Abstract
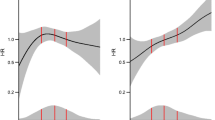
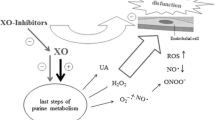
Kynurenine pathway of tryptophan metabolism is involved in the pathophysiology of chronic kidney disease (CKD) and diabetes mellitus, mainly through the inflammation-induced activity of indoleamine 2,3-dioxygenase (IDO), and few studies have investigated its potential link with proteinuria. Renin–angiotensin system inhibitors (RASis) are recommended in these patients to decrease proteinuria, slow CKD progression and reduce cardiovascular risk, but whether these drugs influence kynurenine levels in humans is unknown. We evaluated serum tryptophan and kynurenine in patients suffering from CKD with or without type 2 diabetes mellitus, their correlations with markers of reduced kidney function, and their relationship with RAS-inhibiting therapy. Of 72 adult patients enrolled, 55 were receiving RASis, whereas 17 were not. Tryptophan was assessed by HPLC (high-performance liquid chromatography); kynurenine was measured using an enzyme-linked immunosorbent assay kit; IDO activity (%) was calculated with the formula (kynurenine/tryptophan) × 100. Kynurenine levels were significantly lower in the group under RASis compared to the untreated group (1.56 ± 0.79 vs 2.16 ± 1.51 µmol/l; P = 0.0378). In patients not receiving RASis, kynurenine was inversely related to estimated glomerular filtration rate (eGFR) (r = − 0.4862; P = 0.0478) and directly related to both proteinuria (ρ = 0.493; P = 0.0444) and albuminuria (ρ = 0.542; P = 0.0247). IDO activity was higher in patients with history of cardiovascular disease compared to patients with no such history, and it negatively correlated with eGFR (ρ = − 0.554; P = 0.0210) in the same group. These findings may contribute to explain the well-known beneficial effects of RAS inhibition in CKD population, especially considering that kynurenine is emerging as a potential new biomarker of CKD.








Similar content being viewed by others
References
Cernaro V, Medici MA, Leonello G et al (2015) Auxin induces cell proliferation in an experimental model of mammalian renal tubular epithelial cells. Ren Fail 37(5):911–913
Law KP, Zhang H (2017) The pathogenesis and pathophysiology of gestational diabetes mellitus: deductions from a three-part longitudinal metabolomics study in China. Clin Chim Acta 468:60–70
Schwarcz R, Bruno JP, Muchowski PJ et al (2012) Kynurenines in the mammalian brain: when physiology meets pathology. Nat Rev Neurosci 13(7):465–477
Oxenkrug GF (2007) Genetic and hormonal regulation of tryptophan kynurenine metabolism: implications for vascular cognitive impairment, major depressive disorder, and aging. Ann N Y Acad Sci 1122:35–49
Jayawickrama GS, Nematollahi A, Sun G et al (2018) Improvement of kynurenine aminotransferase-II inhibitors guided by mimicking sulfate esters. PLoS ONE 13(4):e0196404
Larkin PB, Sathyasaikumar KV, Notarangelo FM et al (2016) Tryptophan 2,3-dioxygenase and indoleamine 2,3-dioxygenase 1 make separate, tissue-specific contributions to basal and inflammation-induced kynurenine pathway metabolism in mice. Biochim Biophys Acta 1860(11 Pt A):2345–2354
Oxenkrug G (2013) Insulin resistance and dysregulation of tryptophan-kynurenine and kynurenine-nicotinamide adenine dinucleotide metabolic pathways. Mol Neurobiol 48(2):294–301
Debnath S, Velagapudi C, Redus L et al (2017) Tryptophan metabolism in patients with chronic kidney disease secondary to type 2 diabetes: relationship to inflammatory markers. Int J Tryptophan Res 10:1178646917694600
Schefold JC, Zeden JP, Fotopoulou C et al (2009) Increased indoleamine 2,3-dioxygenase (IDO) activity and elevated serum levels of tryptophan catabolites in patients with chronic kidney disease: a possible link between chronic inflammation and uraemic symptoms. Nephrol Dial Transplant 24(6):1901–1908
Vanholder R, De Smet R, Glorieux G et al (2003) Review on uremic toxins: classification, concentration, and interindividual variability. Kidney Int 63(5):1934–1943
Korstanje R, Deutsch K, Bolanos-Palmieri P et al (2016) Loss of kynurenine 3-mono-oxygenase causes proteinuria. J Am Soc Nephrol 27(11):3271–3277
Hirayama A, Nakashima E, Sugimoto M et al (2012) Metabolic profiling reveals new serum biomarkers for differentiating diabetic nephropathy. Anal Bioanal Chem 404(10):3101–3109
Group KDIGOKCW (2013) KDIGO clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl 3(1):1–150
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612
Zhang Y, Ruan Y, Zhang P et al (2017) Increased indoleamine 2,3-dioxygenase activity in type 2 diabetic nephropathy. J Diabetes Complicat 31(1):223–227
