Abstract
Background
A precise description of renal histological lesions and an appropriate classification of lupus nephritis are both essential for nephrologists to guide treatment and predict prognosis among patients. The prognostic value of ISN/RPS 2003 classification is controversial. A new classification for lupus nephritis was recently proposed, namely, the revised ISN/RPS 2018 classification.
Objective
The study aimed to evaluate the predictive value of the clinical and pathological factors according to ISN/RPS 2018 classification on renal remission among patients with proliferative lupus nephritis.
Methods
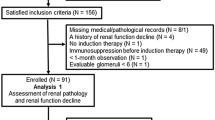
A total number of 41 patients with proliferative lupus nephritis on adequate renal biopsy specimen between 2017 and 2018 were included. Clinical and histological variables were tested for their association with renal remission. Univariate and multivariate logistic regression analysis were performed to identify independent predictors of renal remission after 24 weeks of induction therapy.
Results
After induction therapy, 56.1% of patients reached complete and partial remission and 43.9% reached no remission. In univariate analyses, baseline glomerular filtration rate (GFR), presence of anti-DNA titer, cellular crescents, interstitial inflammation, glomerulosclerosis, interstitial fibrosis, tubular atrophy and total chronicity index strongly impacted renal response. After multivariate logistic regression analysis, we identified aging, presence of cellular crescents, and high total renal chronicity index as independent predictors of renal remission. Receiver operating characteristic (ROC) analysis revealed that baseline estimated GFR (AUC = 0.708; 95% CI 0.527–0.888), anti-DNA titer (AUC = 0.674; 95% CI 0.491–0.858), cellular crescent (AUC = 0.750; 95% CI 0.585–0.915) and renal chronicity index (AUC = 0.765; 95% CI 0.585–0.915) predicted renal remission. Combining all factors achieved a perfect score predicting renal response (AUC 0.924; 95% CI 0.840–1.000).
Conclusion
The study identified baseline GFR, anti-DNA titer, cellular crescent, and high chronicity index according to revised ISN/RPS 2018 classification as important predictors of renal response after induction therapy in proliferative lupus nephritis.

Similar content being viewed by others
Availability of data and materials
Data supporting this study are available upon request.
References
Bernatsky S, Boivin JF, Joseph L, Manzi S, Ginzler E, Gladman DD, Urowitz M, Fortin PR, Petri M, Barr S, Gordon C, Bae SC, Isenberg D, Zoma A, Aranow C, Dooley MA, Nived O, Sturfelt G, Steinsson K, Alarcon G, Senecal JL, Zummer M, Hanly J, Ensworth S, Pope J, Edworthy S, Rahman A, Sibley J, El-Gabalawy H, McCarthy T, St Pierre Y, Clarke A, Ramsey-Goldman R (2006) Mortality in systemic lupus erythematosus. Arthritis Rheum 54(8):2550–2557. https://doi.org/10.1002/art.21955
Parikh SV, Rovin BH (2016) Current and emerging therapies for lupus nephritis. J Am Soc Nephrol 27(10):2929–2939. https://doi.org/10.1681/ASN.2016040415
Satirapoj B, Tasanavipas P, Supasyndh O (2015) Clinicopathological correlation in Asian patients with biopsy-proven lupus nephritis. Int J Nephrol 2015:857316. https://doi.org/10.1155/2015/857316
Najafi CC, Korbet SM, Lewis EJ, Schwartz MM, Reichlin M, Evans J, Lupus Nephritis Collaborative Study G (2001) Significance of histologic patterns of glomerular injury upon long-term prognosis in severe lupus glomerulonephritis. Kidney Int 59(6):2156–2163. https://doi.org/10.1046/j.1523-1755.2001.00730.x
Markowitz GS, D’Agati VD (2009) Classification of lupus nephritis. Curr Opin Nephrol Hypertens 18(3):220–225. https://doi.org/10.1097/mnh.0b013e328327b379
