Abstract
Background
Inflammation, oxidative stress (OS), atherosclerosis and resistant hypertension (RH) are common features of chronic kidney disease (CKD) leading to a higher risk of death from cardiovascular disease. These effects seem to be modulated by impaired anti-oxidant, anti-inflammatory and reverse cholesterol transport actions of high-density lipoprotein cholesterol (HDL). HDL prevents and reverses monocyte recruitment and activation into the arterial wall and impairs endothelial adhesion molecule expression. Recently, monocyte count to HDL-cholesterol ratio (MHR) has emerged as a potential marker of inflammation and OS, demonstrating to be relevant in CKD. Our research was aimed to assess, for the first time, its reliability in RH.
Methods
We performed a retrospective study on 214 patients with CKD and arterial hypertension who were admitted between January and June 2019 to our Department, 72 of whom were diagnosed with RH.
Results
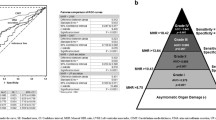
MHR appeared inversely related to eGFR (ρ = − 0.163; P = 0.0172). MHR was significantly higher among RH patients compared to non-RH ones (12.39 [IQR 10.67–16.05] versus 7.30 [5.49–9.06]; P < 0.0001). Moreover, MHR was significantly different according to the number of anti-hypertensive drugs per patient in the whole study cohort (F = 46.723; P < 0.001) as well as in the non-RH group (F = 14.191; P < 0.001). Moreover, MHR positively correlates with diabetes mellitus (ρ = 0.253; P = 0.0002), white blood cells (ρ = 0.664; P < 0.0001) and C-reactive protein (ρ = 0.563; P < 0.0001).
Conclusions
MHR may be a reliable biomarker due to the connection between HDL and monocytes. Our study suggests that MHR is linked with the use of multiple anti-hypertensive therapy and resistant hypertension in CKD patients, and can be a useful ratio to implement appropriate treatment strategies.







Similar content being viewed by others
References
Go AS, Chertow GM, Fan D, McCulloch C, Hsu C (2004) Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 351:1296–1305
Untersteller K, Meissl S, Trieb M, Emrich IE, Zawada AM, Holzer M, Knuplez E, Fliser D, Heine GH, Marsche G (2018) HDL functionality and cardiovascular outcome among nondialysis chronic kidney disease patients. J Lipid Res 59(7):1256–1265
Balla S, Nusair MB, Alpert MA (2013) Risk factors for atherosclerosis in patients with chronic kidney disease: recognition and management. Curr Opin Pharmacol 13(2):192–199
Vaziri ND, Navab M, Fogelman AM (2010) HDL metabolism and activity in chronic kidney disease. Nat Rev Nephrol 6(5):287–296
Maeda S, Nakanishi S, Yoneda M, Awaya T, Yamane K, Hirano T, Kohno N (2012) Associations between small dense LDL, HDL subfractions (HDL2, HDL3) and risk of atherosclerosis in Japanese-Americans. J Atheroscler Thromb 19(5):444–452
Zwijsen RM, de Haan LH, Kuivenhoven JA, Nusselder IC (1991) Modulation of low-density lipoprotein-induced inhibition of intercellular communication by antioxidants and high-density lipoproteins. Food Chem Toxicol 29(9):615–620
Bandeali S, Farmer J (2012) High-density lipoprotein and atherosclerosis: the role of antioxidant activity. Curr Atheroscler Rep 14(2):101–107
Mackness B, Mackness M (2012) The antioxidant properties of high-density lipoproteins in atherosclerosis. Panminerva Med 54(2):83–90
Conti G, Caccamo D, Siligato R, Gembillo G, Satta E, Pazzano D, Carucci N, Carella A, Campo GD, Salvo A, Santoro D (2019) Association of higher advanced oxidation protein products (AOPPs) levels in patients with diabetic and hypertensive nephropathy. Med (Kaunas) 55(10):7
Gembillo G, Cernaro V, Salvo A, Siligato R, Laudani A, Buemi M, Santoro D (2019) Role of vitamin D status in diabetic patients with renal disease. Med (Kaunas) 55(6):273
Pugh D, Gallacher PJ, Dhaun N (2020) Management of hypertension in chronic kidney disease [published correction appears in Drugs 2020 Aug 25]. Drugs 79(4):365–379. https://doi.org/10.1007/s40265-019-1064-1
Sun HJ (2019) Current opinion for hypertension in renal fibrosis. Adv Exp Med Biol 1165:37–47. https://doi.org/10.1007/978-981-13-8871-2_3
McCarty MF (2006) Adjuvant strategies for prevention of glomerulosclerosis. Med Hypotheses 67(6):1277–1296
