Abstract
Purpose
Malnutrition is a common comorbidity of coronary artery disease (CAD) and is often associated with adverse events. The malnutrition often means lower cholesterol, albumin and high lymphocyte, as risk factors of Contrast-Induced Acute Kidney Injury (CI-AKI). We aim to evaluate the association between malnutrition and CI-AKI following coronary angiography (CAG) in CAD patients.
Methods
We analyzed 3170 CAD patients with variables of nutritional status (Controlling Nutritional Status score (CONUT)) from the prospective multicenter study, REICIN (NCT01402232) including 4,271 consecutive patients undergoing CAG from January 2013 to February 2016. Patients were divided into the normal group (CONUT score 0–1) and malnutrition group (CONUT score > 1). The association of malnutrition and the risk of CI-AKI was examined in all CAD patients using multivariable logistics regression analysis.
Results
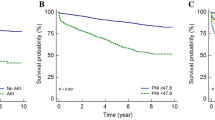
Among the 3170 patients (mean age: 63.1 ± 10.7 years), 1865 (58.8%) suffered from malnutrition, 111 (3.5%) developed CI-AKI, including 23 (1.76%) in normal group and 88 (4.72%) in malnutrition group (p < 0.01). The malnourished patients were older, and likely had anemia and worse cardiorenal function. After adjustment for confounders, the risk of CI-AKI was 1.04 times higher in the malnutrition group than in the normal group (adjusted OR: 2.04, 95% CI 1.28–3.38, p < 0.01).
Conclusions
Among CAD patients undergoing CAG, malnutrition is extremely common and associated with a double risk of CI-AKI. Further studies are needed to investigate the potential renal protection of intervening malnutrition in CAD patients.
Similar content being viewed by others
Availability of data and material
Not applicable.
Code availability
Not applicable.
References
McCullough PA, Choi JP, Feghali GA, Schussler JM, Stoler RM, Vallabahn RC, Mehta A (2016) Contrast-induced acute kidney injury. J Am Coll Cardiol 68:1465–1473. https://doi.org/10.1016/j.jacc.2016.05.099
Rear R, Bell RM, Hausenloy DJ (2016) Contrast-induced nephropathy following angiography and cardiac interventions. Heart 102:638–648. https://doi.org/10.1136/heartjnl-2014-306962
Raposeiras Roubín S, Abu Assi E, Cespón Fernandez M, Barreiro Pardal C, Lizancos Castro A, Parada JA, Pérez DD, Blanco Prieto S, Rossello X, Ibanez B, Íñiguez Romo A (2020) J Am Coll Cardiol 76:828–840. https://doi.org/10.1016/j.jacc.2020.06.058
Wada H, Dohi T, Miyauchi K, Doi S, Konishi H, Naito R, Tsuboi S, Ogita M, Kasai T, Okazaki S, Isoda K, Suwa S, Daida H (2017) Prognostic impact of nutritional status assessed by the Controlling Nutritional Status score in patients with stable coronary artery disease undergoing percutaneous coronary intervention. Clin Res Cardiol 106:875–883. https://doi.org/10.1007/s00392-017-1132-z
Kunimura A, Ishii H, Uetani T, Aoki T, Harada K, Hirayama K, Negishi Y, Shibata Y, Sumi T, Kawashima K, Tatami Y, Kawamiya T, Yamamoto D, Suzuki S, Amano T, Murohara T (2017) Impact of nutritional assessment and body mass index on cardiovascular outcomes in patients with stable coronary artery disease. Int J Cardiol 230:653–658. https://doi.org/10.1016/j.ijcard.2017.01.008
Murat SN, Kurtul A, Yarlioglues M (2015) Impact of serum albumin levels on contrast-induced acute kidney injury in patients with acute coronary syndromes treated with percutaneous coronary intervention. Angiology 66:732–737. https://doi.org/10.1177/0003319714551979
Lankinen R, Hakamäki M, Metsärinne K, Koivuviita N, Pärkkä JP, Saarenhovi M, Hellman T, Järvisalo MJ (2021) Association of maximal stress ergometry performance with troponin T and abdominal aortic calcification score in advanced chronic kidney disease. BMC Nephrol 22:50. https://doi.org/10.1186/s12882-021-02251-y
Qin YH, Yan GL, Ma CL, Tang CC, Ma GS (2018) Effects of hyperglycaemia and elevated glycosylated haemoglobin on contrast-induced nephropathy after coronary angiography. Exp Ther Med 16:377–383. https://doi.org/10.3892/etm.2018.6183
Li S, Tang X, Peng L, Luo Y, Zhao Y, Chen L, Dong R, Zhu J, Chen Y, Liu J (2015) A head-to-head comparison of homocysteine and cystatin C as pre-procedure predictors for contrast-induced nephropathy in patients undergoing coronary computed tomography angiography. Clin Chim Acta 444:86–91. https://doi.org/10.1016/j.cca.2015.02.019
Ignacio de Ulíbarri J, González-Madroño A, de Villar NG, González P, González B, Mancha A, Rodríguez F, Fernández G (2005) CONUT: a tool for controlling nutritional status. First validation in a hospital population. Nutr Hosp 20:38–45
Waitzberg DL, Caiaffa WT, Correia MI (2001) Hospital malnutrition: the Brazilian national survey (IBRANUTRI): a study of 4000 patients. Nutrition 17:573–580. https://doi.org/10.1016/s0899-9007(01)00573-1