Yokoyama H, Wada T, Hara A, Yamahana J, Nakaya I, Kobayashi M, Kitagawa K, Kokubo S, Iwata Y, Yoshimoto K, Shimizu K, Sakai N, Furuichi K, Kanazawa Study Group for Renal D, Hypertension (2004) The outcome and a new ISN/RPS 2003 classification of lupus nephritis in Japanese. Kidney Int 66(6):2382–2388. https://doi.org/10.1111/j.1523-1755.2004.66027.x
Hiramatsu N, Kuroiwa T, Ikeuchi H, Maeshima A, Kaneko Y, Hiromura K, Ueki K, Nojima Y (2008) Revised classification of lupus nephritis is valuable in predicting renal outcome with an indication of the proportion of glomeruli affected by chronic lesions. Rheumatology (Oxford) 47(5):702–707. https://doi.org/10.1093/rheumatology/ken019
Wilhelmus S, Alpers CE, Cook HT, Ferrario F, Fogo AB, Haas M, Joh K, Noel LH, Seshan SV, Bruijn JA, Bajema IM (2015) The revisited classification of GN in SLE at 10 years: time to re-evaluate histopathologic lesions. J Am Soc Nephrol 26(12):2938–2946. https://doi.org/10.1681/ASN.2015040384
Rijnink EC, Teng YKO, Wilhelmus S, Almekinders M, Wolterbeek R, Cransberg K, Bruijn JA, Bajema IM (2017) Clinical and histopathologic characteristics associated with renal outcomes in lupus nephritis. Clin J Am Soc Nephrol 12(5):734–743. https://doi.org/10.2215/CJN.10601016
Bajema IM, Wilhelmus S, Alpers CE, Bruijn JA, Colvin RB, Cook HT, D’Agati VD, Ferrario F, Haas M, Jennette JC, Joh K, Nast CC, Noel LH, Rijnink EC, Roberts ISD, Seshan SV, Sethi S, Fogo AB (2018) Revision of the International Society of Nephrology/Renal Pathology Society classification for lupus nephritis: clarification of definitions, and modified National Institutes of Health activity and chronicity indices. Kidney Int 93(4):789–796. https://doi.org/10.1016/j.kint.2017.11.023
Chen YE, Korbet SM, Katz RS, Schwartz MM, Lewis EJ, Collaborative Study G (2008) Value of a complete or partial remission in severe lupus nephritis. Clin J Am Soc Nephrol 3(1):46–53. https://doi.org/10.2215/CJN.03280807
Radhakrishnan J, Cattran DC (2012) The KDIGO practice guideline on glomerulonephritis: reading between the (guide) lines–application to the individual patient. Kidney Int 82(8):840–856. https://doi.org/10.1038/ki.2012.280
Pagni F, Galimberti S, Goffredo P, Basciu M, Malachina S, Pilla D, Galbiati E, Ferrario F (2013) The value of repeat biopsy in the management of lupus nephritis: an international multicentre study in a large cohort of patients. Nephrol Dial Transplant 28(12):3014–3023. https://doi.org/10.1093/ndt/gft272
Tesar V, Hruskova Z (2017) Understanding histolopathologic characteristics to predict renal outcomes in lupus nephritis. Clin J Am Soc Nephrol 12(5):711–712. https://doi.org/10.2215/CJN.03490317
Dasari S, Chakraborty A, Truong L, Mohan C (2019) A systematic review of interpathologist agreement in histologic classification of lupus nephritis. Kidney Int Rep 4(10):1420–1425. https://doi.org/10.1016/j.ekir.2019.06.011
Oni L, Beresford MW, Witte D, Chatzitolios A, Sebire N, Abulaban K, Shukla R, Ying J, Brunner HI (2017) Inter-observer variability of the histological classification of lupus glomerulonephritis in children. Lupus 26(11):1205–1211. https://doi.org/10.1177/0961203317706558
Mavragani CP, Fragoulis GE, Somarakis G, Drosos A, Tzioufas AG, Moutsopoulos HM (2015) Clinical and laboratory predictors of distinct histopathogical features of lupus nephritis. Medicine (Baltimore) 94(21):e829. https://doi.org/10.1097/MD.0000000000000829
Wernick RM, Smith DL, Houghton DC, Phillips DS, Booth JL, Runckel DN, Johnson DS, Brown KK, Gaboury CL (1993) Reliability of histologic scoring for lupus nephritis: a community-based evaluation. Ann Intern Med 119(8):805–811. https://doi.org/10.7326/0003-4819-119-8-199310150-00006
Appel GB, Cohen DJ, Pirani CL, Meltzer JI, Estes D (1987) Long-term follow-up of patients with lupus nephritis. A study based on the classification of the World Health Organization. Am J Med 83(5):877–885
