Abstract
Introduction
Renal cell carcinoma (RCC) accounts for approximately 3% of adult malignancies and more than 90% of neoplasms arising from the kidney. Uninformative percutaneous kidney biopsies vary from 10 to 23%. As a result, 7.5–33.6% of partial nephrectomies in patients with small renal masses (SRM) are performed on benign renal tumors. The aim of this study was to assess the feasibility of the apparent diffusion coefficient (ADC) of the diffusion-weighted imaging (DWI) of MRI, as RCC imaging biomarker for differentiation of SRM.
Method
Adult patients (n = 158) with 170 SRM were enrolled into this study. The control group were healthy volunteers with normal clinical and radiologic findings (n = 15). All participants underwent MRI with DWI sequence included.
Results
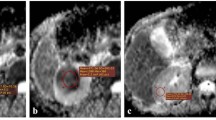
Mean ADC values of solid RCC (1.65 ± 0.38 × 10−3 mm2/s) were lower than healthy renal parenchyma (2.47 ± 0.12 × 10−3 mm2/s, p < 0.05). There was no difference between mean ADC values of ccRCC, pRCC and chRCC (1.82 ± 0.22 × 10−3 vs 1.61 ± 0.07 × 10−3 vs 1.46 ± 0.09 × 10−3 mm2/s, respectively, p = ns). An inverse relationship between mean ADC values and Fuhrman grade of nuclear atypia of solid ccRCCs was observed: grade I—1.92 ± 0.11 × 10−3 mm2/s, grade II—1.84 ± 0.14 × 10−3 mm2/s, grade III—1.79 ± 0.10 × 10−3 mm2/s, grade IV—1.72 ± 0.06 × 10−3 mm2/s. This was significant (p < 0.05) only between tumors of I and IV grades. Significant difference (p < 0.05) between mean ADC values of solid RCCs, benign renal tumors and renal cysts was observed (1.65 ± 0.38 × 10−3 vs 2.23 ± 0.18 × 10−3 vs 3.15 ± 0.51 × 10−3 mm2/s, respectively). In addition, there was a significant difference (p < 0.05) in mean ADC values between benign cysts and cystic RCC (3.36 ± 0.35 × 10−3 vs 2.83 ± 0.21 × 10−3 mm2/s, respectively).
Conclusion
ADC maps with b values of 0 and 800 s/mm2 can be used as an imaging biomarker, to differentiate benign SRM from malignant SRM. Using ADC value threshold of 1.75 × 10−3 mm2/s allows to differentiate solid RCC from solid benign kidney tumors with 91% sensitivity and 89% specificity; ADC value threshold of 2.96 × 10−3 mm2/s distinguishes cystic RCC from benign renal cysts with 90% sensitivity and 88% specificity. However, the possibility of differentiation between ccRCC histologic subtypes and grades, utilizing ADC values, is limited.


Similar content being viewed by others
References
Howlader N, Noone AM, Krapcho M, Miller D, Bishop K, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (2016) SEER cancer statistics review, 1975–2013, National Cancer Institute. Bethesda, MD, USA, based on November 2015 SEER data submission, posted to the SEER web site, April 2016. http://seer.cancer.gov/csr/1975_2013/
Gill IS, Aron M, Gervais DA, Jewett MA (2010) Clinical practice: small renal mass. N Engl J Med 362:624–634
Phé V, Yates DR, Renard-Penna R, Cussenot O, Rouprêt M (2012) Is there a contemporary role for percutaneous needle biopsy in the era of small renal masses? BJU Int 109:867–872
Jeon HG, Seo SI, Jeong BC, Jeon SS, Lee HM, Choi HY, Song C, Hong JH, Kim CS, Ahn H, Jeong IG (2016) Percutaneous kidney biopsy for a small renal mass: a critical appraisal of results. J Urol 195:568–573
Volpe A, Terrone C, Scarpa RM (2009) The current role of percutaneous needle biopsies of renal tumours. Arch Ital Urol Androl 81:107–112
Menogue SR, O’Brien BA, Brown AL, Cohen RJ (2013) Percutaneous core biopsy of small renal mass lesions: a diagnostic tool to better stratify patients for surgical intervention. BJU Int 111:E146–E151
Michael B, Prince J, Bultman E (2015) Predictors of non-diagnostic renal mass biopsy. J Urol 4:532–533
Link RE, Bhayani SB, Allaf ME, Varkarakis I, Inagaki T, Rogers C, Su LM, Jarrett TW, Kavoussi LR (2005) Exploring the learning curve, pathological outcomes and perioperative morbidity of laparoscopic partial nephrectomy performed for renal mass. J Urol 173:1690–1694
Fananapazir G, Lamba R, Lewis B, Corwin MT, Naderi S, Troppmann C (2015) Utility of MRI in the characterization of indeterminate small renal lesions previously seen on screening CT scans of potential renal donor patients. AJR Am J Roentgenol 205:325–330
Baliyan V, Das CJ, Sharma S, Gupta AK (2014) Diffusion-weighted imaging in urinary tract lesions. Clin Radiol 69:773–782
Doğanay S, Kocakoç E, Ciçekçi M, Ağlamiş S, Akpolat N, Orhan I (2011) Ability and utility of diffusion-weighted MRI with different B values in the evaluation of benign and malignant renal lesions. Clin Radiol 66:420–425
Agnello F, Roy C, Bazille G, Galia M, Midiri M, Charles T, Lang H (2013) Small solid renal masses: characterization by diffusion-weighted MRI at 3 T. Clin Radiol 68:301–308
Baldewijns MM, Thijssen VL, Van den Eynden GG, Van Laere SJ, Bluekens AM, Roskams T, van Poppel H, De Bruïne AP, Griffioen AW, Vermeulen PB (2007) High-grade clear cell renal cell carcinoma has a higher angiogenic activity than low-grade renal cell carcinoma based on histomorphological quantification and qRT-PCR mRNA expression profile. Br J Cancer 96:1888–1895
Kuthi L, Jenei A, Hajdu A, Németh I, Varga Z, Bajory Z, Pajor L, Iványi B (2017) Prognostic factors for renal cell carcinoma subtypes diagnosed according to the 2016 WHO renal tumor classification: a study involving 928 patients. Pathol Oncol Res 23(689):698
Mytsyk Y, Dutka I, Borys Y, Komnatska I, Shatynska-Mytsyk I, Farooqi AA, Gazdikova K, Caprnda M, Rodrigo L, Kruzliak P (2017) Renal cell carcinoma: applicability of the apparent coefficient of the diffusion-weighted estimated by MRI for improving their differential diagnosis, histologic subtyping, and differentiation grade. Int Urol Nephrol 49:215–224
Ponhold L, Javor D, Heinz-Peer G, Sevcenco S, Hofstetter M, Baltzer PA (2016) Inter-observer variation and diagnostic efficacy of apparent diffusion coefficient (ADC) measurements obtained by diffusion-weighted imaging (DWI) in small renal masses. Acta Radiol 57:1014–1020
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Mytsyk, Y., Dutka, I., Yuriy, B. et al. Differential diagnosis of the small renal masses: role of the apparent diffusion coefficient of the diffusion-weighted MRI. Int Urol Nephrol 50, 197–204 (2018). https://doi.org/10.1007/s11255-017-1761-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-017-1761-1