Abstract
Background
Peritoneal dialysis (PD) related infections are associated with technique failure and mortality. The aim of this multicentre study was to examine epidemiology, treatment and outcomes of PD-related infections in Poland as well as practice patterns for prevention of these complications in the context of current ISPD recommendations.
Methods
A survey on PD practices in relation to infectious complications was conducted in 11 large Polish PD centres. Epidemiology of peritonitis and exit-site infections (ESI) was examined in all patients treated in these units over a 2 year period.
Results
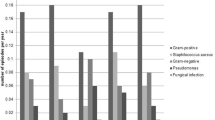
The study included data on 559 PD patients with 62.4% on CAPD. Practice patterns for prevention of infectious complications are presented. The rate of peritonitis was 0.29 episodes per year at risk, with Gram positive microorganisms responsible for more than 50% of infections and 85.8% effectively treated. Diagnosis and treatment followed ISPD guidelines however most units did not provide an anti-fungal prophylaxis. Although neither of the centres reported routine topical mupirocin on catheter exit-site, the rate of ESI was low (0.1 episodes per year at risk), with Staphylococcus aureus as most common pathogen and full recovery in 78.3% of cases.
Conclusion
The study shows rewarding outcomes in prevention and treatment of PD-associated infections, mainly due to a thorough compliance with the current ISPD guidelines, although some deviations from the recommendations in terms of practice patterns have been observed. More studies are needed in large numbers of patients to differentiate the importance of specific recommendations and further support the guidelines.
Similar content being viewed by others
References
Li PK, Szeto CC, Piraino B et al (2016) ISPD peritonitis recommendations: 2016 update on prevention and treatment. Perit Dial Int 36(5):481–508
Szeto CC, Li PK, Johnson DW et al (2017) ISPD catheter-related infection recommendations: 2017 update. Perit Dial Int 37(2):141–154
Chow KM, Szeto CC, Leung CB et al (2005) A risk analysis of continuous ambulatory peritoneal dialysis-related peritonitis. Perit Dial Int 25(4):374–379
De Vecchi AF, Maccario M, Braga M et al (1998) Peritoneal dialysis in nondiabetic patients older than 70 years: comparison with patients aged 40 to 60 years. Am J Kidney Dis 31(3):479–490
Lobo JV, Villar KR, de Andrade Junior MP, Bastos Kde A (2010) Predictor factors of peritoneal dialysis-related peritonitis. J Bras Nefrol 32(2):156–164
Kotsanas D, Polkinghorne KR, Korman TM, Atkins RC, Brown F (2007) Risk factors for peritoneal dialysis-related peritonitis: can we reduce the incidence and improve patient selection?. Nephrology 12(3):239–245
Oo TN, Roberts TL, Collins AJ (2005) A comparison of peritonitis rates from the United States Renal Data System database: CAPD versus continuous cycling peritoneal dialysis patients. Am J Kidney Dis 45(2):372–380
Lim WH, Boudville N, McDonald SP et al (2011) Remote indigenous peritoneal dialysis patients have higher risk of peritonitis, technique failure, all-cause and peritonitis-related mortality. Nephrol Dial Transplant 26(10):3366–3372
Geerlings SE, Hoepelman AI (1999) Immune dysfunction in patients with diabetes mellitus (DM). FEMS Immunol Med Microbiol 26(3–4):259–265
Han SH, Lee SC, Ahn SV et al (2007) Reduced residual renal function is a risk of peritonitis in continuous ambulatory peritoneal dialysis patients. Nephrol Dial Transplant 22(9):2653–2658
Zent R, Myers JE, Donald D, Rayner BL (1994) Continuous ambulatory peritoneal dialysis: an option in the developing world? Perit Dial Int 14(1):48–51
Toda S, Ito Y, Mizuno M et al (2012) Asymptomatic diverticulosis identified by computed tomography is not a risk factor for enteric peritonitis. Nephrol Dial Transplant 27(6):2511–2516
Tranaeus A, Heimburger O, Granqvist S (1990) Diverticular disease of the colon: a risk factor for peritonitis in continuous peritoneal dialysis. Nephrol Dial Transplant 5(2):141–147
Zhang L, Hawley CM, Johnson DW (2016) Focus on peritoneal dialysis training: working to decrease peritonitis rates. Nephrol Dial Transplant 31(2):214–222
Piraino B, Bernardini J, Brown E et al (2011) ISPD position statement on reducing the risks of peritoneal dialysis-related infections. Perit Dial Int 31(6):614–630
Bernardini J, Price V, Figueiredo A (2006) International society for peritoneal dialysis nursing liaison C: peritoneal dialysis patient training, 2006. Perit Dial Int 26(6):625–632