Klahr S, Morrissey JJ (2000) The role of vasoactive compounds, growth factors and cytokines in the progression of renal disease. Kidney Int Suppl 7:S7-14
Nogueira A, Pires MJ, Oliveira PA (2017) Pathophysiological mechanisms of renal fibrosis: a review of animal models and therapeutic strategies. In Vivo 31(1):1–22. https://doi.org/10.21873/invivo.11019
Cernaro V, Loddo S, Macaione V et al (2020) RAS inhibition modulates kynurenine levels in a CKD population with and without type 2 diabetes mellitus. Int Urol Nephrol 52(6):1125–1133. https://doi.org/10.1007/s11255-020-02469-z
Remuzzi G, Benigni A, Remuzzi A (2006) Mechanisms of progression and regression of renal lesions of chronic nephropathies and diabetes. J Clin Invest 116(2):288–296
Klahr S, Morrissey J (2002) Obstructive nephropathy and renal fibrosis. Am J Physiol Renal Physiol 283(5):F861-875
Mennuni S, Rubattu S, Pierelli G, Tocci G, Fofi C, Volpe M (2014) Hypertension and kidneys: unraveling complex molecular mechanisms underlying hypertensive renal damage. J Hum Hypertens 28:74–79
Nicholls SJ, Dusting GJ, Cutri B, Bao S, Drummond GR, Rye KA, Barter PJ (2005) Reconstituted high-density lipoproteins inhibit the acute pro-oxidant and proinflammatory vascular changes induced by a periarterial collar in normocholesterolemic rabbits. Circulation 111:1543–1550
Tedgui A, Mallat Z (2001) Anti-inflammatory mechanisms in the vascular wall. Circ Res 88:877–887
Xia P, Vadas MA, Rye KA, Barter PJ, Gamble JR (1999) High density lipoproteins (HDL) interrupt the sphingosine kinase signaling pathway. A possible mechanism for protection against atherosclerosis by HDL. J Biol Chem 274:33143–33147
Nicholls SJ, Nelson AJ (2019) HDL and cardiovascular disease. Pathology 51(2):142–147
Ganjali S, Gotto AM Jr, Ruscica M, Atkin SL, Butler AE, Banach M, Sahebkar A (2018) Monocyte-to-HDL-cholesterol ratio as a prognostic marker in cardiovascular diseases. J Cell Physiol 233(12):9237–9246
Kuvin JT, Rämet ME, Patel AR, Pandian NG, Mendelsohn ME, Karas RH (2002) A novel mechanism for the beneficial vascular effects of high-density lipoprotein cholesterol: enhanced vasorelaxation and increased endothelial nitric oxide synthase expression. Am Heart J 144(1):165–172
Linton MRF, Yancey PG, Davies SS et al (2019) The role of lipids and lipoproteins in atherosclerosis. [Updated 2019 Jan 3]. In: Feingold KR, Anawalt B, Boyce A et al (eds) Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc. https://www.ncbi.nlm.nih.gov/books/NBK343489/
Canpolat U, Cetin EH, Cetin S, Aydin S, Akboga MK, Yayla C, Turak O, Aras D, Aydogdu S (2016) Association of monocyte-to-HDL cholesterol ratio with slow coronary flow is linked to systemic inflammation. Clin Appl Thromb Hemost 22:476–482. https://doi.org/10.1177/1076029615594002
Viedt C, Orth SR (2002) Monocyte chemoattractant protein-1 (MCP-1) in the kidney: does it more than simply attract monocytes? Nephrol Dial Transplant 17(12):2043–2047. https://doi.org/10.1093/ndt/17.12.2043 (PMID: 12454208)
Williams B, Mancia G, Spiering W et al (2018) 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J 39(33):3021–3104
Levey A, Stevens L, Schmid C, Zhang YL, Castro AF, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J (2009) CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration). A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612
Yvan-Charvet L, Pagler T, Gautier EL, Avagyan S, Siry RL, Han S, Welch CL, Wang N, Randolph GJ, Snoeck HW, Tall AR (2010) ATP-binding cassette transporters and HDL suppress hematopoietic stem cell proliferation. Science 328(5986):1689–1693
Patel VK, Williams H, Li SCH, Fletcher JP, Medbury HJ (2017) Monocyte inflammatory profile is specific for individuals and associated with altered blood lipid levels. Atherosclerosis 263:15–23
Karataş MB, Çanga Y, Özcan KS, Ipek G, Güngör B, Onuk T, Durmuş G, Öz A, Karaca M, Bolca O (2016) Monocyte to high-density lipoprotein ratio as a new prognostic marker in patients with STEMI undergoing primary percutaneous coronary intervention. Am J Emerg Med 34(2):240–244
