Abstract
Objective
To explore the correlation between body composition measurement by bioelectrical impedance analysis (BIA) and intradialytic hypotension (IDH).
Methods
The clinical data of 127 patients with end-stage renal disease (ESRD) who underwent regular dialysis in the Blood Purification Center of the Second Affiliated Hospital of Chongqing Medical University were retrospectively analyzed. According to the occurrence of IDH, the patients were divided into IDH group and intradialytic normotension group. The difference in body composition measured by BIA and its relationship with IDH were compared between the two groups.
Results
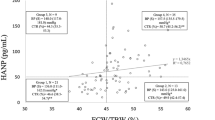
Compared with intradialytic normotension group, the intracellular water (ICW) ratio (P = 0.009), extracellular water (ECW) ratio (P = 0.029), total body water (TBW) ratio (P = 0.012), protein ratio (P = 0.010), soft lean mass (SLM) ratio (P = 0.011), fat-free mass (FFM) ratio (P = 0.012) and skeletal muscle mass (SMM) ratio (P = 0.009) in IDH group were significantly decreased. However, the fat mass (FM) ratio (P = 0.016), percentage body fat (PBF) ratio (P = 0.001), extracellular water/total body water (ECW/TBW) ratio (P = 0.036), extracellular water/total body water in trunk (ECW/TBWT) ratio (P = 0.045) and visceral fat area (VFA) (P = 0.003) in IDH group were significantly increased when compared with intradialytic normotension group. In addition, there was a positive correlation between systolic blood pressure (SBP) during IDH and ECW ratio, ECW/TBW ratio, and ECW/TBWTR ratio before dialysis.
Conclusions
The body composition of dialysis patients is closely related to the occurrence of IDH. Strengthening the body composition management of dialysis patients outside the hospital may reduce the occurrence of IDH and improve the long-term prognosis of dialysis patients.

Similar content being viewed by others
References
McIntyre CW, Goldsmith DJ (2015) Ischemic brain injury in hemodialysis patients: which is more dangerous, hypertension or intradialytic hypotension? Kidney Int 87(6):1109–1115
Daugirdas JT (2015) Measuring intradialytic hypotension to improve quality of care. J Am Soc Nephrol 26(3):512–514
Lertdumrongluk P, Streja E, Rhee CM, Sim JJ, Gillen D, Kovesdy CP, Kalantar-Zadeh K (2015) Changes in pulse pressure during hemodialysis treatment and survival in maintenance dialysis patients. Clin J Am Soc Nephrol 10(7):1179–1191
Chou JA, Kalantar-Zadeh K, Mathew AT (2017) A brief review of intradialytic hypotension with a focus on survival. Semin Dial 30(6):473–480
Dasgupta I, Thomas GN, Clarke J, Sitch A, Martin J, Bieber B, Hecking M, Karaboyas A, Pisoni R, Port F, Robinson B, Rayner H (2019) Associations between hemodialysis facility practices to manage fluid volume and intradialytic hypotension and patient outcomes. Clin J Am Soc Nephrol 14(3):385–393
Burton JO, Jefferies HJ, Selby NM, McIntyre CW (2009) Hemodialysis-induced cardiac injury: determinants and associated outcomes. Clin J Am Soc Nephrol 4(5):914–920
Flythe JE, Xue H, Lynch KE, Curhan GC, Brunelli SM (2015) Association of mortality risk with various definitions of intradialytic hypotension. J Am Soc Nephrol 26(3):724–734
Maurer C, Wagner JY, Schmid RM, Saugel B (2017) Assessment of volume status and fluid responsiveness in the emergency department: a systematic approach. Med Klin Intensivmed Notfmed 112(4):326–333
Lim PS, Chen CH, Zhu F, Kotanko P, Jeng Y, Hu CY, Chiu LS, Chang HC (2017) Validating body fat assessment by bioelectric impedance spectroscopy in Taiwanese hemodialysis patients. J Renal Nutr 27(1):37–44
Chamney PW, Wabel P, Moissl UM, Müller MJ, Bosy-Westphal A, Korth O, Fuller NJ (2007) A whole-body model to distinguish excess fluid from the hydration of major body tissues. Am J Clin Nutr 85(1):80–89
