Abstract
Purpose
The number of examined lymph node (ELN) is regarded as the critical quality index for cancer care. We scrutinize the relationship among ELN number, accurate staging, and long-term survival in prostate cancer (Pca).
Methods
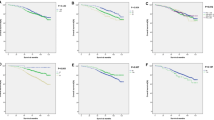
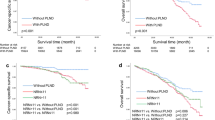
Population-based data on Pca patients in 2004–2015 from the US SEER database were investigated. The connection among ELN number and stage migration, overall survival (OS), and prostate cancer-specific survival (CSS) were evaluated by performing multivariable-adjusted logistic, Cox proportional hazards, and fine-gray competing-risk regression models, respectively. LOWESS smoother was used to fit the series of ELN number, odds ratios (OR), and hazard ratios (HR), while the Chow test was used to resolve the structural breakpoints. Subgroup and interaction analyses were performed in different risk populations.
Results
Overall, 84,838 patients were analyzed. Serial improvements were seen in stage migration (OR, 1.072, P < 0.001), OS (HR, 0.991; P < 0.001), and CSS (HR, 0.983; P < 0.001) per additional ELN after adjusting for confounders. Subgroup analysis revealed that the ELN number gains the most staging and survival benefits in high-risk population (P for interaction < 0.001). Cut-point analyses suggested that an optimal number of 12 ELNs, which was verified by the cumulative incidence curve, had a strong capability to distinguish different probabilities of CSS.
Conclusions
Higher quantities of ELNs are related to more-accurate nodal staging and long-term survival of Pca patients undergoing RP. We highlight that 12 ELNs are the optimal cut-point for the high-risk population to investigate the quality of LN detection and stratifying postoperative prognosis.





Similar content being viewed by others
Abbreviations
- ELN:
-
Examined lymph node
- LN:
-
Lymph node
- PCa:
-
Prostate cancer
- PLND:
-
Pelvic lymph-node dissection
- LND:
-
Lymph-node dissection
- LNI:
-
Lymph-node involvement
- RP:
-
Radical prostatectomy
- PSA:
-
Prostate-specific antigen
- SEER:
-
Surveillance, epidemiology, and end results database
- LOWESS:
-
the locally weighted scatterplot smoothing
- NCCN:
-
the National Comprehensive Cancer Network
- OR:
-
Odds ratio
- HR:
-
Hazard ratio
- LL:
-
Lower limit of 95% CI
- UL:
-
Upper limit of 95% CI
- Sig.:
-
Significance
- IQR:
-
Interquartile range
- OS:
-
Overall survival
- CSS:
-
Prostate cancer-specific survival
References
Siegel RL, Miller KD (2018) Jemal A (2018) Cancer statistics. CA Cancer J Clin 68(1):7–30. https://doi.org/10.3322/caac.21442
Fossati N, Willemse PM, Van den Broeck T, van den Bergh RCN, Yuan CY, Briers E, Bellmunt J, Bolla M, Cornford P, De Santis M, MacPepple E, Henry AM, Mason MD, Matveev VB, van der Poel HG, van der Kwast TH, Rouviere O, Schoots IG, Wiegel T, Lam TB, Mottet N, Joniau S (2017) The Benefits and Harms of Different Extents of Lymph Node Dissection During Radical Prostatectomy for Prostate Cancer: A Systematic Review. Eur Urol 72(1):84–109. https://doi.org/10.1016/j.eururo.2016.12.003
Briganti A, Blute ML, Eastham JH, Graefen M, Heidenreich A, Karnes JR, Montorsi F, Studer UE (2009) Pelvic lymph node dissection in prostate cancer. Eur Urol 55(6):1251–1265. https://doi.org/10.1016/j.eururo.2009.03.012
