Abstract
Purpose
To design a dedicated risk calculator for patients with penile urethra stricture who are scheduled to urethroplasty that might be used to counsel patients according to their pre-operative risk of failure.
Methods
Patients treated with penile urethroplasty at our center (1994–2018) were included in the study. Patients received 1-stage or staged penile urethroplasty. Patients with failed hypospadias repair, lichen sclerosus or incomplete clinical records were excluded. Treatment failure was defined as any required postoperative instrumentation, including dilation. Univariable Cox regression identified predictors of post-operative treatment failure and Kaplan–Meier analysis plotted the failure-free survival rates according to such predictors. Multivariable Cox regression-based risk calculator was generated to predict the risk of treatment failure at 10 years after surgery.
Results
261 patients met the inclusion criteria. Median follow-up was 113 months. Out of 216 patients, 201 (77%) were classified as success and 60 (23%) failures. Former smoker (hazard ratio [HR] 2.12, p = 0.025), instrumentation-derived stricture (HR 2.55, p = 0.006), and use of grafts (HR 1.83, p = 0.037) were predictors of treatment failure. Model-derived probabilities showed that the 10-year risk of treatment failure varied from 5.8 to 41.1% according to patient’s characteristics.
Conclusions
Long-term prognosis in patients who underwent penile urethroplasty is uncertain. To date, our risk-calculator represents the first tool that might help physicians to predict the risk of treatment failure at 10 years. According to our model, such risk is largely influenced by the etiology of the stricture, the use of graft, and patient’s smoking habits.

Similar content being viewed by others
Abbreviations
- QoL:
-
Quality of life
- BMI:
-
Body mass index
- FHR:
-
Failed hypospadias repair
- LS:
-
Lichen sclerosus
- RUG:
-
Retrograde urethrogram
- VCUG:
-
Voiding cystourethrogram
- PVR:
-
Post-void residual
References
Singh SK, Agrawal SK, Mavuduru RS (2011) Management of the stricture of fossa navicularis and pendulous urethral strictures. Indian J Urol IJU J Urol Soc India 27:371–377. https://doi.org/10.4103/0970-1591.85442
Andrich DE, Greenwell TJ, Mundy AR (2003) The problems of penile urethroplasty with particular reference to 2-stage reconstructions. J Urol 170:87–89. https://doi.org/10.1097/01.ju.0000069721.20193.fd
Andrich DE, Mundy AR (2008) What is the best technique for urethroplasty? Eur Urol 54:1031–1041. https://doi.org/10.1016/j.eururo.2008.07.052
Mundy AR, Andrich DE (2011) Urethral strictures. BJU Int 107:6–26. https://doi.org/10.1111/j.1464-410X.2010.09800.x
Tonkin JB, Jordan GH (2009) Management of distal anterior urethral strictures. Nat Rev Urol 6:533–538. https://doi.org/10.1038/nrurol.2009.181
Asopa HS, Garg M, Singhal GG et al (2001) Dorsal free graft urethroplasty for urethral stricture by ventral sagittal urethrotomy approach. Urology 58:657–659. https://doi.org/10.1016/s0090-4295(01)01377-2
Barbagli G, Pellegrini G, Corradini F et al (2016) One-stage penile urethroplasty using oral mucosal graft and glue. Eur Urol 70:1069–1075. https://doi.org/10.1016/j.eururo.2016.04.025
Barbagli G, Balò S, Sansalone S, Lazzeri M (2016) One-stage and two-stage penile buccal mucosa urethroplasty. Afr J Urol 22:11–17. https://doi.org/10.1016/j.afju.2015.09.002
Joshi PM, Barbagli G, Batra V et al (2017) A novel composite two-stage urethroplasty for complex penile strictures: a multicenter experience. Indian J Urol IJU J Urol Soc India 33:155–158. https://doi.org/10.4103/0970-1591.203426
Bandini M, Marchioni M, Pompe RS et al (2017) First North American validation and head-to-head comparison of four preoperative nomograms for prediction of lymph node invasion before radical prostatectomy. BJU Int. https://doi.org/10.1111/bju.14074
Johanson B (1953) Reconstruction of the male urethra in strictures. Application of the buried intact epithelium technic. Acta Chir Scand 176(176 Suppl):1–89
Andrich DE, Mundy AR (2012) Non-transecting anastomotic bulbar urethroplasty: a preliminary report. BJU Int 109:1090–1094. https://doi.org/10.1111/j.1464-410X.2011.10508.x
Mcgowan AJ, Waterhouse K (1964) Mobilization of the anterior urethra. Bull N Y Acad Med 40:776–782
Waterhouse K, Glassberg KI (1981) Mobilization of the anterior urethra as an aid in the one-stage repair of hypospadias. Urol Clin N Am 8:521–525
Koff SA (1981) Mobilization of the urethra in the surgical treatment of hypospadias. J Urol 125:394–397. https://doi.org/10.1016/s0022-5347(17)55048-x
Atala A (2002) Urethral mobilization and advancement for midshaft to distal hypospadias. J Urol 168:1738–1741. https://doi.org/10.1097/01.ju.0000023971.96439.b8(discussion 1741)
Orandi A (1972) One-stage urethroplasty: 4-year followup. J Urol 107:977–980. https://doi.org/10.1016/s0022-5347(17)61187-x
Barbagli G, Morgia G, Lazzeri M (2008) Retrospective outcome analysis of one-stage penile urethroplasty using a flap or graft in a homogeneous series of patients. BJU Int 102:853–860. https://doi.org/10.1111/j.1464-410X.2008.07741.x
Kulkarni S, Barbagli G, Sansalone S, Lazzeri M (2009) One-sided anterior urethroplasty: a new dorsal onlay graft technique. BJU Int 104:1150–1155. https://doi.org/10.1111/j.1464-410X.2009.08590.x
Fenton AS, Morey AF, Aviles R, Garcia CR (2005) Anterior urethral strictures: etiology and characteristics. Urology 65:1055–1058. https://doi.org/10.1016/j.urology.2004.12.018
Lumen N, Hoebeke P, Willemsen P et al (2009) Etiology of urethral stricture disease in the 21st century. J Urol 182:983–987. https://doi.org/10.1016/j.juro.2009.05.023
Stein DM, Thum DJ, Barbagli G et al (2013) A geographic analysis of male urethral stricture aetiology and location. BJU Int 112:830–834. https://doi.org/10.1111/j.1464-410X.2012.11600.x
Armenakas NA, Morey AF, McAninch JW (1998) Reconstruction of resistant strictures of the fossa navicularis and meatus. J Urol 160:359–363
Pederzoli F, Joice G, Salonia A et al (2019) Regenerative and engineered options for urethroplasty. Nat Rev Urol 16:453–464. https://doi.org/10.1038/s41585-019-0198-y
Barbagli G, Akbarov I, Heidenreich A et al (2018) Anterior urethroplasty using a new tissue engineered oral mucosa graft: surgical techniques and outcomes. J Urol 200:448–456. https://doi.org/10.1016/j.juro.2018.02.3102
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. None conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.

