Abstract
Purpose
Identifying performance-based tests that meaningful for patients may facilitate the implementation of rehabilitation programs. The primary aim of this study was to determine the independent associations between different performance-based tests and health-related quality of life (HRQoL) among elderly peritoneal dialysis (PD) patients.
Methods
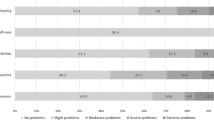
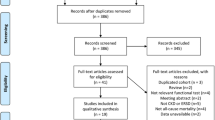
This cross-sectional study was conducted in China. Patients on PD who were 60 years of age or above were included. HRQoL was assessed using the Medical Outcomes Study Short Form 36. Physical function was determined by handgrip strength, timed up and go (TUG) test, 5-repetition sit-to-stand test, and comfortable gait speed. Depressive symptoms were measured using the self-reported Geriatric Depression Scale (GDS-15). Multiple linear regression analyses were performed to examine the factors influencing HRQoL.
Results
In total, 115 participants with a mean age of 69.7 were included (46 women and 69 men). TUG (β =− 0.460, p < 0.001), prealbumin (β = 0.223, p = 0.014), and education level (β = 0.183, p = 0.042) were associated with physical health. GDS score (β = − 0.475, p < 0.001), serum albumin level (β = 0.264, p = 0.003), and sex (β = 0.217, p = 0.012), were associated with mental HRQoL.
Conclusion
TUG could be a valuable test for use in clinical practice and research aiming at facilitating tailed exercise programs, as it was associated with self-perceived physical HRQoL and could be meaningful to elderly PD patients. Depressive symptoms and nutrition were another two important rehabilitation areas for optimizing the overall HRQoL of older adults on PD.
Similar content being viewed by others
Availability of data and materials
The datasets generated and/or analyzed during the current study will be available from the corresponding author on reasonable request.
References
Xie Y, Bowe B, Mokdad AH et al (2018) Analysis of the Global Burden of Disease study highlights the global, regional, and national trends of chronic kidney disease epidemiology from 1990 to 2016. Kidney Int 94:567–581. https://doi.org/10.1016/j.kint.2018.04.011
United States Renal Data System (2019) US renal data system 2019 annual data report: epidemiology of kidney disease in the United States. https://www.usrds.org/2019/view/USRDS_2019_ES_final.pdf. Accessed 10 Feb 2020
Wang F, Yang C, Long J et al (2019) Executive summary for the 2015 annual data report of the China kidney disease network (CK-NET). Kidney Int 95:501–505. https://doi.org/10.1016/j.kint.2018.11.011
Walker RC, Morton RL, Palmer SC et al (2018) A discrete choice study of patient preferences for dialysis modalities. Clin J Am Soc Nephrol 13:100–108. https://doi.org/10.2215/cjn.06830617
Brown EA, Johansson L, Farrington K et al (2010) Broadening options for long-term dialysis in the elderly (BOLDE): differences in quality of life on peritoneal dialysis compared to haemodialysis for older patients. Nephrol Dial Transplant 25:3755–3763. https://doi.org/10.1093/ndt/gfq212
Guilloteau S, Lobbedez T, Guillouet S et al (2018) Impact of assisted peritoneal dialysis modality on outcomes: a cohort study of the French language peritoneal dialysis registry. Am J Nephrol 48:425–433. https://doi.org/10.1159/000494664
Sun L, Zou LX, Han YC et al (2016) Forecast of the incidence, prevalence and burden of end-stage renal disease in Nanjing, China to the year 2025. BMC Nephrol 17:60. https://doi.org/10.1186/s12882-016-0269-8
van Loon IN, Bots ML, Boereboom FTJ et al (2017) Quality of life as indicator of poor outcome in hemodialysis: relation with mortality in different age groups. BMC Nephrol 18:217. https://doi.org/10.1186/s12882-017-0621-7
Hall RK, Luciano A, Pieper C et al (2018) Association of kidney disease quality of life (KDQOL-36) with mortality and hospitalization in older adults receiving hemodialysis. BMC Nephrol 19:11. https://doi.org/10.1186/s12882-017-0801-5