Correia MI, Campos AC (2003) Prevalence of hospital malnutrition in Latin America: the multicenter ELAN study. Nutrition 19:823–825. https://doi.org/10.1016/s0899-9007(03)00168-0
Pirlich M, Schütz T, Kemps M, Luhman N, Minko N, Lübke HJ, Rossnagel K, Willich SN, Lochs H (2005) Social risk factors for hospital malnutrition. Nutrition 21:295–300. https://doi.org/10.1016/j.nut.2004.06.023
Anker SD, Coats AJ (1999) Cardiac cachexia: a syndrome with impaired survival and immune and neuroendocrine activation. Chest 115:836–847. https://doi.org/10.1378/chest.115.3.836
Piggott KD, Liu A, Monczka J, Fakioglu H, Narasimhulu SS, Pourmoghadam K, DeCampli W (2018) Inadequate preoperative nutrition might be associated with acute kidney injury and greater illness severity postoperatively. J Thorac Cardiovasc Surg 155:2104–2109. https://doi.org/10.1016/j.jtcvs.2017.12.080
Li C, Xu L, Guan C, Zhao L, Luo C, Zhou B, Zhang X, Wang J, Zhao J, Huang J, Li D, Luan H, Man X, Che L, Wang Y, Zhang H, Xu Y (2020) Malnutrition screening and acute kidney injury in hospitalised patients: a retrospective study over a 5-year period from China. Br J Nutr 123:337–346. https://doi.org/10.1017/s000711451900271x
Chen YL, Fu NK, Xu J, Yang SC, Li S, Liu YY, Cong HL (2014) A simple preprocedural score for risk of contrast-induced acute kidney injury after percutaneous coronary intervention. Catheter Cardiovasc Interv 83:E8-16. https://doi.org/10.1002/ccd.25109
Börekçi A, Gür M, Türkoğlu C, Çaylı M, Selek Ş, Kaypaklı O, Uçar H, Coşkun M, Şeker T, Koç M, Gökdeniz T, Gözükara MY (2015) Oxidative stress and paraoxonase 1 activity predict contrast-induced nephropathy in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Angiology 66:339–345. https://doi.org/10.1177/0003319714533588
Dennis KK, Go YM, Jones DP (2019) Redox systems biology of nutrition and oxidative stress. J Nutr 149:553–565. https://doi.org/10.1093/jn/nxy306
Merker M, Felder M, Gueissaz L, Bolliger R, Tribolet P, Kägi-Braun N, Gomes F, Hoess C, Pavlicek V, Bilz S, Sigrist S, Brändle M, Henzen C, Thomann R, Rutishauser J, Aujesky D, Rodondi N, Donzé J, Stanga Z, Mueller B, Schuetz P (2020) Association of Baseline Inflammation With Effectiveness of Nutritional Support Among Patients With Disease-Related Malnutrition: A Secondary Analysis of a Randomized Clinical Trial. JAMA Netw Open 3:e200663. https://doi.org/10.1001/jamanetworkopen.2020.0663
Liu L, Liu Y, Liu C, Zhang Z, Du Y, Zhao H (2016) Analysis of gene expression profile identifies potential biomarkers for atherosclerosis. Mol Med Rep 14:3052–3058. https://doi.org/10.3892/mmr.2016.5650
Sueta D, Hokimoto S, Sakamoto K, Akasaka T, Tabata N, Kaikita K, Honda O, Naruse M, Ogawa H (2017) Validation of the high mortality rate of Malnutrition-Inflammation-Atherosclerosis syndrome: -Community-based observational study. Int J Cardiol 230:97–102. https://doi.org/10.1016/j.ijcard.2016.12.072
Santarpia L, Contaldo F, Pasanisi F (2011) Nutritional screening and early treatment of malnutrition in cancer patients. J Cachexia Sarcopenia Muscle 2:27–35. https://doi.org/10.1007/s13539-011-0022-x
Funding
This study was supported by grants from the Beijing Lisheng Cardiovascular Health Foundation and Guangdong Provincial People's Hospital Foundation (LHJJ20141751) and the National Science Foundation of China (81670339, 81970311) and Medical Scientific Research Foundation of Guangdong Province (A2019414). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript; the work was not funded by any industry sponsors.
Author information
Authors and Affiliations
Contributions
The authors’ responsibilities were as follows—Research idea and study design: SQC, LLC, YL and KHC; Data acquisition: JLI, ZDH, HZH, YBH, JJL, JLU, YFY, YHL RWL, YYH, MFL, YL, YZH, JFY and KHC; Data analysis/interpretation: JLI, HZH; Statistical analysis: ZDH, HZH; Supervision and mentorship: SQC, LLC, YL; Writing guidance: SQC, YL. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions on the accuracy or integrity of any portion of the work are appropriately investigated and resolved. The authors declare that there is no competing interest. All authors read and approved the final version.
Corresponding authors
Ethics declarations
Conflicts of interest
Not applicable.
Ethics approval
The study and all of its protocols were approved by the institutional Ethics Research Committee of Guangdong Provincial People’s Hospital (No. GDREC2012141H). All patients were given written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chen, L., Huang, Z., Li, W. et al. Malnutrition and the risk for contrast-induced acute kidney injury in patients with coronary artery disease. Int Urol Nephrol 54, 429–435 (2022). https://doi.org/10.1007/s11255-021-02915-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-021-02915-6