Van den Bergh L, Lerut E, Haustermans K, Deroose CM, Oyen R, Isebaert S, Budiharto T, Ameye F, Mottaghy FM, Bogaerts K, Van Poppel H, Joniau S (2015) Final analysis of a prospective trial on functional imaging for nodal staging in patients with prostate cancer at high risk for lymph node involvement. Urol Oncol 33(3):e123–e131. https://doi.org/10.1016/j.urolonc.2014.11.008
Abdollah F, Sun M, Thuret R, Budaus L, Jeldres C, Graefen M, Briganti A, Perrotte P, Rigatti P, Montorsi F, Karakiewicz PI (2010) Decreasing rate and extent of lymph node staging in patients undergoing radical prostatectomy may undermine the rate of diagnosis of lymph node metastases in prostate cancer. Eur Urol 58(6):882–892. https://doi.org/10.1016/j.eururo.2010.09.029
Abdollah F, Suardi N, Gallina A, Bianchi M, Tutolo M, Passoni N, Fossati N, Sun M, dell’Oglio P, Salonia A, Karakiewicz PI, Rigatti P, Montorsi F, Briganti A (2013) Extended pelvic lymph node dissection in prostate cancer: a 20-year audit in a single center. Ann Oncol 24(6):1459–1466. https://doi.org/10.1093/annonc/mdt120
Klein EA, Kattan M, Stephenson A, Vickers A (2008) How many lymphadenectomies does it take to cure one patient? Eur Urol 53(1):13–15. https://doi.org/10.1016/j.eururo.2007.09.017
Shah AD, Bartlett JW, Carpenter J, Nicholas O, Hemingway H (2014) Comparison of random forest and parametric imputation models for imputing missing data using MICE: a CALIBER study. Am J Epidemiol 179(6):764–774. https://doi.org/10.1093/aje/kwt312
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) Prostate Cancer. Version 2.2018
Liang W, He J, Shen Y, Shen J, He Q, Zhang J, Jiang G, Wang Q, Liu L, Gao S, Liu D, Wang Z, Zhu Z, Ng CS, Liu CC, Horsleben Petersen R, Rocco G, D’Amico T, Brunelli A, Chen H, Zhi X, Liu B, Yang Y, Chen W, Zhou Q, He J (2017) Impact of Examined Lymph Node Count on Precise Staging and Long-Term Survival of Resected Non-Small-Cell Lung Cancer: a Population Study of the US SEER Database and a Chinese Multi-Institutional Registry. J Clin Oncol 35(11):1162–1170. https://doi.org/10.1200/JCO.2016.67.5140
Sanda MG, Cadeddu JA, Kirkby E, Chen RC, Crispino T, Fontanarosa J, Freedland SJ, Greene K, Klotz LH, Makarov DV, Nelson JB, Rodrigues G, Sandler HM, Taplin ME, Treadwell JR (2018) Clinically Localized Prostate Cancer: AUA/ASTRO/SUO Guideline. Part I: Risk Stratification, Shared Decision Making, and Care Options. J Urol 199(3):683–690. https://doi.org/10.1016/j.juro.2017.11.095
Mottet N, Bellmunt J, Bolla M, Briers E, Cumberbatch MG, De Santis M, Fossati N, Gross T, Henry AM, Joniau S, Lam TB, Mason MD, Matveev VB, Moldovan PC, van den Bergh RCN, Van den Broeck T, van der Poel HG, van der Kwast TH, Rouviere O, Schoots IG, Wiegel T, Cornford P (2017) EAU-ESTRO-SIOG Guidelines on Prostate Cancer. Part 1: Screening, Diagnosis, and Local Treatment with Curative Intent. Eur Urol 71(4):618–629. https://doi.org/10.1016/j.eururo.2016.08.003
Briganti A, Larcher A, Abdollah F, Capitanio U, Gallina A, Suardi N, Bianchi M, Sun M, Freschi M, Salonia A, Karakiewicz PI, Rigatti P, Montorsi F (2012) Updated nomogram predicting lymph node invasion in patients with prostate cancer undergoing extended pelvic lymph node dissection: the essential importance of percentage of positive cores. Eur Urol 61(3):480–487. https://doi.org/10.1016/j.eururo.2011.10.044