Torino C, Panuccio V, Tripepi R et al (2020) The dominant prognostic value of physical functioning among quality of life domains in end-stage kidney disease. Nephrol Dial Transplant 35:170–175. https://doi.org/10.1093/ndt/gfy334
Pei M, Aguiar R, Pagels AA et al (2019) Health-related quality of life as predictor of mortality in end-stage renal disease patients: an observational study. BMC Nephrol 20:144. https://doi.org/10.1186/s12882-019-1318-x
Eneanya ND, Maddux DW, Reviriego-Mendoza MM et al (2019) Longitudinal patterns of health-related quality of life and dialysis modality: a national cohort study. BMC Nephrol 20:7. https://doi.org/10.1186/s12882-018-1198-5
Ulutas O, Farragher J, Chiu E et al (2016) Functional disability in older adults maintained on peritoneal dialysis therapy. Perit Dial Int 36:71–78. https://doi.org/10.3747/pdi.2013.00293
Jassal SV, Karaboyas A, Comment LA et al (2016) Functional dependence and mortality in the international dialysis outcomes and practice patterns study (DOPPS). Am J Kidney Dis 67:283–292. https://doi.org/10.1053/j.ajkd.2015.09.024
Manera KE, Tong A, Craig JC et al (2019) An international Delphi survey helped develop consensus-based core outcome domains for trials in peritoneal dialysis. Kidney Int 96:699–710. https://doi.org/10.1016/j.kint.2019.03.015
Portela OT, Belasco AGS, Casarin BF et al (2020) Quality of life and cognitive and functional performance of octogenarians and nonagenarians undergoing hemodialysis. Int Urol Nephrol 52:179–185. https://doi.org/10.1007/s11255-019-02323-x
Goto NA, van Loon IN, Morpey MI et al (2019) Geriatric assessment in elderly patients with end-stage kidney disease. Nephron 141:41–48. https://doi.org/10.1159/000494222
Gill TM, Robison JT, Tinetti ME (1997) Predictors of recovery in activities of daily living among disabled older persons living in the community. J Gen Intern Med 12(12):757–762
Wang DXM, Yao J, Zirek Y et al (2020) Muscle mass, strength, and physical performance predicting activities of daily living: a meta-analysis. J Cachexia Sarcopenia Muscle 11:3–25
Balogun S, Winzenberg T, Wills K et al (2019) Prospective associations of low muscle mass and strength with health-related quality of life over 10-year in community-dwelling older adults. Exp Gerontol 118:65–71
Penninx BW, Guralnik JM, Ferrucci L et al (1998) (1998) Depressive symptoms and physical decline in community-dwelling older persons. JAMA 279:1720–1726. https://doi.org/10.1001/jama.279.21.1720
Sivertsen H, Bjorklof GH, Engedal K et al (2015) Depression and quality of life in older persons: a review. Dement Geriatr Cogn Disord 40:311–339. https://doi.org/10.1159/000437299
Zhang M, Kim JC, Li Y et al (2014) Relation between anxiety, depression, and physical activity and performance in maintenance hemodialysis patients. J Ren Nutr 24:252–260. https://doi.org/10.1053/j.jrn.2014.03.002
Belayev LY, Mor MK, Sevick MA et al (2015) Longitudinal associations of depressive symptoms and pain with quality of life in patients receiving chronic hemodialysis. Hemodial Int 19:216–224. https://doi.org/10.1111/hdi.12247
Li H, Jia J, Yang Z (2016) Mini-mental state examination in elderly Chinese: a population-based normative study. J Alzheimers Dis 53:487–496
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30:473–483
Li L, Wang H, Shen Y (2002) Development and psychometric tests of a Chinese version of the SF-36 health survey scales. Chin J Prev Med 36:109–113
Brown LM, Schinka JA (2005) Development and initial validation of a 15-item informant version of the Geriatric Depression Scale. Int J Geriatr Psychiatry 20:911–918. https://doi.org/10.1002/gps.1375
Balogun RA, Balogun SA, Kepple AL et al (2011) The 15-item geriatric depression scale as a predictor of mortality in older adults undergoing hemodialysis. J Am Geriatr Soc 59:1563–1565. https://doi.org/10.1111/j.1532-5415.2011.03533.x
