Abstract
Objectives
The aim of this study is to evaluate the association between total testosterone density (TTD), defined as the ratio of serum TT to prostate volume (PV), and high tumor load (HTL) in low-risk prostate cancer (PCA) patients who underwent radical prostatectomy.
Materials and methods
Tumor load was defined as the percentage of prostate volume invaded by cancer (PPI-PCA) in the surgical specimen. Pathologic features including tumor upgrading, upstaging or positive surgical margins in the specimen defined unfavorable disease (UD). PSA, TT, PSA density (PSAD), TTD, percentage of biopsy positive cores (BPC), PV and body mass index (BMI). The association of factors with the risk UD and HTL was evaluated by statistical methods.
Results
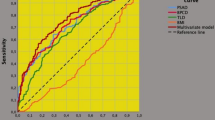
The cohort included 144 consecutive low-risk PCA patients. Overall, 104 patients (72.2%) had at least one feature indicating UD. TTD was associated with BMI, TT, PSA, PV and PPI-PCA ≥ 20% defined as HTL. A higher PPI-PCA was associated with an increased risk of UD with a fair discriminant power (area under the curve, AUC = 0.775; p < 0.0001). Patients with PPI-PCA > 20% were considered the study group versus patients with a PPI-PCA < 20% (control group). BPC, PSAD and TTD were independently associated with the risk of HTL (PPI-PCA ≥ 20%) with receiver-operating characteristics (ROC) curves indicating the same discriminant power for BPC (AUC = 0.628; p = 0.013), PSAD (AUC = 0.611; p = 0.032) and TTD (AUC = 0.610; p = 0.032).
Conclusions
Among low-risk PCA patients, TTD is associated with the risk of HTL, which is an independent predictor of UD and should be evaluated in the management of these patients.





Similar content being viewed by others
Abbreviations
- AS:
-
Active surveillances
- AUC:
-
Area under the curve
- BMI:
-
Body mass index
- BPC:
-
Biopsy positive cores
- EAU:
-
European association of urology
- ePLND:
-
Extended pelvic lymph node dissection HTL—high tumor load
- ISUP:
-
International society of urologic pathology
- LNI:
-
Lymph node invasion
- PW:
-
Prostate weight
- PCA:
-
Prostate cancer
- PPI-PCA:
-
Percentage of prostate volume invaded by prostate cancer
- PSA:
-
Prostate-specific antigen
- PSAD:
-
PSA density
- PV:
-
Prostate volume
- RARP:
-
Robot-assisted radical prostatectomy
- ROC:
-
Receiver-operating characteristics
- RP:
-
Radical prostatectomy
- RRP:
-
Retropubic radical prostatectomy
- TT:
-
Total testosterone
- TTD:
-
Total testosterone density
- UD:
-
Unfavorable disease
- WW:
-
Watchful waiting
References
D’Amico AV, Whittington R, Malkowicz SB, Schultz D, Blank K, Broderick GA, Tomaszewski JE, Renshaw AA, Kaplan I, Beard CJ, Wein A (1998) Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA 280:969–974
Mottet N, Bellmunt J, Bolla M, Briers E, Cumberbatch MG, De Santis M, Fossati N, Gross T, Henry AM, Joniau S, Lam TB, Mason MD, Matveev VB, Moldovan PC, van den Bergh RCN, Van den Broeck T, van der Poel HG, van der Kwast TH, Rouviere O, Schoots IG, Wiegel T, Cornford P (2017) EAU-ESTRO-SIOG guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol 71:618–629
Pierorazio PM, Walsh PC, Partin AW, Epstein JI (2013) Prognostic Gleason grade grouping: data based on the modified Gleason scoring system. BJU Int 111:753–760
Epstein JI, Egevad L, Amin MB, Delahunt B, Srigley JR, Humphrey PA (2016) The International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma: definition of grading patterns and proposal for a new grading system. Am J Surg Pathol 40:244–252
Epstein JI, Zelefsky MJ, Sjoberg DD, Nelson JB, Egevad L, Magi-Galluzzi C, Vickers AJ, Parwani AV, Reuter VE, Fine SW, Eastham JA, Wiklund P, Han M, Reddy CA, Ciezki JP, Nyberg T, Klein EA (2016) A contemporary prostate cancer grading system: a validated alternative to the Gleason Score. Eur Urol 69:428–435