Eifler JB, Feng Z, Lin BM, Partin MT, Humphreys EB, Han M, Epstein JI, Walsh PC, Trock BJ, Partin AW (2013) An updated prostate cancer staging nomogram (Partin tables) based on cases from 2006 to 2011. BJU Int 111(1):22–29. https://doi.org/10.1111/j.1464-410X.2012.11324.x
Roach M 3rd (1993) Re: the use of prostate specific antigen, clinical stage and Gleason score to predict pathological stage in men with localized prostate cancer. J Urol 150(6):1923–1924. https://doi.org/10.1016/s0022-5347(17)35937-2
Pisansky TM, Blute ML, Suman VJ, Bostwick DG, Earle JD, Zincke H (1996) Correlation of pretherapy prostate cancer characteristics with seminal vesicle invasion in radical prostatectomy specimens. Int J Radiat Oncol Biol Phys 36(3):585–591. https://doi.org/10.1016/s0360-3016(96)00359-8
Abdollah F, Gandaglia G, Suardi N, Capitanio U, Salonia A, Nini A, Moschini M, Sun M, Karakiewicz PI, Shariat SF, Montorsi F, Briganti A (2015) More extensive pelvic lymph node dissection improves survival in patients with node-positive prostate cancer. Eur Urol 67(2):212–219. https://doi.org/10.1016/j.eururo.2014.05.011
Abdollah F, Sun M, Thuret R, Jeldres C, Tian Z, Briganti A, Shariat SF, Perrotte P, Montorsi F, Karakiewicz PI (2012) Lymph node count threshold for optimal pelvic lymph node staging in prostate cancer. Int J Urol 19(7):645–651. https://doi.org/10.1111/j.1442-2042.2012.02993.x
Osmonov DK, Boller A, Aksenov A, Naumann M, Junemann KP (2013) Intermediate and high risk prostate cancer patients. Clinical significance of extended lymphadenectomy. Urologe A 52(2):240–245. https://doi.org/10.1007/s00120-012-3005-4
Preisser F, Bandini M, Marchioni M, Nazzani S, Tian Z, Pompe RS, Fossati N, Briganti A, Saad F, Shariat SF, Heinzer H, Huland H, Graefen M, Tilki D, Karakiewicz PI (2018) Extent of lymph node dissection improves survival in prostate cancer patients treated with radical prostatectomy without lymph node invasion. Prostate 78(6):469–475. https://doi.org/10.1002/pros.23491
Moravek P (1987) Therapeutic role of pelvic lymphadenectomy in carcinoma of the prostate: own experiences. Int Urol Nephrol 19(3):315–319. https://doi.org/10.1007/bf02549869
Thomas C, Ziewers S, Thomas A, Dotzauer R, Bartsch G, Haferkamp A, Tsaur I (2019) Development of symptomatic lymphoceles after radical prostatectomy and pelvic lymph node dissection is independent of surgical approach: a single-center analysis. Int Urol Nephrol 51(4):633–640. https://doi.org/10.1007/s11255-019-02103-7
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Drafting the manuscript, Cheng Chen, Jie Shen, and Zhaoyu Xing; Revising, Changchuan Jiang and Li Cui; Conception and design, Xiaozhou He and Renfang Xu; Acquisition of data, Cheng Chen; Analysis and interpretation of data, Dong Xue and Linkun Hu.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, C., Shen, J., Xing, Z. et al. Significance of examined lymph-node count in accurate staging and long-term survival in patients undergoing radical prostatectomy: a population-based study. Int Urol Nephrol 52, 271–278 (2020). https://doi.org/10.1007/s11255-019-02300-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-019-02300-4