Chen DN, Fan L, Wu YX, Zhou Q, Chen W, Yu XQ (2018) A predictive model for estimation risk of proliferative lupus nephritis. Chin Med J (Engl) 131(11):1275–1281. https://doi.org/10.4103/0366-6999.232809
Rush PJ, Baumal R, Shore A, Balfe JW, Schreiber M (1986) Correlation of renal histology with outcome in children with lupus nephritis. Kidney Int 29(5):1066–1071. https://doi.org/10.1038/ki.1986.108
Austin HA 3rd, Muenz LR, Joyce KM, Antonovych TT, Balow JE (1984) Diffuse proliferative lupus nephritis: identification of specific pathologic features affecting renal outcome. Kidney Int 25(4):689–695. https://doi.org/10.1038/ki.1984.75
Chan TM, Tse KC, Tang CS, Lai KN, Li FK (2005) Long-term outcome of patients with diffuse proliferative lupus nephritis treated with prednisolone and oral cyclophosphamide followed by azathioprine. Lupus 14(4):265–272. https://doi.org/10.1191/0961203305lu2081oa
Ding Y, Nie LM, Pang Y, Wu WJ, Tan Y, Yu F, Zhao MH (2018) Composite urinary biomarkers to predict pathological tubulointerstitial lesions in lupus nephritis. Lupus 27(11):1778–1789. https://doi.org/10.1177/0961203318788167
Obrisca B, Jurubita R, Andronesi A, Sorohan B, Achim C, Bobeica R, Gherghiceanu M, Mandache E, Ismail G (2018) Histological predictors of renal outcome in lupus nephritis: the importance of tubulointerstitial lesions and scoring of glomerular lesions. Lupus 27(9):1455–1463. https://doi.org/10.1177/0961203318776109
Wagrowska-Danilewicz M, Danilewicz M (2014) Clinicopathological characteristics of segmental (IV-S) and global (IV-G) active subclasses of class IV lupus nephritis: a comparative study. Pol J Pathol 65(3):223–228. https://doi.org/10.5114/pjp.2014.45786
Markowitz GS, D’Agati VD (2007) The ISN/RPS 2003 classification of lupus nephritis: an assessment at 3 years. Kidney Int 71(6):491–495. https://doi.org/10.1038/sj.ki.5002118
Yu F, Wu LH, Tan Y, Li LH, Wang CL, Wang WK, Qu Z, Chen MH, Gao JJ, Li ZY, Zheng X, Ao J, Zhu SN, Wang SX, Zhao MH, Zou WZ, Liu G (2010) Tubulointerstitial lesions of patients with lupus nephritis classified by the 2003 International Society of Nephrology and Renal Pathology Society system. Kidney Int 77(9):820–829. https://doi.org/10.1038/ki.2010.13
Yu F, Tan Y, Liu G, Wang SX, Zou WZ, Zhao MH (2009) Clinicopathological characteristics and outcomes of patients with crescentic lupus nephritis. Kidney Int 76(3):307–317. https://doi.org/10.1038/ki.2009.136
Satirapoj B, Kitiyakara C, Leelahavanichkul A, Avihingsanon Y, Supasyndh O (2017) Urine neutrophil gelatinase-associated lipocalin to predict renal response after induction therapy in active lupus nephritis. BMC Nephrol 18(1):263. https://doi.org/10.1186/s12882-017-0678-3
Park DJ, Choi SE, Xu H, Kang JH, Lee KE, Lee JS, Choi YD, Lee SS (2018) Chronicity index, especially glomerular sclerosis, is the most powerful predictor of renal response following immunosuppressive treatment in patients with lupus nephritis. Int J Rheum Dis 21(2):458–467. https://doi.org/10.1111/1756-185X.13254
Acknowledgements
The authors wish to acknowledge the contributions of the following individuals to this study: staff in the Division of Nephrology and Division of Pathology in Phramongkutklao Hospital.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval
The study was approved by the Ethics Committee of the Institute Review Board at the Royal Thai Army Medical Department and was conducted according to the Declaration of Helsinki.
Informed consent
Informed consent was obtained from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Krassanairawiwong, K., Charoenpitakchai, M., Supasyndh, O. et al. Revised ISN/RPS 2018 classification of lupus renal pathology predict clinical remission. Int Urol Nephrol 53, 1391–1398 (2021). https://doi.org/10.1007/s11255-020-02732-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-020-02732-3