Porcaro AB, Inverardi D, Corsi P, Sebben M, Cacciamani G, Tafuri A, Processali T, Pirozzi M, Mattevi D, De Marchi D, Amigoni N, Rizzetto R, Cerruto MA, Brunelli M, Siracusano S, Artibani W (2018) Prostate specific antigen levels and proportion of biopsy positive cores are independent predictors of upgrading patterns in low risk prostate cancer. Minerva Urol Nefrol. https://doi.org/10.23736/S0393-2249.18.03172-7
Porcaro AB, de Luyk N, Corsi P, Sebben M, Tafuri A, Mattevi D, Processali T, Cerruto MA, Brunelli M, Antoniolli SZ (2017) Clinical factors predicting and stratifying the risk of lymph node invasion in localized prostate cancer. Urol Int 99:207–214
Porcaro AB, Siracusano S, Luyk ND, Corsi P, Sebben M, Tafuri A, Processali T, Cerasuolo M, Mattevi D, Inverardi D (2018) Clinical factors stratifying the risk of tumor upgrading to high-grade disease in low-risk prostate cancer. Tumori J 104:111–115
Porcaro AB, Cavicchioli F, Mattevi D, De Luyk N, Corsi P, Sebben M, Tafuri A, Processali T, Cerasuolo M, Tamanini I (2017) Clinical factors of disease reclassification or progression in a contemporary cohort of prostate cancer patients elected to active surveillance. Urol Int 98:32–39
Porcaro AB, De Luyk N, Corsi P, Sebben M, Tafuri A, Processali T, Cerasuolo M, Mattevi D, Cerruto MA, Brunelli M, Siracusano S, Artibani W (2017) Association between basal total testosterone levels and tumor upgrading in low and intermediate risk prostate cancer. Urol Int 99:215–221
Porcaro AB, Cavicchioli F, Mattevi D, De Luyk N, Corsi P, Sebben M, Tafuri A, Processali T, Cerasuolo M, Tamanini I, Cacciamani G, Cerruto MA, Brunelli M, Novella G, Siracusano S, Artibani W (2017) Clinical factors of disease reclassification or progression in a contemporary cohort of prostate cancer patients elected to active surveillance. Urol Int 98:32–39
Freedland SJ, Isaacs WB, Platz EA, Terris MK, Aronson WJ, Amling CL, Presti JC Jr, Kane CJ (2005) Prostate size and risk of high-grade, advanced prostate cancer and biochemical progression after radical prostatectomy: a search database study. J Clin Oncol 23:7546–7554
D’Amico AV, Whittington R, Malkowicz SB, Schultz D, Tomaszewski JE, Wein A (1998) A prostate gland volume of more than 75 cm3 predicts for a favorable outcome after radical prostatectomy for localized prostate cancer. Urology 52:631–636
Porcaro AB, Petroziello A, Brunelli M, De Luyk N, Cacciamani G, Corsi P, Sebben M, Tafuri A, Tamanini I, Caruso B (2016) High testosterone preoperative plasma levels independently predict biopsy Gleason score upgrading in men with prostate cancer undergoing radical prostatectomy. Urol Int 96:470–478
Porcaro AB, Tafuri A, Sebben M, Corsi P, Pocessali T, Pirozzi M, Amigoni N, Rizzetto R, Mariotto A, Inverardi D (2018) Positive association between preoperative total testosterone levels and risk of positive surgical margins by prostate cancer: results in 476 consecutive patients treated only by radical prostatectomy. Urol Int 101:38–46
Porcaro AB, Tafuri A, Sebben M, Pirozzi M, Processali T, Rizzetto R, Amigoni N, Shakir A, Tiso L, Cerrato C (2019) Positive association between basal total testosterone circulating levels and tumor grade groups at the time of diagnosis of prostate cancer. Urol Int, pp 1–8
Massengill JC, Sun L, Moul JW, Wu H, McLEOD DG, Amling C, Lance R, Foley J, Sexton W, Kusuda L (2003) Pretreatment total testosterone level predicts pathological stage in patients with localized prostate cancer treated with radical prostatectomy. J Urol 169:1670–1675
