Abstract
Objectives
To analyze effects of intraurethral EPO application on urethral wound healing by defining hystopathologic changes in a rat model of hypospadias.
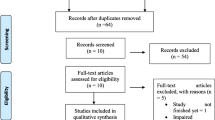
Methods
A hypospadias model was created in 30 rats and randomized into 3 groups of 10. For 14 days, the first group was administered 25 iu EPO instillation intraurethrally once a day, while group 2 was administered with 50 iu EPO in the same manner. The third group was assigned as control group. On the day 15, rats were sacrificed and penectomies were performed. One independent pathologist who is blinded to groups and treatments evaluated the penis samples.
Results
Histopathologic examinations yielded the mean fibrosis scores (± SD) as 1.9 ± 0.568, 1.1 ± 0.786 and 2.5 ± 0.535 in groups I, II and III, respectively. There was significant difference between the EPO groups and the control group (p = 0.04-I, p = 0.003-II). The mean inflammation scar scores (± SD) were determined as 1 ± 1.054, 2 ± 1.247, 2.63 ± 0.744 in groups I, II and III, respectively. There was a significant difference in terms of inflammation between control group and group I (p = 0.005). Mean congestion scores (± SD) were found 1.2 ± 0.789 in groups I–II and 0.75 ± 0.463 in group III (p = 0.310). Hyperemia was seen in 60% 70% and 37.5% in groups I, II and III, respectively (p = 0.387).
Conclusion
Intraurethral EPO therapy effected urethral wound healing in a good way. Thus it could be feasible to treat the patients with after hypospadias surgeries and to improve success rates.




Similar content being viewed by others
Availability of data and material
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Shih EM, Graham JM Jr (2014) Review of genetic and environmental factors leading to hypospadias. Eur J Med Genet 57:453–463
Springer A, Van Den Heijkant M, Baumann S (2016) Worldwide prevalence of hypospadias. J Pediatr Urol 12:152. e151-152. e157
Tekgül S, Riedmiller H, Gerharz E, Hoebeke P, Kocvara R, Nijman R, Radmayr C, Stein R (2015) Guidelines on paediatric urology. Europ Assoc Urol 1:13–15
Van der Horst H, De Wall L (2017) Hypospadias, all there is to know. Eur J Pediatr 176:435–441
Bhat A, Mandal AK (2008) Acute postoperative complications of hypospadias repair. Indian J Urol 24:241
Duckett JW (1998) Hypospadias. Campbell’s Urol 2:2093–2119
Snyder CL, Evangelidis A, Hansen G, Peter SDS, Ostlie DJ, Gatti JM, Gittes GK, Sharp RJ, Murphy JP (2005) Management of complications after hypospadias repair. Urology 65:782–785
El Kassaby A, AbouShwareb T, Atala A (2008) Randomized comparative study between buccal mucosal and acellular bladder matrix grafts in complex anterior urethral strictures. J Urol 179:1432–1436
Lin D, Wang G, Song H, Qu Y, Liu P, Liang H, Xu S, Chen S, Zhang W, Zhao Y (2020) Use of acellular dermal matrix for urethroplasty coverage in proximal hypospadias repair: a pilot study. Adv Therapy 1:11
Kaya C, Bektic J, Radmayr C, Schwentner C, Bartsch G, Oswald J (2008) The efficacy of dihydrotestosterone transdermal gel before primary hypospadias surgery: a prospective, controlled, randomized study. J Urol 179:684–688
Karakan T, Ozcan S, Bagcioglu M, Aydın A, Doluoglu O, Yucel M, Adalı Y, Yagli O (2019) The effect of intraurethral dexpanthenol in hypospadias repair: experimental rabbit study. J Pediatr Urol 15(375):e371–e375
Sahinkanat T, Ozkan KU, Cıralık H, Ozturk S, Resim S (2009) Botulinum toxin-A to improve urethral wound healing: an experimental study in a rat model. Urology 73:405–409
Mazdak H, Meshki I, Ghassami F (2007) Effect of mitomycin C on anterior urethral stricture recurrence after internal urethrotomy. Eur Urol 51:1089–1092
