Abstract
Purpose
In addition to standard TNM N staging, lymph node ratio (LNR) and log odds of metastatic lymph node (LODDS) staging methods have been developed for cancer staging. We compared the prognostic performance of the total number of lymph nodes examined (TNLE), number of metastatic lymph node (NMLN), LNR, and LODDS in prostate cancer.
Methods
Data from 1400 patients diagnosed with prostate cancer between 2004 and 2009 who underwent lymphadenectomy were extracted from the Surveillance Epidemiology and End Results database. Kaplan–Meier methods and multivariable Cox regression analysis were used to evaluate the prognostic value of different lymph node staging schemes in patients with lymph node metastasis.
Results
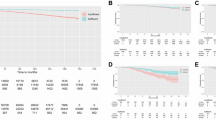
Univariate analysis showed that age, T stage, radiotherapy history, Gleason score, LNR classification, LODDS classification, and NMLN except TNLE classification were significant prognostic factors for overall survival. In multivariate analysis, LNR classification, LODDS classification, and NMLN but TNLE classification remained significant prognostic factors for overall survival. LNR classification had the highest C-index (0.672; 95% confidence interval [CI]: 0.609–0.734) and the lowest Akaike information criterion (AIC) (4057.018), indicating the best prognostic performance. Scatter plots showed that LODDS increased with increasing LNR, exhibiting a strong overall correlation between these two lymph node staging methods (r2 = 0.9072). LNR and LODDS generally increased with increasing NMLN, although the correlation was relatively low.
Conclusion
Our results indicate that LNR and LODDS may be better predictors of overall survival than the AJCC/UICC N category in patients undergoing curative surgery for prostate cancer.



Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A (2018) Cancer statistics. CA Cancer J Clin 68(1):7–30. https://doi.org/10.3322/caac.21442
Miller KD, Siegel RL, Lin CC, Mariotto AB, Kramer JL, Rowland JH, Stein KD, Alteri R, Jemal A (2016) Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin 66(4):271–289. https://doi.org/10.3322/caac.21349
Daneshmand S, Quek ML, Stein JP, Lieskovsky G, Cai J, Pinski J, Skinner EC, Skinner DG (2004) Prognosis of patients with lymph node positive prostate cancer following radical prostatectomy: long-term results. J Urol 172(6 Pt 1):2252–2255. https://doi.org/10.1097/01.ju.0000143448.04161.cc
Amin MB, Edge Stephen B (eds) (2017) AJCC cancer staging manual. Springer, Berlin
Sakata J, Shirai Y, Wakai T, Ajioka Y, Hatakeyama K (2010) Number of positive lymph nodes independently determines the prognosis after resection in patients with gallbladder carcinoma. Ann Surg Oncol 17(7):1831–1840. https://doi.org/10.1245/s10434-009-0899-1
Marchet A, Mocellin S, Ambrosi A, Morgagni P, Garcea D, Marrelli D, Roviello F, de Manzoni G, Minicozzi A, Natalini G, De Santis F, Baiocchi L, Coniglio A, Nitti D (2007) The ratio between metastatic and examined lymph nodes (N ratio) is an independent prognostic factor in gastric cancer regardless of the type of lymphadenectomy: results from an Italian multicentric study in 1853 patients. Ann Surg 245(4):543–552. https://doi.org/10.1097/01.sla.0000250423.43436.e1
Marchet A, Mocellin S, Ambrosi A, de Manzoni G, Di Leo A, Marrelli D, Roviello F, Morgagni P, Saragoni L, Natalini G, De Santis F, Baiocchi L, Coniglio A, Nitti D (2008) The prognostic value of N-ratio in patients with gastric cancer: validation in a large, multicenter series. Eur J Surg Oncol 34(2):159–165. https://doi.org/10.1016/j.ejso.2007.04.018
Arslan NC, Sokmen S, Canda AE, Terzi C, Sarioglu S (2014) The prognostic impact of the log odds of positive lymph nodes in colon cancer. Colorectal Dis 16(11):O386–O392. https://doi.org/10.1111/codi.12702
Huang B, Chen C, Ni M, Mo S, Cai G, Cai S (2016) Log odds of positive lymph nodes is a superior prognostic indicator in stage III rectal cancer patients: a retrospective analysis of 17,632 patients in the SEER database. Int J Surg (London, England) 32:24–30. https://doi.org/10.1016/j.ijsu.2016.06.002
Calero A, Escrig-Sos J, Mingol F, Arroyo A, Martinez-Ramos D, de Juan M, Salvador-Sanchis JL, Garcia-Granero E, Calpena R, Lacueva FJ (2015) Usefulness of the log odds of positive lymph nodes to predict and discriminate prognosis in gastric carcinomas. J Gastrointest Surg 19(5):813–820. https://doi.org/10.1007/s11605-014-2728-5