Dong J, Chen Y (2010) Impact of the bag exchange procedure on risk of peritonitis. Perit Dial Int 30(4):440–447
Bernardini J, Nagy M, Piraino B (2000) Pattern of noncompliance with dialysis exchanges in peritoneal dialysis patients. Am J Kidney Dis 35(6):1104–1110
Strippoli GF, Tong A, Johnson D, Schena FP, Craig JC (2004) Antimicrobial agents to prevent peritonitis in peritoneal dialysis: a systematic review of randomized controlled trials. Am J Kidney Dis 44(4):591–603
Kofteridis DP, Valachis A, Perakis K et al (2010) Peritoneal dialysis-associated peritonitis: clinical features and predictors of outcome. Int J Infect Dis 14(6):e489–e493
Ghali JR, Bannister KM, Brown FG et al (2011) Microbiology and outcomes of peritonitis in Australian peritoneal dialysis patients. Perit Dial Int 31(6):651–662
Zelenitsky SA, Howarth J, Lagace-Wiens P et al (2017) Microbiological trends and antimicrobial resistance in peritoneal dialysis-related peritonitis, 2005–2014. Perit Dial Int 37(2):170–176
Campbell DJ, Mudge DW, Gallagher MP et al (2017) Infection prophylaxis in peritoneal dialysis patients: results from an Australia/New Zealand survey. Perit Dial Int 37(2):191–197
Williams PF, Moncrieff N, Marriott J (2000) No benefit in using nystatin prophylaxis against fungal peritonitis in peritoneal dialysis patients. Perit Dial Int 20(3):352–353
Perl J, Zhao J, Bieber B et al (2016) Variation in the treatment and prevention of peritoneal dialysis related infections: preliminary results from the Peritoneal Dialysis Outcomes and Practice Patterns Study (PDOPPS). Nephrol Dial Transplant 31(Supplement 1):i235–i245
Htay H, Johnson DW, Wu SY et al (2017) Comparison of topical chlorhexidine and mupirocin for the prevention of Exit-site infection in incident peritoneal dialysis patients. Perit Dial Int 37(3):266–272
Thodis E, Bhaskaran S, Pasadakis P et al (1998) Decrease in Staphylococcus aureus exit-site infections and peritonitis in CAPD patients by local application of mupirocin ointment at the catheter exit site. Perit Dial Int 18(3):261–270
Lim CT, Wong KS, Foo MW (2005) The impact of topical mupirocin on peritoneal dialysis infection in Singapore General Hospital. Nephrol Dial Transplant 20(10):2202–2206
Kopriva-Altfahrt G, Konig P, Mundle M et al (2009) Exit-site care in Austrian peritoneal dialysis centers—a nationwide survey. Perit Dial Int 29(3):330–339
Bechade C, Guillouet S, Verger C et al (2017) Centre characteristics associated with the risk of peritonitis in peritoneal dialysis: a hierarchical modelling approach based on the data of the French Language Peritoneal Dialysis Registry. Nephrol Dial Transplant 32(6):1018–1023
Nadeau-Fredette AC, Johnson DW, Hawley CM et al (2016) Center-specific factors associated with peritonitis risk-a multi-center registry analysis. Perit Dial Int 36(5):509–518
Htay H, Cho Y, Pascoe EM et al (2018) Center effects and peritoneal dialysis peritonitis outcomes: analysis of a national registry. Am J Kidney Dis 71(6):814–821
Perl J, Davies SJ, Lambie M et al (2016) The Peritoneal Dialysis Outcomes and Practice Patterns Study (PDOPPS): unifying efforts to inform practice and improve global outcomes in peritoneal dialysis. Perit Dial Int 36(3):297–307
Funding
There was no funding to the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MLN,JMR,EG,BS,MG,PJ - Speaker’s honoraria from Fresenius Medical Care, MLN,MC,BN,EG,BS,EW,ES,MG,RK- Speaker’s honoraria from Baxter, BN,BS - Speaker’s honoraria from MSD, BN - Speaker’s honoraria from Amgen, JMR, BN,BS - Speaker’s honoraria from Roche, BS - Speaker’s honoraria from Servier, MLN,BN,JMR,EG,ES,BS,MG - Travel sponsorship from Fresenius Medical Care, BS - Travel sponsorship from Servier, MLN, PJ, BM, MA,KK,RK,KC - employees of Fresenius Nephrocare Dialysis Units, MB declares that he has no conflict of interest
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study contains retrospective observational data. For this type of study formal consent is not required. Protocol of the study received approval from the Local Bioethics Committee.
Rights and permissions
About this article
Cite this article
Lichodziejewska-Niemierko, M., Chmielewski, M., Wojtaszek, E. et al. Current epidemiology and practice patterns in prevention and treatment of PD-related infections in Poland. Int Urol Nephrol 51, 335–341 (2019). https://doi.org/10.1007/s11255-018-2057-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-018-2057-9