Kang SH, Choi EW, Park JW, Cho KH, Do JY (2016) Clinical significance of the edema index in incident peritoneal dialysis patients. PLoS ONE 11(1):e0147070
O'Lone EL, Visser A, Finney H, Fan SL (2014) Clinical significance of multi-frequency bioimpedance spectroscopy in peritoneal dialysis patients: independent predictor of patient survival. Nephrol Dial Transplant 29(7):1430–1437
Ng JK, Kwan BC, Chow KM, Pang WF, Cheng PM, Leung CB, Li PK, Szeto CC (2018) Asymptomatic fluid overload predicts survival and cardiovascular event in incident Chinese peritoneal dialysis patients. PLoS ONE 13(8):e0202203
Wanner C, Amann K, Shoji T (2016) The heart and vascular system in dialysis. Lancet 388(10041):276–284
Ok E, Asci G, Chazot C, Ozkahya M, Mees EJ (2016) Controversies and problems of volume control and hypertension in haemodialysis. Lancet 388(10041):285–293
Kalantar-Zadeh K, Abbott KC, Salahudeen AK, Kilpatrick RD, Horwich TB (2005) Survival advantages of obesity in dialysis patients. Am J Clin Nutr 81(3):543–554
Johansen KL (2010) Association of body composition with survival among patients on hemodialysis. Clin J Am Soc Nephrol 5(12):2144–2145
Huang CX, Tighiouart H, Beddhu S, Cheung AK, Dwyer JT, Eknoyan G, Beck GJ, Levey AS, Sarnak MJ (2010) Both low muscle mass and low fat are associated with higher all-cause mortality in hemodialysis patients. Kidney Int 77(7):624–629
Kalantar-Zadeh K, Streja E, Kovesdy CP, Oreopoulos A, Noori N, Jing J, Nissenson AR, Krishnan M, Kopple JD, Mehrotra R, Anker SD (2010) The obesity paradox and mortality associated with surrogates of body size and muscle mass in patients receiving hemodialysis. Mayo Clin Proc 85(11):991–1001
Marcelli D, Usvyat LA, Kotanko P, Bayh I, Canaud B, Etter M, Gatti E, Grassmann A, Wang Y, Marelli C, Scatizzi L, Stopper A, van der Sande FM, Kooman J (2015) MONitoring Dialysis Outcomes (MONDO) Consortium: body composition and survival in dialysis patients: results from an international cohort study. Clin J Am Soc Nephrol 10(7):1192–1200
Noori N, Kopple JD, Kovesdy CP, Feroze U, Sim JJ, Murali SB, Luna A, Gomez M, Luna C, Bross R, Nissenson AR, Kalantar-Zadeh K (2010) Mid-arm muscle circumference and quality of life and survival in maintenance hemodialysis patients. Clin J Am Soc Nephrol 5(12):2258–2268
Acknowledgements
We would like to thank all Fellows and Staff of the Department of Nephrology, The Second Affiliated Hospital of Chongqing Medical University.
Funding
This work was supported by China Postdoctoral Science Foundation funded project (no. 2018M633630XB), Science and Technology Research Program of Chongqing Municipal Education Commission (Grant no. KJQN201800403), the National Natural Science Foundation of China (Grant no. 81800771) and the Chongqing Science and Technology Commission (cstc2019jcyj-msxm0195).The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Conceived and designed the study: JW, and LZ. Performed the experimental procedures: JC, SY. Analyzed the data: SX, QZ. Drafted the manuscript: QZ, JW.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Statement of ethics
This study was approved by the Ethics Committee of the Second Affiliated Hospital of Chongqing Medical University (No. (2019) 250). All persons recruited for this study provided written informed consent prior to participation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhou, Q., Wang, J., Xie, S. et al. Correlation between body composition measurement by bioelectrical impedance analysis and intradialytic hypotension. Int Urol Nephrol 52, 953–958 (2020). https://doi.org/10.1007/s11255-020-02456-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-020-02456-4