Yoo W, Mayberry R, Bae S (2014) A study of effects of multicollinearity in the multivariable analysis. Int J Appl Sci Technol 3:9–19
Brach JS, VanSwearingen JM, Newman AB et al (2002) Identifying early decline of physical function in community-dwelling older women: performance-based and self-report measures. Phys Ther 82:320–328. https://doi.org/10.1111/ggi.12379
Matsuzawa R, Kamitani T, Roshanravan B et al (2019) Decline in the functional status and mortality in patients on hemodialysis: results from the Japan dialysis outcome and practice patterns study. J Ren Nutr 29:504–510. https://doi.org/10.1053/j.jrn.2018.10.012
Iyasere O, Brown EA, Johansson L et al (2019) Quality of life with conservative care compared with assisted peritoneal dialysis and haemodialysis. Clin Kidney J 12:262–268. https://doi.org/10.1093/ckj/sfy059
Shah KK, Murtagh FEM, McGeechan K et al (2019) Health-related quality of life and well-being in people over 75 years of age with end-stage kidney disease managed with dialysis or comprehensive conservative care: a cross-sectional study in the UK and Australia. BMJ Open 9:e027776. https://doi.org/10.1136/bmjopen-2018-027776
Rogan A, McCarthy K, McGregor G et al (2017) Quality of life measures predict cardiovascular health and physical performance in chronic renal failure patients. PLoS ONE 12:e0183926. https://doi.org/10.1371/journal.pone.0183926
Laegreid IK, Aasarod K, Bye A et al (2014) The impact of nutritional status, physical function, comorbidity and early versus late start in dialysis on quality of life in older dialysis patients. Ren Fail 36:9–16. https://doi.org/10.3109/0886022x.2013.830206
Ekstrom H, Dahlin-Ivanoff S, Elmstahl S (2011) Effects of walking speed and results of timed get-up-and-go tests on quality of life and social participation in elderly individuals with a history of osteoporosis-related fractures. J Aging Health 23:1379–1399. https://doi.org/10.1177/0898264311418504
Everard KM, Lach HW, Fisher EB et al (2000) Relationship of activity and social support to the functional health of older adults. J Gerontol B Psychol Sci Soc Sci 55:S208-212. https://doi.org/10.1093/geronb/55.4.s208
Frih B, Jaafar H, Mkacher W et al (2017) The effect of interdialytic combined resistance and aerobic exercise training on health related outcomes in chronic hemodialysis patients: the Tunisian randomized controlled study. Front Physiol 8:288. https://doi.org/10.3389/fphys.2017.00288
Tao X, Chow SKY, Zhang H et al (2020) Family caregiver’s burden and the social support for older patients undergoing peritoneal dialysis. J Ren Care. https://doi.org/10.1111/jorc.12322
Blazer DG (2003) Depression in late life: review and commentary. J Gerontol Ser A Biol Sci Med Sci 58:249–265. https://doi.org/10.1093/gerona/58.3.m249
Senol V, Sipahioglu MH, Ozturk A et al (2010) Important determinants of quality of life in a peritoneal dialysis population in Turkey. Ren Fail 32:1196–1201. https://doi.org/10.3109/0886022x.2010.517349
Wedding U, Koch A, Rohrig B et al (2008) Depression and functional impairment independently contribute to decreased quality of life in cancer patients prior to chemotherapy. Acta Oncol 47:56–62. https://doi.org/10.1080/02841860701460541
King-Wing MT, Kam-Tao LP (2016) Depression in dialysis patients. Nephrology (Carlton) 21:639–646. https://doi.org/10.1111/nep.12742
Einwohner R, Bernardini J, Fried L et al (2004) The effect of depressive symptoms on survival in peritoneal dialysis patients. Perit Dial Int 24:256–263
Liebman S, Li NC, Lacson E (2016) Change in quality of life and one-year mortality risk in maintenance dialysis patients. Qual Life Res 25:2295–2306. https://doi.org/10.1007/s11136-016-1257-y
Rambod M, Kovesdy CP, Bross R et al (2008) Association of serum prealbumin and its changes over time with clinical outcomes and survival in patients receiving hemodialysis. Am J Clin Nutr 88:1485–1494. https://doi.org/10.3945/ajcn.2008.25906