11255_2020_2397_MOESM1_ESM.jpg
Supplementary Figure 1. Retrograde urethrogram showing narrow, irregular, and not distensible penile urethral lumen suggesting extensive scar tissue, and staged repair (JPG 61 kb)

11255_2020_2397_MOESM2_ESM.jpg
Supplementary Figure 2 A, B, C. First-stage urethroplasty. The new-meatus is located at a different site from the balanic sulcus to the base of the penis, according to the stricture length (JPG 70 kb)

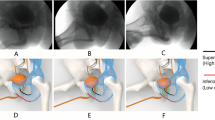
11255_2020_2397_MOESM3_ESM.jpg
Supplementary Figure 3. Two-stage oral mucosa graft. A: the urethra is ventrally opened according to Johanson's procedure. Six to nine months later the second stage is performed. B: the urethral plate is incised longitudinally to create a wide bed for the graft location. C: the oral graft is fixed to the distal urethral and the glue is injected. D: the oral graft is moved over the glue bed and pressed for 45 seconds. E: the oral graft is well fixed and distend on the urethral plate. F: the penile skin margins are incised. G: the urethra is closed. H: the penile skin is sutured (JPG 394 kb)

11255_2020_2397_MOESM4_ESM.jpg
Supplementary Figure 4. Retrograde urethrogram showing wide and non-obliterative penile urethral lumen suggesting limited scar tissue, and a one-stage repair (JPG 461 kb)

11255_2020_2397_MOESM5_ESM.jpg
Supplementary Figure 5. One-stage oral mucosa graft. A: the site of penile stricture and of the perineal incision are marked. B: the penis is pushed into the perineum and the penile stricture site is marked. C: the penile urethra is opened and the strictured area is marked. D: the urethral plate is longitudinally incised. E: the oral graft is fixed onto the bed of the dorsal urethrotomy using Glubran glue. F: the urethra is closed. G: the penis is stretched on his original position. H: the perineal opening is sutured (JPG 302 kb)

11255_2020_2397_MOESM6_ESM.jpg
Supplementary Figure 6. One-stage penile skin flap urethroplasty. A: the penile skin flap is marked. B: the skin flap is based on dartos fascia. C: the urethra is dissected from the corpora cavernosa. D: the dorsal urethral surface is exposed and fully opened. E: the penile skin flap is over the corpora cavernosa. F: the margin of skin flap is sutured the margin of the urethral mucosa, Foley 12 F. silicone grooved catheter is inserted and the urethra plate is rotated over the skin flap. G: At the end of the procedure the skin flap is completely covered by the urethra. H: the penile skin incision is closed (JPG 516 kb)
11255_2020_2397_MOESM7_ESM.xlsx
Supplementary File 1: Risk Calculator. The latter was developed from the multivariable Cox-regression model using variables’ coefficients and time-dependent risk ratios of treatment failure. Outcome was set at 10 years of follow-up after surgery (XLSX 17 kb)
Rights and permissions
About this article
Cite this article
Barbagli, G., Bandini, M., Balò, S. et al. Risk calculator for prediction of treatment-related urethroplasty failure in patients with penile urethral strictures. Int Urol Nephrol 52, 1079–1085 (2020). https://doi.org/10.1007/s11255-020-02397-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-020-02397-y