Dai B, Qu Y, Kong Y, Ye D, Yao X, Zhang S, Wang C, Zhang H, Yang W (2012) Low pretreatment serum total testosterone is associated with a high incidence of Gleason score 8–10 disease in prostatectomy specimens: data from ethnic Chinese patients with localized prostate cancer. BJU Int 110:E667–E672
Ferro M, Lucarelli G, Bruzzese D, Di Lorenzo G, Perdonà S, Autorino R, Cantiello F, La Rocca R, Busetto GM, Cimmino A (2017) Low serum total testosterone level as a predictor of upstaging and upgrading in low-risk prostate cancer patients meeting the inclusion criteria for active surveillance. Oncotarget 8:18424
Edge SB, Compton CC (2010) The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 17:1471–1474
Menon M, Tewari A, Peabody J (2003) Vattikuti Institute prostatectomy: technique. J Urol 169:2289–2292
Walsh PC (1998) Anatomic radical prostatectomy: evolution of the surgical technique. J Urol 160:2418–2424
Briganti A, Larcher A, Abdollah F, Capitanio U, Gallina A, Suardi N, Bianchi M, Sun M, Freschi M, Salonia A, Karakiewicz PI, Rigatti P, Montorsi F (2012) Updated nomogram predicting lymph node invasion in patients with prostate cancer undergoing extended pelvic lymph node dissection: the essential importance of percentage of positive cores. Eur Urol 61:480–487
Porcaro AB, de Luyk N, Corsi P, Sebben M, Tafuri A, Tamanini I, Processali T, Cerruto MA, Migliorini F, Brunelli M (2017) Bilateral lymph node micrometastases and seminal vesicle invasion associated with same clinical predictors in localized prostate cancer. Tumori J 103:299–306
Porcaro AB, Siracusano S, De Luyk N, Corsi P, Sebben M, Tafuri A, Bizzotto L, Tamanini I, Inverardi D, Cerruto MA (2016) Low-risk prostate cancer and tumor upgrading to higher patterns in the surgical specimen. Analysis of clinical factors predicting tumor upgrading to higher Gleason patterns in a contemporary series of patients who have been evaluated according to the modified Gleason score grading system. Urol Int 97:32–41
Srigley JR, Humphrey PA, Amin MB, Chang SS, Egevad L, Epstein JI, Grignon DJ, McKiernan JM, Montironi R, Renshaw AA, Reuter VE, Wheeler TM (2009) Protocol for the examination of specimens from patients with carcinoma of the prostate gland. Arch Pathol Lab Med 133:1568–1576
Epstein JI, Feng Z, Trock BJ, Pierorazio PM (2012) Upgrading and downgrading of prostate cancer from biopsy to radical prostatectomy: incidence and predictive factors using the modified Gleason grading system and factoring in tertiary grades. Eur Urol 61:1019–1024
Artibani W, Porcaro AB, De Marco V, Cerruto MA, Siracusano S (2017) Management of biochemical recurrence after primary curative treatment for prostate cancer: a review. Urol Int 100:251–262
Freedland SJ, Kane CJ, Presti JC, Terris MK, Amling CL, Dorey F, Aronson WJ (2003) Comparison of preoperative prostate specific antigen density and prostate specific antigen for predicting recurrence after radical prostatectomy: results from the search data base. J Urol 169:969–973
Klap J, Schmid M, Loughlin KR (2015) The relationship between total testosterone levels and prostate cancer: a review of the continuing controversy. J Urol 193:403–413
Lopez DS, Advani S, Tsilidis KK, Wang R, Canfield S (2017) Endogenous and exogenous testosterone and prostate cancer: decreased-, increased- or null-risk? Transl Androl Urol 6:566–579
Loughlin KR (2016) The testosterone conundrum: the putative relationship between testosterone levels and prostate cancer. Urol Oncol 34:482.e1–482.e4
Benson MC, Seong Whang I, Pantuck A, Ring K, Kaplan SA, Olsson CA, Cooner WH (1992) Prostate specific antigen density: a means of distinguishing benign prostatic hypertrophy and prostate cancer. J Urol 147:815–816