Chertow GM, Goldstein-Fuchs DJ, Lazarus JM et al (2005) Prealbumin, mortality, and cause-specific hospitalization in hemodialysis patients. Kidney Int 68:2794–2800. https://doi.org/10.1111/j.1523-1755.2005.00751.x
Marsen TA, Beer J, Mann H (2017) Intradialytic parenteral nutrition in maintenance hemodialysis patients suffering from protein-energy wasting. Results of a multicenter, open, prospective, randomized trial. Clin Nutr 36:107–117. https://doi.org/10.1016/j.clnu.2015.11.016
Gharekhani A, Khatami MR, Dashti-Khavidaki S et al (2014) Effects of oral supplementation with omega-3 fatty acids on nutritional state and inflammatory markers in maintenance hemodialysis patients. J Ren Nutr 24:177–185. https://doi.org/10.1053/j.jrn.2014.01.014
Johansson L, Fouque D, Bellizzi V et al (2017) As we grow old: nutritional considerations for older patients on dialysis. Nephrol Dial Transplant 32:1127–1136. https://doi.org/10.1093/ndt/gfw201
Fouque D, Kalantar-Zadeh K, Kopple J et al (2008) A proposed nomenclature and diagnostic criteria for protein-energy wasting in acute and chronic kidney disease. Kidney Int 73:391–398. https://doi.org/10.1038/sj.ki.5002585
Kim JR, Kim HN, Song SW (2018) Associations among inflammation, mental health, and quality of life in adults with metabolic syndrome. Diabetol Metab Syndr 10:66. https://doi.org/10.1186/s13098-018-0367-9
Ko GJ, Kim MG, Yu YM et al (2010) Association between depression symptoms with inflammation and cardiovascular risk factors in patients undergoing peritoneal dialysis. Nephron Clin Pract 116:c29-35. https://doi.org/10.1159/000314548
Dantzer R, O’Connor JC, Freund GG et al (2008) From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci 9:46–56. https://doi.org/10.1038/nrn2297
Guenzani D, Buoli M, Caldiroli L et al (2019) Malnutrition and inflammation are associated with severity of depressive and cognitive symptoms of old patients affected by chronic kidney disease. J Psychosom Res 124:109783. https://doi.org/10.1016/j.jpsychores.2019.109783
Gaskins AJ, Wilchesky M, Mumford SL et al (2012) Endogenous reproductive hormones and C-reactive protein across the menstrual cycle: the BioCycle study. Am J Epidemiol 175:423–431. https://doi.org/10.1093/aje/kwr343
Anees M, Malik MR, Abbasi T et al (2014) Demographic factors affecting quality of life of hemodialysis patients—Lahore, Pakistan. Pak J Med Sci 30:1123–1127. https://doi.org/10.12669/pjms.305.5239
Rosa CS, Bueno DR, Souza GD et al (2015) Factors associated with leisure-time physical activity among patients undergoing hemodialysis. BMC Nephrol 16:192. https://doi.org/10.1186/s12882-015-0183-5
Acknowledgements
The authors thank all the patients who participated in this study.
Funding
This study was funded by the National Natural Science Foundation of China (Grant no. 71704105).
Author information
Authors and Affiliations
Contributions
XJT, YY, and HFZ: conceived and designed the study. XJT, YY, and HFZ: managed the whole study. XJT, YY, HFZ, JYH, APG, NL, YNH, and YJ: participated in design and coordination, data collection and analysis, and reading and approval of the final manuscript. XJT and YY: drafted the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee (Public Health and Nursing Research Ethics Committee of Shanghai Jiao Tong University, SJUPN-201705), and in compliance with the 1964 Helsinki Declaration.
Informed consent
Written informed consent was obtained from all individual participants included in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tao, X., Zhang, H., Huang, J. et al. Physical performance and health-related quality of life among older adults on peritoneal dialysis: a cross-sectional study. Int Urol Nephrol 53, 1033–1042 (2021). https://doi.org/10.1007/s11255-020-02737-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-020-02737-y