Atlas SA (2007) The renin–angiotensin aldosterone system: pathophysiological role and pharmacologic inhibition. J Manag Care Pharm. 13(8 Suppl B):9–20
Pacurari M, Kafoury R, Tchounwou PB et al (2014) The Renin–Angiotensin–aldosterone system in vascular inflammation and remodeling. Int J Inflam 2014:689360
Nishiyama A, Kim-Mitsuyama S (2010) New approaches to blockade of the renin-angiotensin-aldosterone system: overview of regulation of the renin–angiotensin-aldosterone system. J Pharmacol Sci 113(4):289–291
Roscioni SS, Heerspink HJ, de Zeeuw D (2014) The effect of RAAS blockade on the progression of diabetic nephropathy. Nat Rev Nephrol 10(2):77–87
Cernaro V, Trifirò G, Lorenzano G et al (2014) New therapeutic strategies under development to halt the progression of renal failure. Expert Opin Investig Drugs 23(5):693–709
Lytvyn Y, Bjornstad P, Pun N et al (2016) New and old agents in the management of diabetic nephropathy. Curr Opin Nephrol Hypertens 25(3):232–239
Mair RD, Sirich TL, Meyer TW (2018) Uremic toxin clearance and cardiovascular toxicities. Toxins (Basel) 10(6):226
Bartosiewicz J, Kaminski T, Pawlak K et al (2017) The activation of the kynurenine pathway in a rat model with renovascular hypertension. Exp Biol Med (Maywood) 242(7):750–761
Zakrocka I, Kocki T, Turski WA (2017) The effect of three angiotensin-converting enzyme inhibitors on kynurenic acid production in rat kidney in vitro. Pharmacol Rep 69(3):536–541
Zakrocka I, Targowska-Duda KM, Wnorowski A et al (2019) Angiotensin II type 1 receptor blockers decrease kynurenic acid production in rat kidney in vitro. Naunyn Schmiedebergs Arch Pharmacol 392(2):209–217
Widner B, Werner ER, Schennach H et al (1997) Simultaneous measurement of serum tryptophan and kynurenine by HPLC. Clin Chem 43(12):2424–2426
Badawy AA, Dougherty DM (2016) Assessment of the human kynurenine pathway: comparisons and clinical implications of ethnic and gender differences in plasma tryptophan, kynurenine metabolites, and enzyme expressions at baseline and after acute tryptophan loading and depletion. Int J Tryptophan Res 9:31–49
Baratta AM, Buck SA, Buchla AD et al (2018) Sex differences in hippocampal memory and kynurenic acid formation following acute sleep deprivation in rats. Sci Rep 8(1):6963
Chauvel V, Schoenen J, Multon S (2013) Influence of ovarian hormones on cortical spreading depression and its suppression by l-kynurenine in rat. PLoS ONE 8(12):e82279
Fertan E, Stover KRJ, Brant MG et al (2019) Effects of the novel IDO inhibitor DWG-1036 on the behavior of male and female 3xTg-AD mice. Front Pharmacol 10:1044
Meier TB, Drevets WC, Teague TK et al (2018) Kynurenic acid is reduced in females and oral contraceptive users: Implications for depression. Brain Behav Immun 67:59–64
Reininghaus EZ, Dalkner N, Riedrich K et al (2019) Sex specific changes in tryptophan breakdown over a 6 week treatment period. Front Psychiatry 10:74
Songtachalert T, Roomruangwong C, Carvalho AF et al (2018) Anxiety disorders: sex differences in serotonin and tryptophan metabolism. Curr Top Med Chem 18(19):1704–1715
Naz S, Bhat M, Stahl S et al (2019) Dysregulation of the tryptophan pathway evidences gender differences in COPD. Metabolites 9(10):212
Sas K, Szabo E, Vecsei L (2018) Mitochondria, oxidative stress and the kynurenine system, with a focus on ageing and neuroprotection. Molecules 23(1):191
Oxenkrug GF (2010) Metabolic syndrome, age-associated neuroendocrine disorders, and dysregulation of tryptophan-kynurenine metabolism. Ann N Y Acad Sci 1199:1–14
Pawlak K, Domaniewski T, Mysliwiec M et al (2009) The kynurenines are associated with oxidative stress, inflammation and the prevalence of cardiovascular disease in patients with end-stage renal disease. Atherosclerosis 204(1):309–314
Silva RE, Baldim JL, Chagas-Paula DA et al (2018) Predictive metabolomic signatures of end-stage renal disease: a multivariate analysis of population-based data. Biochimie 152:14–30
Canadas-Garre M, Anderson K, McGoldrick J et al (2019) Proteomic and metabolomic approaches in the search for biomarkers in chronic kidney disease. J Proteomics 193:93–122
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Research involving human participants
There is no research involving human participants.
Informed consent
Written informed consent was obtained from all recruited patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cernaro, V., Loddo, S., Macaione, V. et al. RAS inhibition modulates kynurenine levels in a CKD population with and without type 2 diabetes mellitus. Int Urol Nephrol 52, 1125–1133 (2020). https://doi.org/10.1007/s11255-020-02469-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-020-02469-z