Terris MK, Prestigiacomo AF, Stamey TA (1998) Comparison of prostate size in university and veterans affairs health care system patients with negative prostate biopsies. Urology 51:412–414
Nixon RG, Meyer GE, Brawer MK (1999) Differences in prostate size between patients from University and Veterans Affairs Medical Center populations. Prostate 38:144–150
Wu FC, Tajar A, Pye SR, Silman AJ, Finn JD, O’Neill TW, Bartfai G, Casanueva F, Forti G, Giwercman A, Huhtaniemi IT, Kula K, Punab M, Boonen S, Vanderschueren D (2008) Hypothalamic-pituitary-testicular axis disruptions in older men are differentially linked to age and modifiable risk factors: the European Male Aging Study. J Clin Endocrinol Metab 93:2737–2745
Porcaro AB, Tafuri A, Sebben M, Processali T, Pirozzi M, Amigoni N, Rizzetto R, Shakir A, Cacciamani GE, Brunelli M, Siracusano S, Cerruto MA, Artibani W (2019) Body mass index and prostatic specific antigen are independent predictors of multiple prostate cancer lymph node metastases in Caucasian patients undergoing robot assisted radical prostatectomy and extended pelvic lymph node dissection. Minerva Urol Nefrol. https://doi.org/10.23736/S0393-2249.19.03401-5
Porcaro AB, Tafuri A, Sebben M, Processali T, Pirozzi M, Amigoni N, Rizzetto R, Shakir A, Cerruto MA, Brunelli M, Siracusano S, Artibani W (2019) High body mass index predicts multiple prostate cancer lymph node metastases after radical prostatectomy and extended pelvic lymph node dissection. Asian J Androl. https://doi.org/10.4103/aja.aja_70_19
Porcaro AB, Sebben M, Tafuri A, de Luyk N, Corsi P, Processali T, Pirozzi M, Rizzetto R, Amigoni N, Mattevi D, Cerruto MA, Brunelli M, Novella G, De Marco V, Migliorini F, Artibani W (2019) Body mass index is an independent predictor of Clavien-Dindo grade 3 complications in patients undergoing robot assisted radical prostatectomy with extensive pelvic lymph node dissection. J Robot Surg 13:83–89
Hua Q, Zhu Y, Liu H, Ye X (2016) Diabetes and the risk of biochemical recurrence in patients with treated localized prostate cancer: a meta-analysis. Int Urol Nephrol 48:1437–1443
Oh JJ, Hong SK, Lee S, Sohn SJ, Lee SE (2013) Diabetes mellitus is associated with short prostate-specific antigen doubling time after radical prostatectomy. Int Urol Nephrol 45:121–127
Koo KC, Yoon YE, Rha KH, Chung BH, Yang SC, Hong SJ (2014) Low body mass index is associated with adverse oncological outcomes following radical prostatectomy in Korean prostate cancer patients. Int Urol Nephrol 46:1935–1940
Labrie F, Bélanger A, Bélanger P, Bérubé R, Martel C, Cusan L, Gomez J, Candas B, Castiel I, Chaussade V (2006) Androgen glucuronides, instead of testosterone, as the new markers of androgenic activity in women. J Steroid Biochem Mol Biol 99:182–188
Smals A, Kloppenborg P, Benraad TJ (1976) Circannual cycle in plasma testosterone levels in man. J Clin Endocrinol Metab 42:979–982
Funding
The authors did not receive financial support.
Author information
Authors and Affiliations
Contributions
ABP: project development, data analysis and interpretation, manuscript writing. AT: project development, data collection, data analysis and interpretation, manuscript writing. MS, MP, TP, NA, and RR: data collection. AS: data collection and language and critical revision. MB, FM, SS, and WA: other (supervision and critical revision).
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Porcaro, A.B., Tafuri, A., Sebben, M. et al. Total testosterone density predicts high tumor load and disease reclassification of prostate cancer: results in 144 low-risk patients who underwent radical prostatectomy. Int Urol Nephrol 51, 2169–2180 (2019). https://doi.org/10.1007/s11255-019-02263-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-019-02263-6