in the standard group (a, b) and CPR group (c, d) according to nerve sparing procedure. (EPS 20 KB)
Rights and permissions
About this article
Cite this article
He, W., Yang, J., Gao, M. et al. Pelvic reconstruction and lateral prostate capsule sparing techniques improve early continence of robot-assisted radical cystectomy with orthotopic ileal neobladder. Int Urol Nephrol 54, 1537–1543 (2022). https://doi.org/10.1007/s11255-022-03214-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-022-03214-4