Cetin EHO, Cetin MS, Canpolat U, Aydin S, Topaloglu S, Aras D, Aydogdu S (2015) Monocyte/HDL-cholesterol ratio predicts the definite stent thrombosis after primary percutaneous coronary intervention for ST-segment elevation myocardial infarction. Biomark Med 9(10):967–977
You S, Zhong C, Zheng D, Xu J, Zhang X, Liu H, Zhang Y, Shi J, Huang Z, Cao Y, Liu CF (2017) Monocyte to HDL cholesterol ratio is associated with discharge and 3- month outcome in patients with acute intracerebral hemorrhage. J Neurol Sci 372:157–161
Dogan A, Oylumlu M (2017) Increased monocyte-to-HDL cholesterol ratio is related to cardiac syndrome X. Acta Cardiol 72(5):516–521
Sarov-Blat L, Kiss RS, Haidar B, Kavaslar N, Jaye M, Bertiaux M, Steplewski K, Hurle MR, Sprecher D, McPherson R, Marcel YL (2007) Predominance of a proinflammatory phenotype in monocyte-derived macrophages from subjects with low plasma HDL-cholesterol. Arterioscler Thromb Vasc Biol 27(5):1115–1122
Selcuk M, Yildirim E, Saylik F (2019) Comparison of monocyte with high density lipoprotein cholesterol ratio in dipper and nondipper hypertensive patients. Biomark Med 13(15):1289–1296
Aydin E, Ates I, Fettah Arikan M, Yilmaz N, Dede F (2017) The ratio of monocyte frequency to HDL cholesterol level as a predictor of asymptomatic organ damage in patients with primary hypertension. Hypertens Res 40(8):758–764
Kanbay M, Solak Y, Unal HU, Kurt YG, Gok M, Cetinkaya H, Karaman M, Oguz Y, Eyileten T, Vural A, Covic A, Goldsmith D, Turak O, Yilmaz MI (2014) Monocyte count/HDL cholesterol ratio and cardiovascular events in patients with chronic kidney disease. Int Urol Nephrol 46:1619–1625
Shi WR, Wang HY, Chen S, Guo XF, Li Z, Sun YX (2019) The impact of monocyte to high-density lipoprotein ratio on reduced renal function: insights from a large population. Biomark Med 13(9):773–783
Batista MC, Welty FK, Diffenderfer MR et al (2004) (2004) Apolipoprotein A-I, B-100, and B-48 metabolism in subjects with chronic kidney disease, obesity, and the metabolic syndrome. Metabolism 53(10):1255–1261. https://doi.org/10.1016/j.metabol.2004.05.001
Bowe B, Xie Y, Xian H, Li T, Al-Aly Z (2017) Association between monocyte count and risk of incident CKD and progression to ESRD. Clin J Am Soc Nephrol 12(4):603–613
Cases A, Coll E (2005) Dyslipidemia and the progression of renal disease in chronic renal failure patients. Kidney Int Suppl 99:S87-93
Bae JC, Han JM, Kwon S, Jee JH, Yu TY, Lee MK, Kim JH (2016) LDL-C/apoB and HDL-C/apoA-1 ratios predict incident chronic kidney disease in a large apparently healthy cohort. Atherosclerosis 251:170–176
Bowe B, Xie Y, Xian H, Balasubramanian S, Al-Aly Z (2016) Low levels of high-density lipoprotein cholesterol increase the risk of incident kidney disease and its progression. Kidney Int 89(4):886–896
Xu W, Guan H, Gao D, Pan J, Wang Z, Alam M, Lian J, Zhou J (2019) Sex-specific association of monocyte count to high-density lipoprotein ratio with SYNTAX score in patients with suspected stable coronary artery disease. Med (Baltim). 98(41):e17536
Davis CE, Williams DH, Oganov RG, Tao SC, Rywik SL, Stein Y, Little JA (1996) Sex difference in high density lipoprotein cholesterol in six countries. Am J Epidemiol 143:1100–1106
Rossouw JE (2002) Hormones, genetic factors, and gender differences in cardiovascular disease. Cardiovasc Res 53:550–557
Acknowledgements
We thank the nurse staff of the Unit of Nephrology and Dialysis for their help with the blood sampling and the blood pressure measurement of the patients.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization, GG, DS, RS; data curation, RS, GG, AS, AR, GS; formal analysis, VC, VCA and GG; investigation, GG, DS; methodology, GG, GC and DS; supervision, GG, GC and DS; writing—original draft, GG, RS, DS and ES; writing—review & editing, GF, RS, GG and VC. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Conflicts of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gembillo, G., Siligato, R., Cernaro, V. et al. Monocyte to HDL ratio: a novel marker of resistant hypertension in CKD patients. Int Urol Nephrol 54, 395–403 (2022). https://doi.org/10.1007/s11255-021-02904-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-021-02904-9