Nagler A, Gofrit O, Ohana M, Pode D, Genina O, Pines M (2000) The effect of halofuginone, an inhibitor of collagen type I synthesis, on urethral stricture formation: in vivo and in vitro study in a rat model. J Urol 164:1776–1780
Shirazi M, Khezri A, Samani SM, Monabbati A, Kojoori J, Hassanpour A (2007) Effect of intraurethral captopril gel on the recurrence of urethral stricture after direct vision internal urethrotomy: Phase II clinical trial. Int J Urol 14:203–208
Hebert P (1972) The treatment of urethral stricture: transurethral injection of triamcinolone. J Urol 108:745–747
Lu H, Wu X, Wang Z, Li L, Chen W, Yang M, Huo D, Zeng W, Zhu C (2016) Erythropoietin-activated mesenchymal stem cells promote healing ulcers by improving microenvironment. J Surg Res 205:464–473
Hofer MD, Cheng EY, Bury MI, Park E, Xu W, Hong SJ, Kaplan WE, Sharma AK (2014) Analysis of primary urethral wound healing in the rat. Urology 84:246. e241-246. e247
Bouty A, Ayers KL, Pask A, Heloury Y, Sinclair AH (2015) The genetic and environmental factors underlying hypospadias. Sexual Develop 9:239–259
Yıldız A, Bakan V (2010) Comparison of perimeatal-based flap and tubularized incised plate urethroplasty combined with single-or double-layer dartos flap in distal hypospadias. Urol Int 84:265–268
Cruz-Diaz O, Castellan M, Gosalbez R (2013) Use of buccal mucosa in hypospadias repair. Curr Urol Rep 14:366–372
Jia W, Liu G-c, Zhang L-y, Wen Y-q, Fu W, Hu J-h, Wang Z, He Q-m, Xia H-m (2016) Comparison of tubularized incised plate urethroplasty combined with a meatus-based ventral dartos flap or dorsal dartos flap in hypospadias. Pediatr Surg Int 32:411–415
Hassan JM, Pope JC IV, Revelo P, Adams MC, Brock JW III, DeMarco RT (2006) The role of postoperative testosterone in repair of iatrogenic hypospadias in rabbits. J Pediatr Urol 2:329–332
Brines M, Cerami A (2006) Discovering erythropoietin’s extra-hematopoietic functions: biology and clinical promise. Kidney Int 70:246–250
Badiavas EV, Falanga V (2003) Treatment of chronic wounds with bone marrow–derived cells. Arch Dermatol 139:510–516
Suh W, Kim KL, Kim JM, Shin IS, Lee YS, Lee JY, Jang HS, Lee JS, Byun J, Choi JH (2005) Transplantation of endothelial progenitor cells accelerates dermal wound healing with increased recruitment of monocytes/macrophages and neovascularization. Stem cells 23:1571–1578
Kilinc MF, Doluoglu OG, Eser PE, Yildiz Y, Yazar VM, Ayyildiz A, Hucumenoglu S (2019) Intraurethral erythropoietin to prevent fibrosis and improve urethral healing: an experimental study in a rat model. Urology 123:297e299-297. e214
Funding
No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
E Tokat: protocol/project development, data collection or management, data analysis, manuscript writing/editing. Y Yıldız: protocol/project development, data collection or management. EP Eser: data collection or management, data analysis. MF Kılınç: protocol/project development, data collection or management, manuscript writing/editing. ÖG Doluoğlu: manuscript writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest that are relevant to the content of this article.
Ethics approval
The study was approved by the Local Ethics Committee of Ankara Training and Research Hospital (Reference number: 63-642).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tokat, E., Yildiz, Y., Eser, P.E. et al. Does intraurethral erythropoietin administration effect wound healing after hypospadias correction? an experimental rat study. Int Urol Nephrol 53, 2057–2062 (2021). https://doi.org/10.1007/s11255-021-02912-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-021-02912-9