Aurello P, Petrucciani N, Nigri GR, La Torre M, Magistri P, Tierno S, D’Angelo F, Ramacciato G (2014) Log odds of positive lymph nodes (LODDS): what are their role in the prognostic assessment of gastric adenocarcinoma? J Gastrointest Surg 18(7):1254–1260. https://doi.org/10.1007/s11605-014-2539-8
Wu SG, Sun JY, Yang LC, Zhou J, Li FY, Li Q, Lin HX, Lin Q, He ZY (2015) Prognosis of patients with esophageal squamous cell carcinoma after esophagectomy using the log odds of positive lymph nodes. Oncotarget 6(34):36911–36922. https://doi.org/10.18632/oncotarget.5366
Wen J, Ye F, He X, Li S, Huang X, Xiao X, Xie X (2016) Development and validation of a prognostic nomogram based on the log odds of positive lymph nodes (LODDS) for breast cancer. Oncotarget 7(15):21046–21053. https://doi.org/10.18632/oncotarget.8091
Song YX, Gao P, Wang ZN, Tong LL, Xu YY, Sun Z, Xing CZ, Xu HM (2011) Which is the most suitable classification for colorectal cancer, log odds, the number or the ratio of positive lymph nodes? PLoS One 6(12):e28937. https://doi.org/10.1371/journal.pone.0028937
Rosenberg R, Engel J, Bruns C, Heitland W, Hermes N, Jauch KW, Kopp R, Putterich E, Ruppert R, Schuster T, Friess H, Holzel D (2010) The prognostic value of lymph node ratio in a population-based collective of colorectal cancer patients. Ann Surg 251(6):1070–1078. https://doi.org/10.1097/SLA.0b013e3181d7789d
Berger AC, Sigurdson ER, LeVoyer T, Hanlon A, Mayer RJ, Macdonald JS, Catalano PJ, Haller DG (2005) Colon cancer survival is associated with decreasing ratio of metastatic to examined lymph nodes. J Clin Oncol 23(34):8706–8712. https://doi.org/10.1200/jco.2005.02.8852
Kornprat P, Pollheimer MJ, Lindtner RA, Schlemmer A, Rehak P, Langner C (2011) Value of tumor size as a prognostic variable in colorectal cancer: a critical reappraisal. Am J Clin Oncol 34(1):43–49. https://doi.org/10.1097/COC.0b013e3181cae8dd
Wang J, Hassett JM, Dayton MT, Kulaylat MN (2008) The prognostic superiority of log odds of positive lymph nodes in stage III colon cancer. J Gastrointest Surg 12(10):1790–1796. https://doi.org/10.1007/s11605-008-0651-3
Spolverato G, Ejaz A, Kim Y, Squires MH, Poultsides G, Fields RC, Bloomston M, Weber SM, Votanopoulos K, Acher AW, Jin LX, Hawkins WG, Schmidt C, Kooby DA, Worhunsky D, Saunders N, Cho CS, Levine EA, Maithel SK, Pawlik TM (2015) Prognostic performance of different lymph node staging systems after curative intent resection for gastric adenocarcinoma. Ann Surg 262(6):991–998. https://doi.org/10.1097/sla.0000000000001040
Acknowledgements
The authors would like to thank all patients involved in this study and all the staff working for SEER database. This work was funded by the National Natural Science Foundation of China (81572531). The funding source provided financial support for the study and did not have any other involvement in this study. In addition, we thank Clare Cox, PhD, from Liwen Bianji, Edanz Editing China (www.liwenbianji.cn/ac), for editing the English text of a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
None of the authors declare competing financial interests.
Ethical approval
All the procedures performed in studies involving human participants were in accordance with the ethical standards of the Research Ethics Committee of Shanghai Cancer Center, Fudan University, China and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by the Research Ethics Committee of Shanghai Cancer Center, Fudan University, China according to the provisions of the Declaration of Helsinki (as revised in Fortaleza, Brazil, October 2013). All patients were identified from the public SEER database. Thus, informed consent was not required.
Informed consent
The public SEER databases have obtained informed consent from all individual participants included in the SEER database before. Therefore, we did not need extra informed consent of the patients. In addition, patients in this study were all anonymous and other personal information was also erased.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jin, S., Wang, J., Shen, Y. et al. Comparison of different lymph node staging schemes in prostate cancer patients with lymph node metastasis. Int Urol Nephrol 52, 87–95 (2020). https://doi.org/10.1007/s11255-019-02294-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-019-02294-z